Multiple sclerosis (MS) is a chronic autoimmune disease characterized by the immune system’s misguided attack on the central nervous system (CNS). This results in inflammation, demyelination, and neurodegeneration, leading to a wide range of neurological symptoms and disabilities.
MS affects over 2.8 million people globally, with a higher prevalence in regions farther from the equator. While the exact cause remains elusive, genetic predisposition, environmental factors, and immune dysregulation are believed to contribute to its development.
Pathophysiology of MS
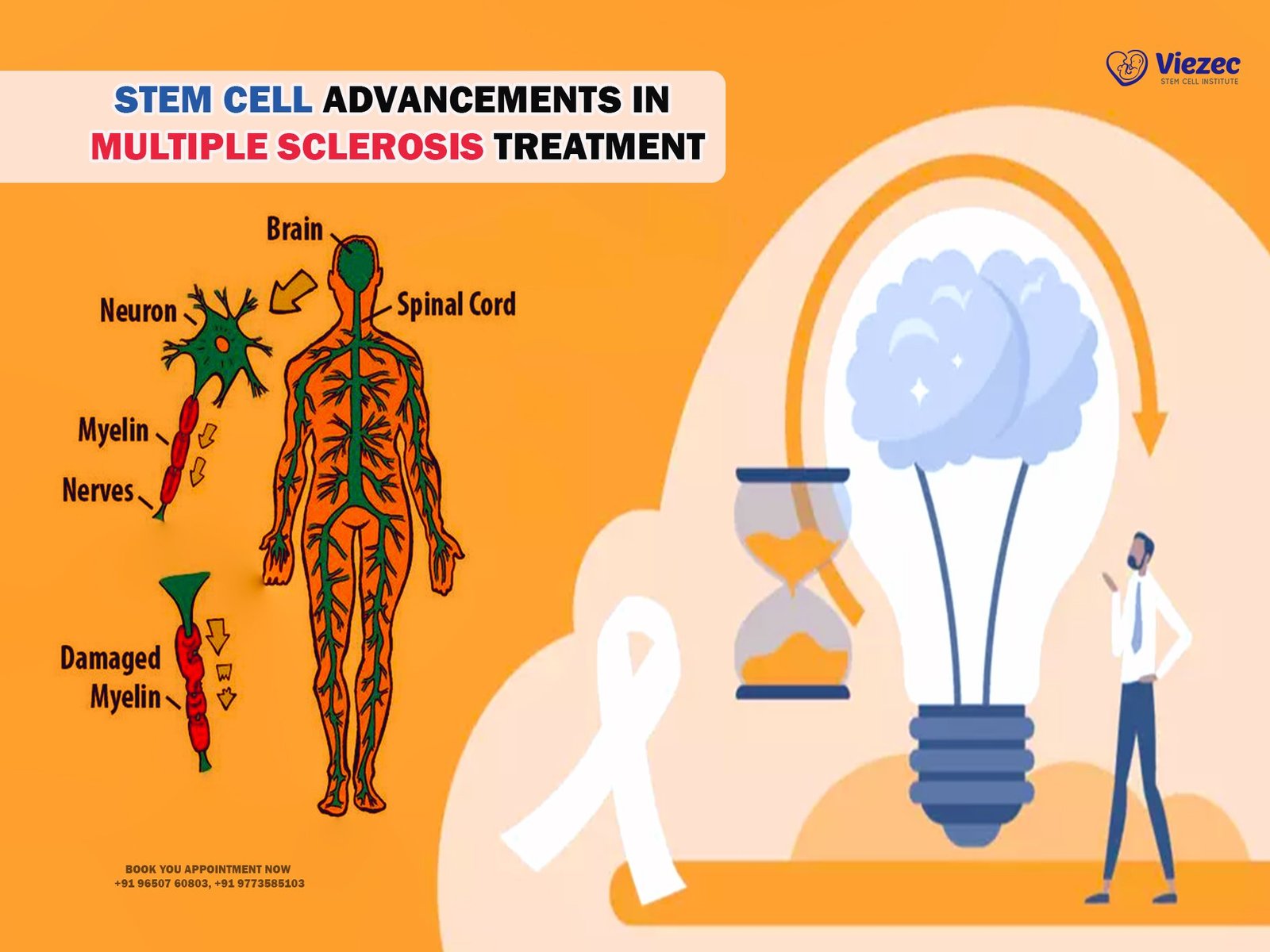
The pathophysiology of MS involves complex interactions between immune cells, cytokines, and the CNS. T cells infiltrate the CNS, triggering inflammation and attacking myelin, the protective sheath surrounding nerve fibers. This disrupts nerve signaling and leads to the formation of lesions in the brain and spinal cord.
