Stem cell therapy has emerged as a promising avenue in the field of regenerative medicine, offering potential treatments for a wide range of diseases and injuries. Stem cell transplants, in particular, have gained significant attention due to their ability to replace or repair damaged cells and tissues. However, not all stem cell transplants are the same. There are various types of stem cell transplants, each with its own unique characteristics and applications. In this comprehensive guide, we will explore the different types of stem cell transplants, their methodologies, and their clinical uses.
Understanding Stem Cells
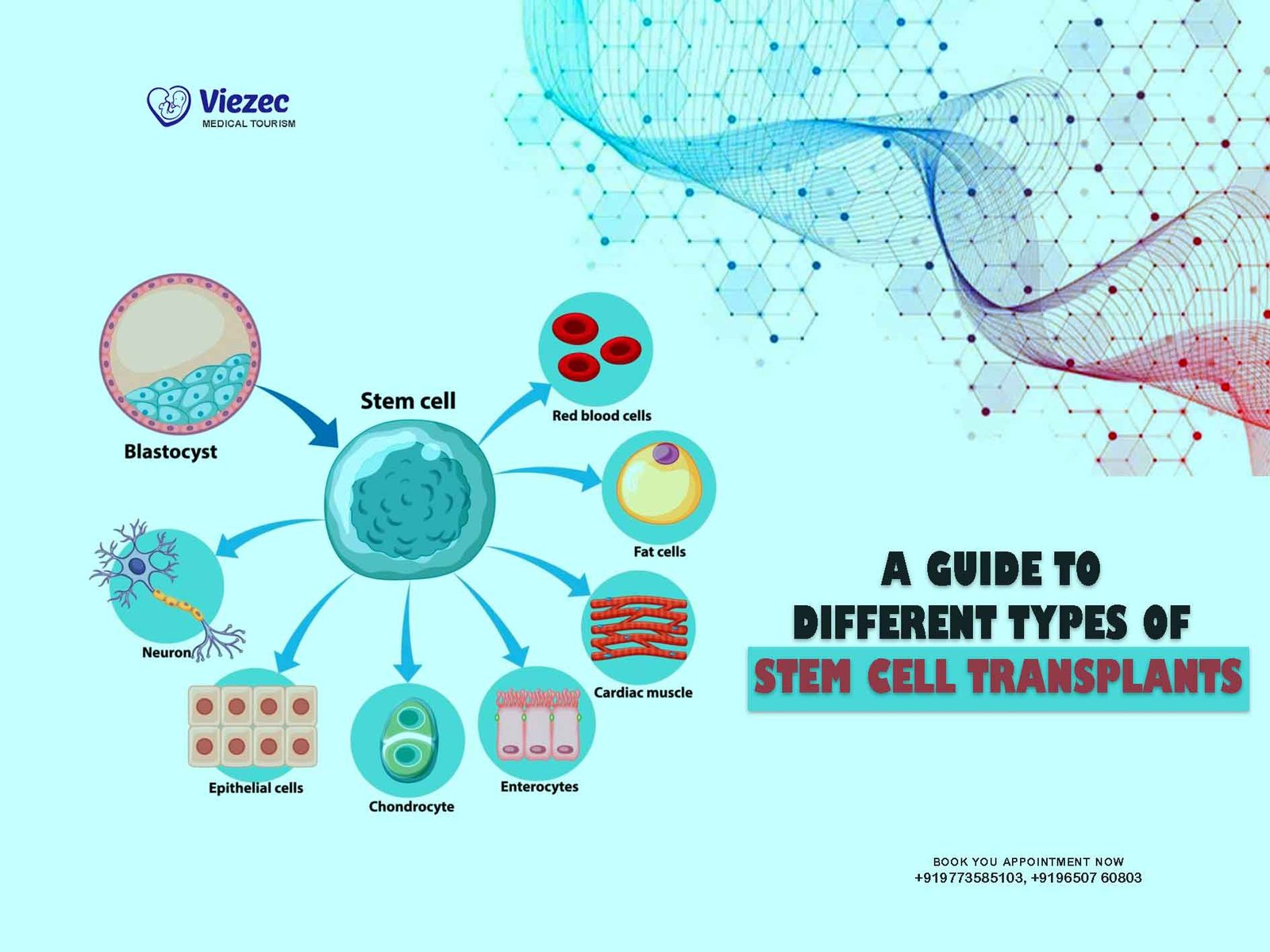
Before delving into the types of stem cell transplants, it’s essential to grasp the fundamentals of stem cells themselves. Stem cells are undifferentiated cells that have the remarkable ability to differentiate into various specialized cell types. They serve as the body’s natural repair system, replenishing cells in tissues and organs throughout life.
There are two primary types of stem cells:
1. Embryonic Stem Cells (ESCs)
Embryonic stem cells are derived from the inner cell mass of blastocysts, which are early-stage embryos. These cells are pluripotent, meaning they can differentiate into any cell type in the body. Due to their potency and ability to proliferate indefinitely in culture, ESCs hold immense potential for regenerative medicine.
