Stem cell therapy is revolutionizing the way we approach immune health. By harnessing the regenerative power of stem cells, researchers and clinicians are uncovering new ways to treat immune-related conditions, reduce inflammation, and support the body’s natural defenses. This article dives into the science, applications, and future of how stem cell therapy enhances immune function.
A Closer Look at the Immune System
How the Immune System Defends the Body
Your immune system is your body’s natural shield—designed to detect, fight, and eliminate anything that poses a threat, from bacteria and viruses to toxins and mutated cells. It’s made up of a dynamic network of cells, tissues, and signaling pathways that coordinate to protect you every moment of the day.
This defense system has two powerful branches:
-
Innate immunity acts as the first responder. It kicks in quickly and fights off invaders using general tactics like inflammation and phagocytosis (where immune cells engulf threats).
-
Adaptive immunity takes a more targeted approach. It learns from past encounters and produces highly specific antibodies and memory cells, helping your body react faster and more effectively to known invaders in the future.
Together, these two arms form a powerful team—responding to immediate threats and building long-term immunity.
What Happens When Immunity Breaks Down
When the immune system becomes unbalanced, the consequences can be serious—and sometimes life-altering.
-
A weakened immune system struggles to respond to infections or cancer cells, making you more vulnerable to illness.
-
An overactive immune system, on the other hand, may start attacking the body itself, mistaking healthy tissues as threats. This is the root of autoimmune diseases like lupus, multiple sclerosis, and rheumatoid arthritis.
-
And when chronic inflammation sets in—often due to a misregulated immune response—it can quietly damage tissues over time and contribute to heart disease, diabetes, and neurodegenerative conditions.
Maintaining immune balance isn’t just about staying infection-free. It’s about protecting every system in your body and preserving long-term health. This is where stem cell therapy begins to show promise—not just by treating symptoms, but by helping restore that critical balance.
What Are Stem Cells and Why Do They Matter?
The Unique Role of Stem Cells in Regeneration
Stem cells are unlike any other cells in the body—they’re the architects of healing and regeneration. What makes them special is their ability to transform into different types of specialized cells, like immune cells, nerve cells, or muscle tissue. Even more impressive, they can replicate themselves, creating fresh new cells when the body needs repair.
This regenerative power is exactly why they’re being explored in immune therapy. When stem cells are introduced into the body, they don’t just replace damaged tissue—they can also help regulate immune activity, calm inflammation, and promote balance throughout the immune system. Traditional treatments often suppress the immune response or treat symptoms. Stem cell therapy, by contrast, aims to restore healthy function from the inside out.
Types of Stem Cells Used in Immune Therapy
Not all stem cells are created equal. Different types are used in various therapeutic applications, each with unique properties and potential.
Mesenchymal Stem Cells (MSCs)
MSCs are perhaps the most widely studied in immune-related treatments. Found in bone marrow, fat tissue, and umbilical cord tissue, these stem cells have strong anti-inflammatory and immunomodulatory effects. They can help quiet an overactive immune system, reduce inflammatory cytokines, and encourage healing in damaged tissues. MSCs are currently being researched and used in clinical trials for conditions like rheumatoid arthritis, lupus, and even COVID-19–related inflammation.
Hematopoietic Stem Cells (HSCs)
HSCs are the foundation of your blood and immune system. These stem cells give rise to all types of blood cells, including white blood cells that are critical for immune defense. HSCs are commonly used in bone marrow transplants, particularly for cancer patients whose immune systems have been damaged by chemotherapy or radiation. They’re also used in severe autoimmune conditions, where “resetting” the immune system can lead to remission.
Induced Pluripotent Stem Cells (iPSCs)
iPSCs represent one of the most exciting frontiers in regenerative medicine. These are adult cells (like skin or blood cells) that scientists reprogram to behave like embryonic stem cells—capable of becoming almost any type of cell in the body. The major benefit of iPSCs is that they can be custom-created from a patient’s own cells, reducing the risk of rejection. While still largely in the research phase for immune applications, iPSCs have the potential to revolutionize personalized therapies in the future.
