Stress fractures are tiny cracks in bones, often caused by repetitive force or overuse, commonly affecting athletes, runners, and active individuals. These injuries typically occur in weight-bearing bones like the tibia, metatarsals, or femur. Unlike acute fractures, they develop gradually, making early detection tricky. Symptoms include localized pain, swelling, and tenderness that worsen with activity. Traditional treatments—rest, immobilization, and pain management—can take weeks or months, frustrating patients eager to resume normal life. Complications like delayed healing or chronic pain may arise if untreated. Regenerative medicine offers a promising alternative, harnessing the body’s natural healing processes to accelerate recovery and strengthen bones. This article explores how innovative therapies like stem cells, platelet-rich plasma (PRP), and growth factors transform stress fracture treatment, reducing downtime and enhancing long-term outcomes for patients.
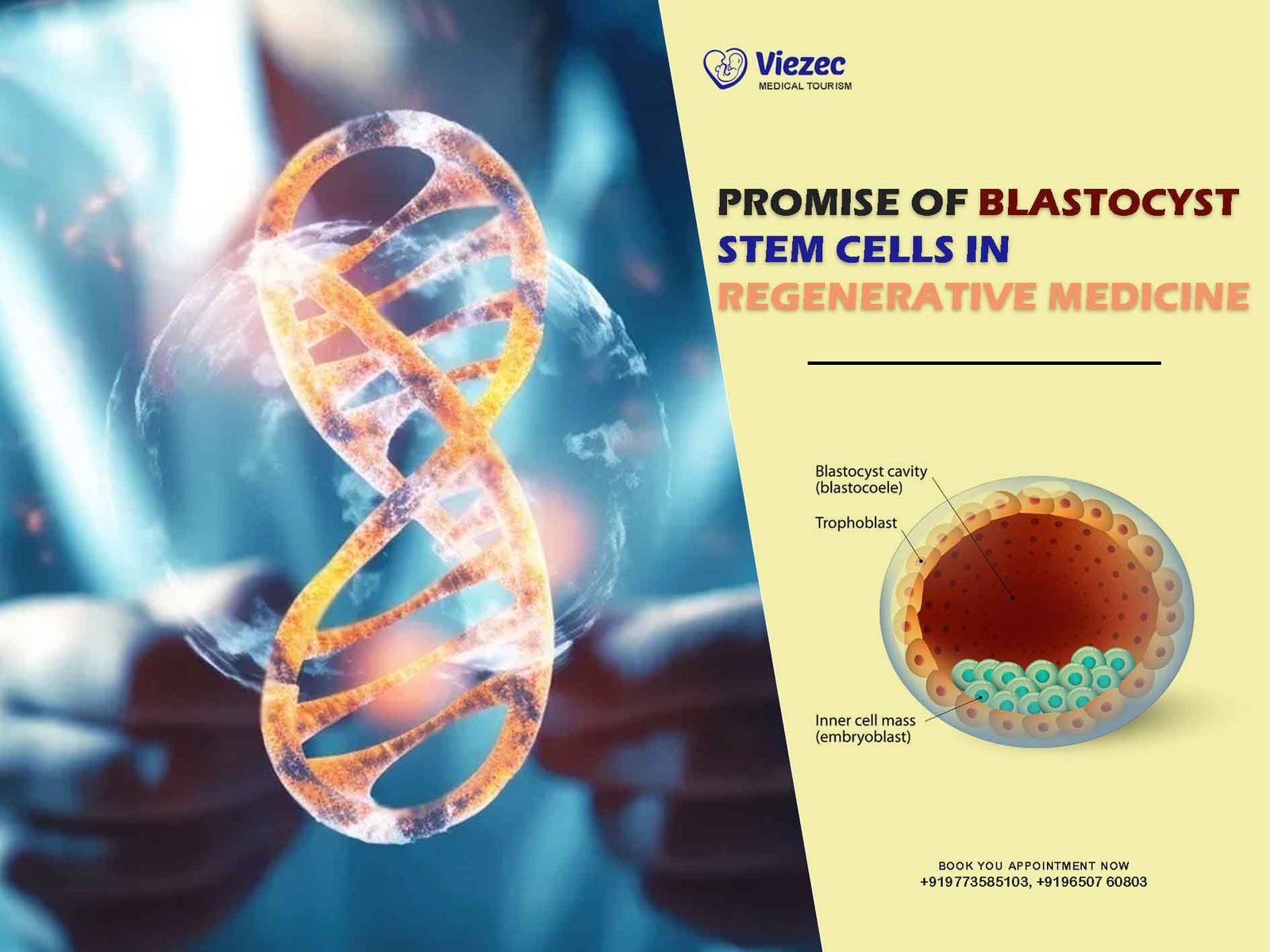
What Is Regenerative Medicine?
