Understanding Diabetic Foot Ulcers
What Causes These Chronic Wounds?
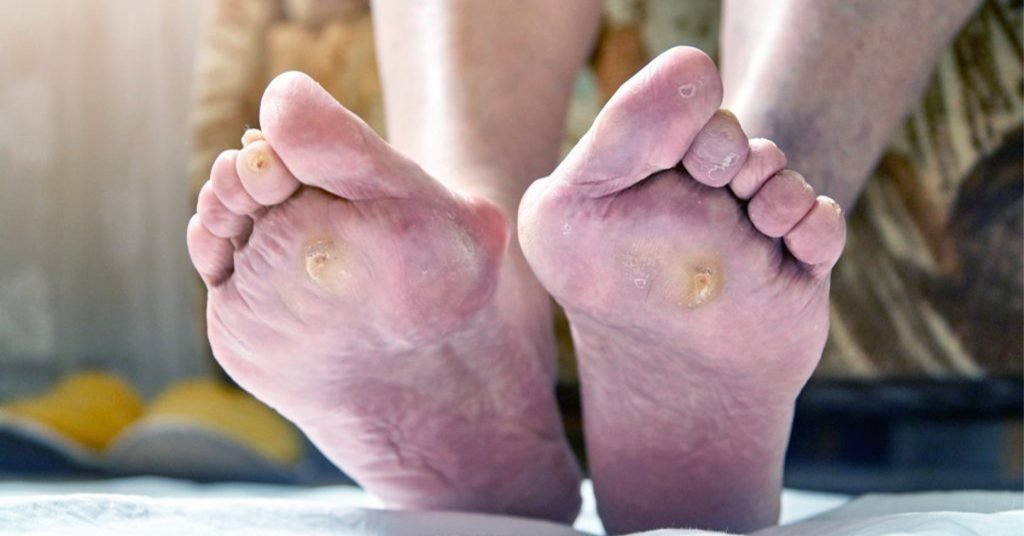
Diabetic foot ulcers are more than just surface-level wounds—they’re the result of deep-seated complications associated with diabetes. When blood sugar levels remain elevated over time, they can damage peripheral nerves (a condition known as diabetic neuropathy). This leads to reduced sensation in the feet, meaning that cuts, blisters, or pressure sores may go unnoticed.
At the same time, diabetes also affects blood vessels, restricting circulation and reducing the delivery of oxygen and nutrients to the tissues. With impaired immune function, even a small injury can spiral into a chronic, non-healing wound.
Why Are Diabetic Ulcers So Hard to Heal?
Diabetic ulcers are notoriously difficult to treat because they exist in an environment where the body’s natural healing mechanisms are disrupted. Chronic inflammation, poor blood flow, and tissue breakdown create a perfect storm for persistent wounds. On top of that, continuous pressure from walking and poorly fitting shoes, as well as frequent infections, slow down healing or prevent it entirely.
Many patients face months—or even years—of slow progress, and in severe cases, ulcers can lead to hospitalization or limb amputation. That’s why innovative solutions like exosome therapy are generating so much excitement.