How Stem Cells Interact with the Immune System
Immune Modulation and Anti-Inflammatory Effects
One of the most powerful attributes of stem cells—especially mesenchymal stem cells (MSCs)—is their ability to communicate with and influence the immune system. Rather than attacking pathogens or diseased cells directly, MSCs act more like immune conductors, orchestrating the activity of other immune cells.
They release signaling molecules, known as cytokines and growth factors, which help regulate immune responses. For example, if inflammation is too high, MSCs can calm it by:
-
Suppressing overactive T-cells
-
Encouraging the production of anti-inflammatory cytokines
-
Promoting the development of regulatory T-cells, which keep immune responses in check
This immunomodulatory effect makes stem cell therapy especially promising for conditions where the immune system is in overdrive, like autoimmune diseases and chronic inflammatory disorders.
Reprogramming Overactive or Damaged Immune Responses
Stem cells don’t just manage inflammation—they can actually help reprogram the immune system. In cases of autoimmunity, the body mistakenly attacks its own tissues. MSCs can help “re-educate” the immune system, promoting immune tolerance and reducing these misguided attacks.
In patients recovering from serious infections, cancer treatments, or immune deficiencies, stem cells may help rebuild immune memory, strengthen weak defenses, and support the restoration of normal immune surveillance.
Think of them as a system reset—aiming not to suppress, but to restore immune function to a healthier, more balanced state.
Stem Cell Therapy in Autoimmune Disorders
Targeting the Root Cause of Autoimmunity
Autoimmune diseases develop when the immune system turns against the body’s own tissues, mistakenly identifying them as foreign threats. Traditional treatments—like immunosuppressants—can help control symptoms, but they often come with side effects and do not address the underlying immune dysfunction.
This is where stem cell therapy shines. Instead of broadly suppressing the immune system, stem cells help restore immune balance. They target the root problem by:
-
Calming hyperactive immune cells
-
Promoting immune tolerance, so the body stops attacking itself
-
Reducing inflammation and supporting tissue repair in affected areas
By modulating immune activity rather than simply shutting it down, stem cell therapy offers a more targeted, sustainable solution for autoimmune conditions.
Rheumatoid Arthritis, Lupus, and MS
Rheumatoid Arthritis (RA):
RA is driven by chronic inflammation that damages joints. MSCs have shown promise in reducing inflammation, alleviating pain, and even slowing joint deterioration by calming immune activity and promoting tissue repair.
Lupus (Systemic Lupus Erythematosus):
In lupus, the immune system attacks multiple organs and tissues. Clinical studies have shown that stem cell infusions—particularly MSCs—can reduce disease activity, improve kidney function, and decrease reliance on corticosteroids or immunosuppressants.
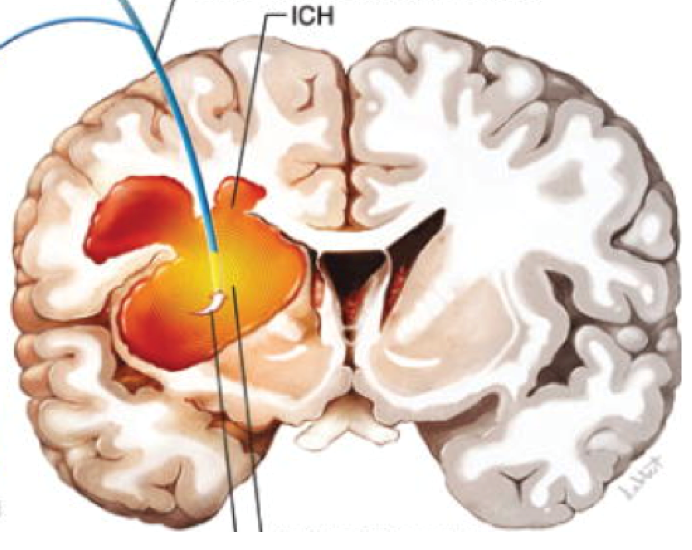
Multiple Sclerosis (MS):
MS is an autoimmune disease that targets the central nervous system, damaging the protective covering of nerves. Stem cell therapy offers twofold benefits:
-
Immune modulation to prevent further attacks on nerve tissue
-
Neuroregeneration to potentially repair myelin and restore function
Enhancing Immune Recovery in Cancer Patients
Restoring Immunity After Chemotherapy or Radiation
Cancer treatments like chemotherapy and radiation are designed to destroy rapidly dividing cancer cells—but unfortunately, they also harm healthy immune cells in the process. This often leaves patients with severely weakened immune systems, making recovery more difficult and increasing the risk of infections and complications.