Regenerative medicine is a cutting-edge field focused on repairing, replacing, or regenerating damaged tissues and organs. Unlike conventional treatments that merely manage symptoms, it targets the root cause of injuries like stress fractures. It leverages the body’s own biological mechanisms—cells, proteins, and growth factors—to promote healing. Key approaches include stem cell therapy, PRP injections, and tissue engineering. For stress fractures, this means stimulating bone repair at a cellular level, rather than relying solely on rest or surgery. The goal is to restore function faster and more effectively. Scientists and clinicians see it as a game-changer, especially for injuries resistant to traditional care. By enhancing natural regeneration, these therapies reduce inflammation, boost blood flow, and encourage new bone formation. Patients benefit from shorter recovery times and potentially stronger bones, making regenerative medicine a beacon of hope for those sidelined by stress fractures.
The Science Behind Stress Fractures
Stress fractures result from cumulative microtrauma when bones can’t withstand repeated stress. Normally, bones adapt to pressure by remodeling—breaking down and rebuilding stronger—but excessive strain outpaces this process, causing tiny cracks. Risk factors include overtraining, poor footwear, nutritional deficiencies (like low calcium or vitamin D), and biomechanical issues. The lower leg, particularly the tibia and metatarsals, absorbs significant impact during activities like running, making it a common site. Initially, pain may be mild, but without rest, cracks deepen, impairing mobility. Bone healing involves inflammation, soft callus formation, and hard callus remodeling, a process that can stall under chronic stress. Regenerative medicine intervenes by amplifying these stages. It introduces bioactive agents that enhance cellular activity, speeding up repair and reducing the risk of re-injury. Understanding this science highlights why advanced therapies outperform traditional methods for stubborn fractures.
How Stem Cells Repair Bone Damage
Stem cells are the body’s master builders, capable of transforming into specialized cells like osteoblasts, which form bone. In stress fracture treatment, stem cells—often harvested from bone marrow or fat tissue—are injected into the injury site. There, they stimulate repair by differentiating into bone cells and releasing growth factors that signal surrounding tissues to heal. This dual action accelerates the formation of new bone and strengthens the fracture site. Studies show stem cell therapy can cut healing time significantly compared to rest alone, especially for high-demand patients like athletes. It also reduces inflammation, a key barrier to recovery. By targeting the fracture directly, stem cells address the underlying damage, not just the symptoms. While still evolving, this approach offers a personalized, biology-driven solution, minimizing reliance on invasive procedures and paving the way for faster, more resilient recoveries.
Platelet-Rich Plasma (PRP): A Natural Booster
Platelet-rich plasma (PRP) therapy uses a patient’s own blood to supercharge healing. Blood is drawn, spun in a centrifuge to concentrate platelets, and injected into the stress fracture site. Platelets release growth factors—proteins that promote tissue repair, reduce inflammation, and enhance blood flow. For stress fractures, PRP jumpstarts the body’s repair process, encouraging osteoblast activity and collagen production, essential for bone strength. It’s minimally invasive, with little downtime, making it ideal for active individuals. Research suggests PRP can shorten recovery by weeks, especially in early-stage fractures. Patients often report less pain and faster return to activity compared to traditional methods. Since it’s derived from the patient’s body, risks like rejection are negligible. PRP’s simplicity and effectiveness make it a cornerstone of regenerative medicine, offering a natural, potent tool to mend stress fractures and restore mobility with precision.
Growth Factors and Their Role in Healing
Growth factors are proteins that orchestrate tissue repair, acting as chemical messengers to stimulate cell growth and division. In stress fractures, key players like bone morphogenetic proteins (BMPs) and vascular endothelial growth factor (VEGF) are critical. BMPs trigger bone formation by activating osteoblasts, while VEGF boosts blood vessel growth, delivering oxygen and nutrients to the injury. Regenerative medicine amplifies these natural signals, often delivering concentrated growth factors via injections or scaffolds. This speeds up the transition from soft to hard callus, the stages where bone solidifies. For slow-healing stress fractures, this targeted boost can be transformative, reducing recovery time and preventing complications like nonunion. Clinical trials show promise, with patients experiencing less pain and stronger repairs. By mimicking and enhancing the body’s own processes, growth factors bridge the gap between injury and recovery, making them vital in modern fracture care.
Comparing Regenerative Medicine to Traditional Treatments
Traditional stress fracture treatments—rest, bracing, and sometimes surgery—focus on immobilization and symptom relief. Rest allows natural healing, but it’s slow, often taking 6-12 weeks, and risks muscle atrophy or re-injury. Surgery, used for severe cases, involves hardware like screws, adding recovery time and infection risks. Regenerative medicine, by contrast, actively repairs damage. Stem cells, PRP, and growth factors accelerate bone regeneration, often halving downtime. They also address inflammation and poor blood supply, common hurdles in healing. While traditional methods are passive, regenerative approaches are proactive, rebuilding tissue rather than waiting it out. Cost and accessibility remain challenges, but outcomes—faster recovery, less pain, and stronger bones—favor regenerative options, especially for athletes or chronic cases. As research advances, this shift promises to redefine how we treat stress fractures, blending science with the body’s innate resilience.
Who Benefits Most from Regenerative Treatments?
