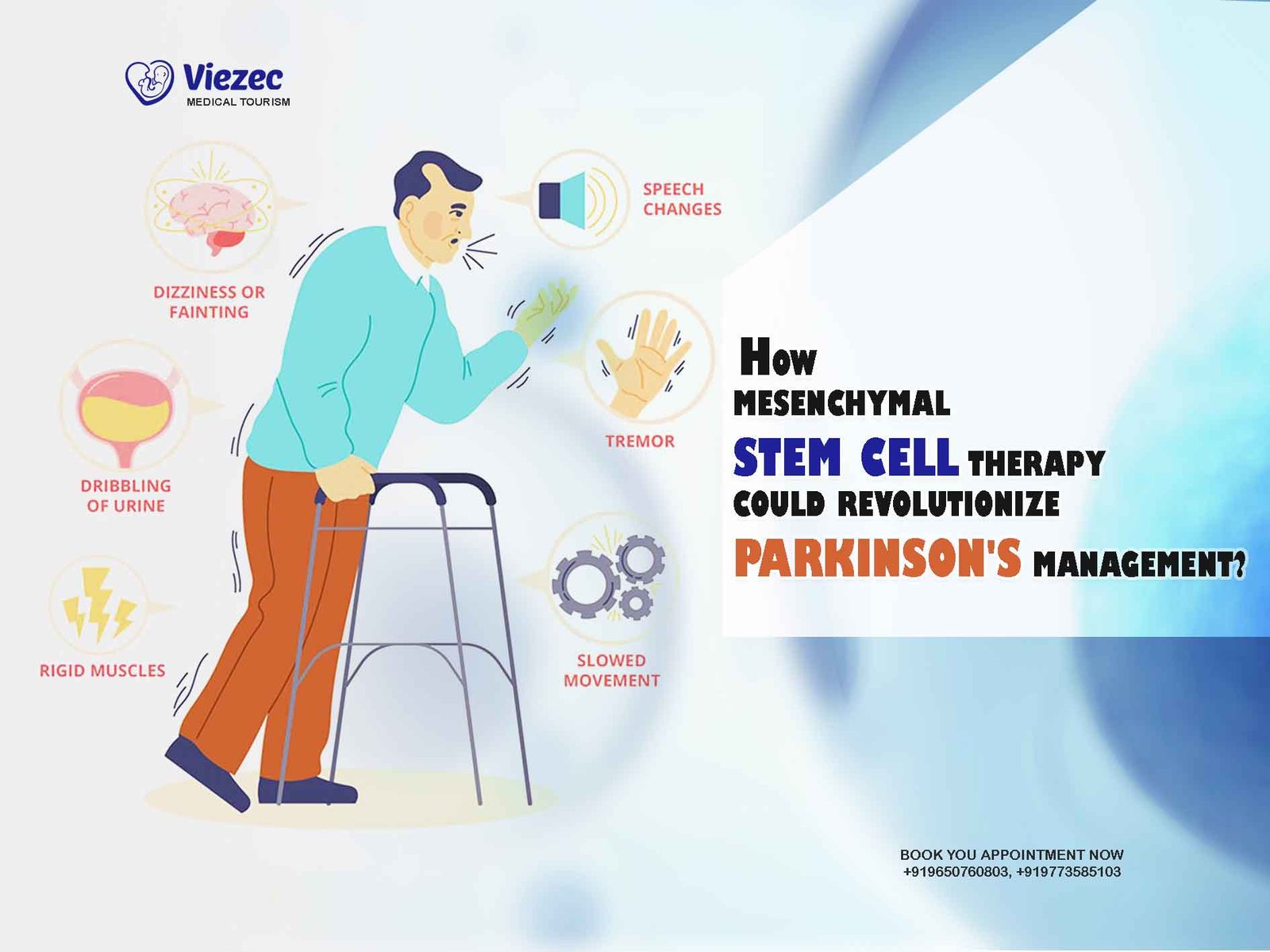
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by the loss of dopaminergic neurons in the substantia nigra region of the brain. This leads to a range of motor and non-motor symptoms, including tremors, rigidity, bradykinesia, and cognitive impairment. Despite significant advancements in pharmacological and surgical interventions, there remains an unmet need for therapies that can halt or reverse the underlying pathology of PD. Mesenchymal stem cell (MSC) therapy has emerged as a promising approach in this regard, offering the potential to not only alleviate symptoms but also to modify the course of the disease itself. In this article, we explore how MSC therapy could revolutionize the management of Parkinson’s disease.
Understanding Mesenchymal Stem Cells
What are Mesenchymal Stem Cells?