Stem cell therapy—especially with hematopoietic stem cells (HSCs)—is a proven way to rebuild the immune system after these treatments. In fact, HSC transplants (commonly known as bone marrow transplants) are already a standard part of care for patients with leukemia, lymphoma, and other blood cancers.
Here’s how it works:
-
After chemotherapy or radiation has cleared out the diseased immune cells, HSCs are transplanted to regrow a new, healthy immune system from scratch.
-
These new cells develop into all the key components of immunity, including white blood cells, T-cells, and B-cells.
For many cancer patients, this is more than just recovery—it’s a second chance at a fully functional immune system.
Stem Cells and Cancer Immunotherapy Synergy
Stem cell therapy isn’t just used to replace immune cells after treatment—it’s also being explored as a way to enhance the effectiveness of cancer immunotherapy.
Emerging research suggests that certain stem cells can:
-
Improve immune recognition of cancer cells, making immunotherapy more effective
-
Repair damaged tissues post-treatment, aiding in faster recovery
-
Reduce treatment-related inflammation, improving quality of life
For example, combining MSCs with checkpoint inhibitors or CAR-T cell therapy may offer a synergistic effect—strengthening the immune attack on cancer while minimizing side effects.
Controlling Chronic Inflammation with Stem Cells
Inflammatory Cytokine Suppression
Chronic inflammation is like a slow-burning fire in the body—subtle at first, but over time, it can damage tissues and fuel serious diseases such as arthritis, heart disease, diabetes, and even neurodegenerative conditions. One of the key drivers of this process is a group of proteins called pro-inflammatory cytokines.
This is where mesenchymal stem cells (MSCs) show tremendous potential. These stem cells secrete anti-inflammatory cytokines and other regulatory molecules that can suppress harmful immune responses. Studies have shown that MSCs can:
-
Decrease levels of tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6)—two major inflammatory cytokines
-
Inhibit the activation of overzealous T-cells and macrophages
-
Promote the production of IL-10, a cytokine that calms inflammation
By dialing down the inflammatory response without shutting the immune system off entirely, stem cells provide a more balanced and natural way to manage chronic inflammation.
Restoring Balance in the Immune Environment
The immune system thrives on balance—a steady rhythm between activation and resolution. Inflammation is a natural and necessary part of healing, but when the body loses its ability to regulate it, problems arise.
Stem cells help restore what scientists call immune homeostasis. This means:
-
Calming the “alarm signals” that keep the immune system in a constant state of alert
-
Encouraging repair and regeneration of damaged tissues
-
Supporting the transition from inflammation to healing
This balancing act has far-reaching effects. It not only improves symptoms in chronic inflammatory diseases but also creates a healthier internal environment where the immune system can respond appropriately to real threats.
Clinical Evidence and Success Stories
What Current Research Shows
Over the past decade, research into stem cell therapy and immune health has grown exponentially. Numerous preclinical studies and clinical trials have shown that stem cells—particularly mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs)—can effectively modulate the immune system, reduce inflammation, and support tissue repair.
Highlights from the research include:
-
Autoimmune diseases: Studies show that MSC therapy can significantly reduce symptoms in patients with rheumatoid arthritis, lupus, and multiple sclerosis, often with fewer side effects than conventional treatments.
-
Post-COVID recovery: Trials suggest MSCs may reduce lung inflammation and improve immune recovery in patients with long COVID.