Regenerative medicine shines for specific groups plagued by stress fractures. Athletes, whose rigorous schedules demand quick recovery, top the list—runners, dancers, and basketball players often face repetitive bone stress. Military personnel, enduring prolonged physical strain, also benefit, as do older adults with slower natural healing due to age-related declines in cell function. Patients with poor bone density, like those with osteoporosis, find regenerative therapies strengthen fractures beyond baseline. Individuals with delayed healing or nonunion fractures—where bones fail to mend—see dramatic improvements, avoiding surgery. Even weekend warriors pushing their limits can sidestep long layoffs. The ideal candidate values speed, strength, and minimal invasiveness. While not yet universal due to cost or availability, those with access and a need for rapid, robust recovery stand to gain the most, transforming how they rebound from these nagging injuries.
The Procedure: What to Expect
Regenerative treatments for stress fractures are straightforward but precise. First, a doctor assesses the fracture via imaging (X-ray or MRI) to pinpoint damage. For stem cell therapy, cells are harvested—often from bone marrow or fat—under local anesthesia, then prepared and injected into the fracture site. PRP involves a blood draw, centrifugation to concentrate platelets, and injection, typically in one visit. Both are outpatient procedures, lasting 1-2 hours, with minimal discomfort. Patients may feel mild soreness post-injection, but there’s no lengthy immobilization. Activity resumes gradually, guided by a physician, often within days to weeks—far faster than traditional rest. Follow-ups monitor healing via imaging or symptom checks. Side effects are rare, thanks to the body’s own materials. This streamlined process, blending advanced tech with natural repair, offers a practical, patient-friendly path to mending stress fractures effectively.
Success Stories and Clinical Evidence
Real-world cases highlight regenerative medicine’s impact on stress fractures. A marathon runner, sidelined by a tibial stress fracture, returned to training in six weeks with PRP, half the usual time. A dancer with a metatarsal crack healed in a month using stem cells, avoiding surgery. Clinical studies back these anecdotes. A 2023 trial found PRP reduced healing time by 30% in athletes, while stem cell research shows faster callus formation in resistant fractures. Bone regeneration rates improve, with patients reporting less pain and better function. Nonunion cases, notoriously stubborn, often resolve without invasive fixes. While long-term data is still growing, early evidence points to higher success rates and lower recurrence compared to rest alone. These stories and stats underscore a shift: regenerative medicine isn’t just theory—it’s delivering tangible wins for those battling stress fractures.
Potential Risks and Limitations
Regenerative medicine isn’t flawless. Risks, though rare, include infection at injection sites, minor bleeding, or allergic reactions to anesthetics. Stem cell or PRP effectiveness can vary—some patients heal slower if underlying issues like malnutrition persist. Overuse post-treatment risks re-injury if patients push too soon. Costs are a hurdle; insurance often doesn’t cover these therapies, leaving patients paying hundreds to thousands out-of-pocket. Availability lags too—specialized clinics aren’t everywhere, and expertise varies. Research, while promising, lacks decades-long studies to confirm durability or rare side effects. For some, traditional rest remains sufficient, making regenerative options overkill. Patient selection matters; those with severe comorbidities may not respond as well. Still, for many, benefits outweigh drawbacks. As technology matures, refining protocols and reducing costs could address these limits, broadening access to this transformative approach for stress fractures.
Integrating Regenerative Medicine into Everyday Care
Bringing regenerative medicine to routine stress fracture treatment hinges on accessibility and education. Clinics need trained specialists and equipment, which urban centers currently dominate—rural areas lag. Physicians must integrate it with staples like physical therapy, ensuring a holistic approach; PRP might speed bone repair, but rehab rebuilds strength. Patient awareness is key—many don’t know these options exist beyond elite sports. Protocols blending rest with injections could become standard, tailored to fracture severity and lifestyle. Insurance adoption would accelerate this, as would streamlined training for doctors. Mobile units or telemedicine consults could extend reach. Success requires collaboration—orthopedists, researchers, and policymakers aligning to normalize these therapies. For patients, it’s a seamless shift: a doctor’s visit, a quick procedure, and faster healing. As infrastructure grows, regenerative medicine could move from cutting-edge to commonplace, reshaping how we tackle stress fractures daily.
A New Era for Bone Healing
Regenerative medicine marks a turning point for stress fractures, shifting from passive recovery to active repair. Stem cells, PRP, and growth factors don’t just mend bones—they enhance them, cutting healing time and boosting resilience. Athletes reclaim their stride, workers return sooner, and chronic sufferers find relief where traditional methods faltered. Evidence mounts, with success stories and studies proving its edge over rest or surgery. Challenges like cost and access remain, but the trajectory is clear: as research refines techniques and infrastructure expands, these therapies will become mainstream. The body’s own healing power, amplified by science, offers a future where stress fractures lose their sting. Patients gain not just recovery, but empowerment—less downtime, less pain, and a stronger foundation. This isn’t just treatment; it’s a revolution in bone health, promising a new standard for injury care.