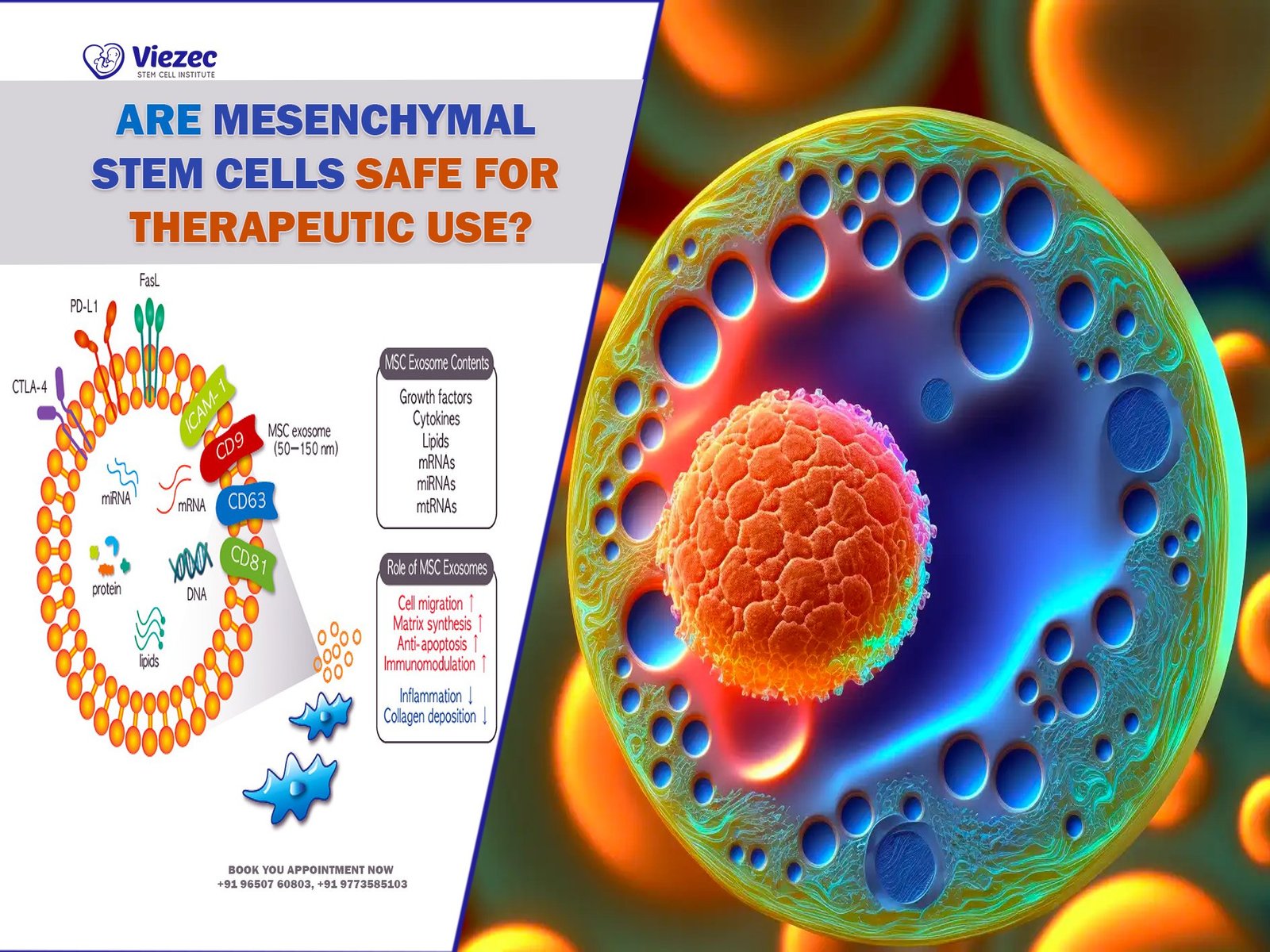
Mesenchymal stem cells are multipotent stromal cells that can differentiate into a variety of cell types, including osteoblasts, chondrocytes, adipocytes, and neural cells. They are primarily derived from various adult tissues, such as bone marrow, adipose tissue, umbilical cord blood, and dental pulp. One of the key properties of MSCs is their ability to modulate the immune response and promote tissue repair and regeneration through paracrine signaling mechanisms.
Mechanisms of Action
MSCs exert their therapeutic effects through multiple mechanisms, including:
- Immunomodulation: MSCs possess immunosuppressive properties that help dampen inflammatory responses and regulate immune cell activity, thereby reducing neuroinflammation and preserving neuronal function.
- Neuroprotection: MSCs secrete neurotrophic factors such as brain-derived neurotrophic factor (BDNF), glial cell line-derived neurotrophic factor (GDNF), and nerve growth factor (NGF), which promote the survival and growth of neurons and protect them from degeneration.