-
Graft-vs-host disease (GVHD): MSCs have been used successfully to treat this serious complication in bone marrow transplant recipients by calming immune overreactions.
While more large-scale, long-term studies are still needed, the early results are both promising and encouraging, pointing toward stem cells as a safe, viable complement or alternative to current immune therapies.
Stem Cell Therapy vs. Conventional Immune Treatments
Key Differences in Approach
When it comes to treating immune-related conditions, traditional medicine and stem cell therapy often take very different paths.
Conventional treatments—like corticosteroids, immunosuppressants, and biologics—focus on suppressing or controlling symptoms. They can be effective in reducing inflammation or halting disease progression, but they don’t typically address the root causes of immune dysfunction. Plus, long-term use can come with side effects such as:
-
Increased risk of infections
-
Organ strain (especially liver and kidneys)
-
Hormonal imbalances or bone loss
Stem cell therapy, on the other hand, is regenerative in nature. Instead of shutting down immune responses, it works to rebalance and rebuild the immune system. Stem cells help regulate overactive immune responses, calm inflammation, and promote healing at a cellular level—essentially encouraging the body to correct its own dysfunction.
Rather than simply putting out fires, stem cell therapy aims to retrain the immune system to function properly again.
Long-Term Benefits vs. Temporary Relief
One of the most exciting aspects of stem cell therapy is its potential for long-lasting results. While conventional treatments may require ongoing medication or injections, stem cell therapy often works with just a few treatments—sometimes even a single infusion.
Here’s what sets stem cells apart:
-
Durability: Many patients report improvements that last for months or even years
-
Fewer side effects: Especially with MSCs, the risk profile is low compared to chronic drug use
-
Whole-body benefits: Stem cells can help heal more than one area at a time, such as joints, immune cells, and internal organs affected by chronic inflammation
That said, stem cell therapy isn’t a universal replacement for conventional care—yet. It’s most powerful as part of a personalized, integrative approach, especially for patients who haven’t responded well to standard treatments or want to minimize medication reliance.
Who Can Benefit From Immune-Enhancing Stem Cell Therapy?
Ideal Candidates
Stem cell therapy isn’t just for the critically ill—it’s becoming an option for a growing number of people dealing with immune-related conditions. Ideal candidates typically include individuals who:
-
Have autoimmune diseases like rheumatoid arthritis, lupus, or multiple sclerosis
-
Are recovering from cancer treatments that weakened their immune systems
-
Suffer from chronic inflammatory conditions, such as Crohn’s disease, ulcerative colitis, or chronic fatigue syndrome
-
Experience immune deficiencies that leave them prone to frequent infections
-
Have not responded well to conventional treatments, or are seeking alternatives to long-term medication use
Stem cell therapy may also be a promising option for patients dealing with emerging post-viral syndromes (like long COVID), where the immune system remains out of balance long after the initial infection has passed.
That said, candidacy depends on several factors, including age, overall health, and the specific type of stem cell treatment being considered. A thorough medical evaluation is essential to determine the best fit.
When to Consider This Option
While stem cell therapy is still gaining traction in mainstream medicine, many people are turning to it when:
-
Conventional therapies aren’t working or cause side effects that disrupt daily life
-
They’re looking for a more natural, root-cause approach to healing
-
Their goal is to reduce reliance on medications and improve long-term health outcomes
-
They want to support immune recovery after illness or major treatments like chemotherapy
Early intervention often leads to better results, especially for autoimmune conditions or inflammatory diseases. However, some of the most remarkable outcomes have come from cases where traditional medicine had run out of options—making stem cell therapy a beacon of hope for those who’ve struggled for years.
Supporting Your Immune Health After Treatment
Lifestyle Tips to Maximize Results
Stem cell therapy doesn’t end after the last infusion—what you do afterward plays a big role in maintaining and enhancing the benefits. Think of your treatment as a reset button. Now it’s up to you to create the conditions that allow your immune system to thrive.
Here are key lifestyle practices that can support immune balance after therapy:
-
Stay physically active – Regular, moderate exercise boosts circulation, reduces inflammation, and supports immune cell function. Aim for daily movement, even if it’s just a brisk walk.