2. Adult Stem Cells
Adult stem cells, also known as somatic or tissue-specific stem cells, exist in various tissues and organs throughout the body. Unlike ESCs, adult stem cells are multipotent or sometimes oligopotent, meaning they can differentiate into a limited range of cell types. Examples of adult stem cells include hematopoietic stem cells (found in the bone marrow) and mesenchymal stem cells (found in tissues such as bone marrow, adipose tissue, and umbilical cord blood).
Types of Stem Cell Transplants
Stem cell transplants, also known as hematopoietic stem cell transplants (HSCT) or bone marrow transplants, involve the infusion of stem cells into a patient to restore or replace damaged cells and tissues. These transplants are categorized based on the source of the stem cells and the relationship between the donor and the recipient. The main types of stem cell transplants include:
1. Autologous Stem Cell Transplantation
Autologous stem cell transplantation involves harvesting a patient’s own stem cells and reintroducing them after chemotherapy or radiation therapy. This type of transplant eliminates the risk of rejection or graft-versus-host disease (GVHD) because the patient’s immune system recognizes the transplanted cells as “self.”
Procedure:
- Stem Cell Collection: Prior to undergoing chemotherapy or radiation therapy, the patient’s stem cells are collected from either the bone marrow or peripheral blood using a process called apheresis.
- Conditioning Therapy: The patient receives high-dose chemotherapy or radiation therapy to eliminate cancer cells or malfunctioning cells.
- Stem Cell Infusion: After completing the conditioning therapy, the collected stem cells are infused back into the patient’s bloodstream through a vein, where they migrate to the bone marrow and begin to regenerate.
Clinical Applications:
- Autologous stem cell transplantation is commonly used in the treatment of cancers such as multiple myeloma, lymphoma, and certain types of leukemia.
- It can also be employed in autoimmune diseases like multiple sclerosis and systemic sclerosis.
2. Allogeneic Stem Cell Transplantation
Allogeneic stem cell transplantation involves transplanting stem cells from a compatible donor, typically a sibling or unrelated donor whose tissue type closely matches that of the recipient. Unlike autologous transplantation, allogeneic transplants carry the risk of graft rejection and GVHD, as the donor’s immune cells may recognize the recipient’s tissues as foreign.
Procedure:
- Donor Matching: Donor selection involves human leukocyte antigen (HLA) typing to identify a suitable donor with the closest HLA match to the recipient.
- Stem Cell Collection: Stem cells are obtained from the donor’s bone marrow, peripheral blood, or umbilical cord blood.
- Conditioning Therapy: Similar to autologous transplantation, the recipient undergoes high-dose chemotherapy or radiation therapy to eradicate diseased cells and suppress the immune system.
- Stem Cell Infusion: The donor stem cells are infused into the recipient’s bloodstream, where they engraft in the bone marrow and produce new blood cells.
Clinical Applications:
- Allogeneic stem cell transplantation is primarily used in the treatment of hematological malignancies such as leukemia, lymphoma, and myelodysplastic syndromes.
- It may also be indicated for certain non-malignant conditions like aplastic anemia and inherited metabolic disorders.
3. Syngeneic Stem Cell Transplantation
Syngeneic stem cell transplantation involves transplanting stem cells from an identical twin (monozygotic twin) to the recipient. Because identical twins share the same genetic makeup, there is no risk of rejection or GVHD in syngeneic transplants.
Procedure:
- Identical Twin Identification: The recipient must have an identical twin whose stem cells can be used for transplantation.
- Stem Cell Collection: Stem cells are harvested from the identical twin through bone marrow aspiration or peripheral blood collection.
- Conditioning Therapy: The recipient undergoes conditioning therapy with chemotherapy or radiation to prepare the body for transplantation.
- Stem Cell Infusion: The harvested stem cells are infused into the recipient’s bloodstream, where they home to the bone marrow and initiate hematopoiesis.
Clinical Applications:
- Syngeneic stem cell transplantation is primarily used in the treatment of hematologic malignancies and certain autoimmune diseases.
- It offers a unique advantage of reduced risk of graft rejection and GVHD compared to allogeneic transplants.
4. Umbilical Cord Blood Transplantation
Umbilical cord blood transplantation involves using stem cells derived from the blood of the umbilical cord and placenta following childbirth. Cord blood stem cells are naïve and immunologically immature, making them suitable for transplantation across HLA barriers with reduced risk of graft rejection and GVHD.
Procedure:
- Cord Blood Collection: After the birth of a baby, the umbilical cord and placenta are collected, and the cord blood is extracted.
- Cord Blood Banking: The cord blood is processed, tested, and cryopreserved in a cord blood bank for future use.
- Matching and Selection: When a patient requires a transplant, cord blood units are selected based on HLA matching criteria.
- Conditioning Therapy and Transplantation: The recipient undergoes conditioning therapy, followed by infusion of the selected cord blood unit.
Clinical Applications:
- Umbilical cord blood transplantation is utilized in the treatment of hematologic malignancies, genetic disorders, and certain metabolic disorders.
- It serves as a valuable source of stem cells for patients who lack suitable related or unrelated donors.
Stem cell transplantation represents a significant advancement in the treatment of various diseases and disorders, offering the potential for regeneration and repair at the cellular level. Each type of stem cell transplant has its own advantages, limitations, and clinical applications. Autologous transplantation harnesses the patient’s own stem cells to restore damaged tissues without the risk of rejection.