- Neurogenesis: MSCs have the capacity to differentiate into neural progenitor cells and integrate into damaged brain tissue, contributing to neuronal repair and regeneration.
- Synaptic Plasticity: MSCs can modulate synaptic activity and promote the formation of new neural connections, potentially restoring normal neuronal circuitry in the brain.
Plan Your Stem Cell Therapy Procedure in India
Promise of MSC Therapy for Parkinson’s Disease
Addressing Underlying Pathology
Conventional treatments for Parkinson’s disease primarily focus on symptom management through the enhancement of dopamine signaling or modulation of neuronal activity. While these approaches can provide symptomatic relief, they do not address the underlying neurodegenerative process. MSC therapy offers a novel approach by targeting the root cause of PD pathology, namely the loss of dopaminergic neurons and associated neuroinflammation.
Preclinical Evidence
Numerous preclinical studies have demonstrated the efficacy of MSC therapy in animal models of Parkinson’s disease. For example, intracerebral transplantation of MSCs has been shown to improve motor function, increase dopamine levels, and reduce neuroinflammation in rodent models of PD. These effects are thought to be mediated by the secretion of neurotrophic factors and the modulation of inflammatory cytokines by MSCs.
Clinical Trials
Building on the promising preclinical data, clinical trials have been initiated to evaluate the safety and efficacy of MSC therapy in Parkinson’s patients. Early-phase trials have shown encouraging results, with improvements in motor function, activities of daily living, and quality of life observed in some patients following MSC transplantation. Importantly, MSC therapy appears to be well-tolerated, with few adverse effects reported.
Mechanistic Insights
Recent studies have provided insights into the mechanisms underlying the therapeutic effects of MSCs in Parkinson’s disease. It is now recognized that MSCs exert their neuroprotective and regenerative effects not only through direct cell replacement but also through paracrine signaling and immunomodulation. By modulating the local microenvironment and promoting endogenous repair mechanisms, MSCs create a conducive environment for neuronal survival and regeneration.
Challenges and Considerations
Heterogeneity of MSC Populations
One of the challenges in MSC therapy is the heterogeneity of MSC populations derived from different tissue sources and donors. Variability in cell purity, potency, and immunomodulatory properties can impact the therapeutic outcomes and reproducibility of MSC-based interventions. Standardization of isolation and manufacturing protocols is essential to ensure the consistency and quality of MSC products for clinical use.
Optimal Delivery Route
The optimal route of administration for MSC therapy in Parkinson’s disease remains a subject of debate. While intracerebral transplantation offers direct access to the affected brain regions, it is invasive and carries the risk of surgical complications. Systemic delivery routes, such as intravenous or intra-arterial infusion, offer non-invasive alternatives but may result in lower cell engraftment and efficacy due to the blood-brain barrier.
Long-Term Safety and Efficacy
Long-term safety and efficacy data are still limited, particularly in the context of chronic neurodegenerative diseases like Parkinson’s. Questions remain regarding the durability of therapeutic effects, potential adverse events such as tumorigenesis or immune reactions, and the need for repeat dosing or maintenance therapy. Continued follow-up and surveillance are necessary to assess the long-term outcomes and risks associated with MSC therapy.
Future Directions
Optimization of MSC Products
Advancements in cell culture techniques, genetic engineering, and biomaterials are driving efforts to optimize MSC products for enhanced therapeutic efficacy and delivery. Strategies such as preconditioning MSCs with neurotrophic factors or genetic modification to enhance their survival, homing, and differentiation capacity are being explored to maximize their therapeutic potential in Parkinson’s disease.
Combination Therapies
Combining MSC therapy with other treatment modalities, such as pharmacotherapy, deep brain stimulation, or gene therapy, may offer synergistic benefits for Parkinson’s patients. Combinatorial approaches targeting multiple pathogenic pathways could potentially enhance neuroprotection, promote neuroregeneration, and improve clinical outcomes beyond what is achievable with monotherapy alone.
Personalized Medicine Approaches
Personalized medicine approaches, incorporating patient-specific factors such as disease stage, genetic profile, and comorbidities, could help tailor MSC therapy to individual needs and optimize treatment outcomes. Biomarker-based strategies for patient stratification and monitoring could enable more precise dosing and timing of interventions, ultimately leading to better therapeutic responses and prognosis.
Contact us for free online appointment
Make an informed Decision
Mesenchymal stem cell therapy holds tremendous promise for revolutionizing the management of Parkinson’s disease by addressing its underlying pathology and providing neuroprotective and regenerative effects. While challenges remain in terms of standardization, delivery optimization, and long-term safety, ongoing research efforts are advancing our understanding of MSC biology and refining therapeutic strategies. With continued innovation and clinical development, MSC therapy has the potential to transform the treatment paradigm for Parkinson’s disease and improve the lives of millions of patients worldwide.