-
Get quality sleep – Your body heals during deep sleep. Try to get 7–9 hours of uninterrupted rest each night to promote recovery.
-
Manage stress – Chronic stress weakens immunity. Practices like deep breathing, meditation, yoga, or spending time in nature can help calm your nervous system.
-
Avoid toxins – Limit alcohol, tobacco, and exposure to harmful chemicals when possible. These can trigger inflammation and burden your immune system.
-
Stay hydrated – Water helps flush toxins and supports cellular health. Try to drink at least half your body weight in ounces of water daily.
These lifestyle shifts not only help you maintain results—they amplify the healing potential of stem cell therapy.
Nutritional and Supplement Recommendations
Food is one of your most powerful tools for immune support. A well-rounded, anti-inflammatory diet can help you get the most out of your stem cell therapy.
Here’s what to focus on:
-
Antioxidant-rich foods – Berries, leafy greens, nuts, and colorful vegetables help fight oxidative stress and support tissue repair.
-
Healthy fats – Omega-3s from sources like salmon, flaxseed, or walnuts reduce inflammation and support brain and immune function.
-
Probiotic and prebiotic foods – A healthy gut = a stronger immune system. Include yogurt, sauerkraut, kefir, and fiber-rich vegetables to nourish your gut microbiome.
-
Vitamin D – Often called the “immune vitamin,” D3 helps regulate immune responses. Many people are deficient, so supplementation may be helpful (always check with your doctor).
-
Other key nutrients – Zinc, vitamin C, magnesium, and quercetin all play important roles in immune function and recovery.
Choosing a Trustworthy Stem Cell Provider
What to Look for in a Reputable Clinic
As the interest in stem cell therapy rises globally, so does the number of clinics offering it—but not all providers meet the same safety and quality standards. Choosing the right clinic isn’t just about convenience or cost—it’s about ensuring your treatment is safe, ethical, and effective.
Here are essential factors to consider when selecting a stem cell provider:
-
Qualified medical team – Treatments should be overseen by licensed, board-certified physicians with experience in regenerative medicine, immunology, or a related specialty.
-
Transparent protocols and practices – A reputable provider clearly outlines the source of the stem cells (autologous or allogeneic), how they’re processed, how the procedure works, and realistic expectations for recovery.
-
Clean lab and clinical standards – The clinic should use facilities that follow Good Manufacturing Practices (GMP) or equivalent international lab standards to ensure the safety and quality of stem cells.
-
Regulatory compliance – In the U.S., clinics must follow FDA regulations, while international clinics should operate under their country’s regulatory framework. Clinical trials, IRB approvals, or recognized certifications add an extra layer of trust.
-
Patient reviews and case studies – Look for clinics that offer honest testimonials and publish treatment outcomes. Real-world success stories—especially for immune-related conditions—can be a helpful guide.
Stem Cell Treatment in India
One notable international provider is Viezec, based in India, which offers personalized stem cell therapy for a variety of conditions, including autoimmune disorders, neurological diseases, and chronic inflammation.
Viezec works with certified hospitals and research labs to deliver treatments that are based on rigorous safety protocols. The clinic uses mesenchymal stem cells derived from umbilical cord tissue, processed in GMP-compliant labs, and delivered by qualified healthcare professionals. Patients from around the world travel to India for treatment due to Viezec’s combination of affordability, advanced care, and personalized service.
If you’re considering medical travel, Viezec is an example of a clinic that blends international-standard care with the benefits of a cost-effective, transparent treatment experience.
Questions to Ask Before Starting Treatment
Before making any decisions, ask your prospective clinic the following questions:
-
What types of stem cells do you use, and where are they sourced?
-
Is the treatment part of an approved protocol or clinical trial?
-
What immune or inflammatory conditions have you treated successfully?
-
What are the potential risks or side effects based on my specific case?
-
How many patients with similar conditions have you treated?
-
What follow-up care or monitoring is included?
The more informed you are, the more empowered you’ll be to choose the right path for your health.