Types of MS and Their Clinical Features
MS encompasses various clinical subtypes, including relapsing-remitting MS (RRMS), secondary progressive MS (SPMS), primary progressive MS (PPMS), and clinically isolated syndrome (CIS). Each subtype presents with distinct clinical features and disease trajectories, influencing treatment decisions.
Conventional Treatment Approaches
Disease-Modifying Therapies (DMTs)
Conventional treatment strategies for MS primarily focus on disease-modifying therapies (DMTs) aimed at reducing relapses, slowing disease progression, and preserving neurological function. These therapies include interferon-based drugs, oral immunomodulators, and monoclonal antibodies targeting specific immune pathways.
Interferon-Based Therapies
Interferon-based therapies, such as interferon beta-1a and beta-1b, have been a cornerstone in MS treatment for decades. They modulate immune responses, decrease inflammatory activity, and reduce relapse rates, albeit with varying efficacy and tolerability profiles.
Oral Immunomodulators
Oral immunomodulators, such as fingolimod and dimethyl fumarate, offer convenience and improved adherence compared to injectable therapies. They target sphingosine-1-phosphate receptors and immune cell trafficking, thereby reducing relapse rates and MRI lesion burden.
Monoclonal Antibodies
Monoclonal antibodies, including natalizumab and alemtuzumab, selectively target key immune cells or molecules involved in MS pathogenesis. By blocking lymphocyte migration into the CNS or depleting autoreactive lymphocytes, these agents effectively reduce relapse rates and disability progression.
Symptomatic Management
In addition to DMTs, symptomatic management plays a crucial role in improving quality of life for MS patients. Pharmacological interventions, rehabilitation strategies, and symptom-specific therapies address common symptoms such as fatigue, spasticity, pain, and cognitive impairment.
Pharmacological Interventions
Pharmacological interventions encompass a diverse range of medications targeting specific MS symptoms, including muscle relaxants, antidepressants, antispasmodics, and cognitive enhancers. These medications aim to alleviate symptoms and improve functional outcomes in daily activities.
Rehabilitation Strategies
Rehabilitation interventions, including physical therapy, occupational therapy, and speech therapy, focus on maximizing mobility, independence, and overall well-being in MS patients. These personalized programs address motor impairments, gait disturbances, and activities of daily living, enhancing functional capacity and quality of life.
Symptom-Specific Therapies
Symptom-specific therapies, such as bladder management strategies, cognitive rehabilitation, and pain management techniques, target individual symptoms based on their impact on daily functioning and quality of life. Multidisciplinary approaches involving healthcare professionals and allied health specialists optimize symptom management and holistic care delivery.
Emerging Therapeutic Paradigms
Role of Precision Medicine in MS Treatment
Precision medicine approaches aim to tailor treatment strategies based on individual patient characteristics, including genetic predisposition, immune profiles, and disease activity. By identifying biomarkers of treatment response and prognosis, personalized therapies hold promise in optimizing outcomes and minimizing treatment-related risks.
Immunomodulatory Strategies Beyond DMTs
Beyond conventional DMTs, emerging immunomodulatory strategies target novel immune pathways implicated in MS pathogenesis. These include B cell-targeted therapies, modulation of T cell function, and manipulation of innate immune responses, offering alternative treatment options for patients with refractory disease or intolerance to standard therapies.
Targeting B Cells in MS
B cell-targeted therapies, such as rituximab and ocrelizumab, selectively deplete B cells or inhibit their function, thereby attenuating inflammatory responses and reducing relapse rates. These agents have demonstrated efficacy in reducing disease activity and disability progression, particularly in patients with highly active or treatment-resistant MS.
Modulation of T Cell Function
Modulation of T cell function represents another promising approach in MS therapy, focusing on restoring immune tolerance and inhibiting autoreactive T cell responses. Therapeutic strategies include antigen-specific tolerance induction, regulatory T cell expansion, and cytokine-based immunomodulation, aiming to restore immune homeostasis and prevent disease relapses.
Neuroprotection and Remyelination Approaches
In addition to immunomodulation, emerging therapeutic paradigms in MS aim to promote neuroprotection and remyelination, addressing the underlying mechanisms of neurodegeneration and tissue repair.
Novel Drug Targets for Neuroprotection
Novel drug targets, such as neurotrophic factors, ion channel modulators, and anti-inflammatory agents, hold promise in preserving neuronal integrity, promoting axonal regeneration, and mitigating neurodegenerative processes in MS. By targeting multiple pathophysiological pathways, these agents offer potential synergistic effects and disease-modifying benefits.
Remyelination Therapies in Development
Remyelination therapies aim to restore damaged myelin sheaths and promote axonal remyelination, thereby preserving neuronal function and preventing disability progression in MS. Emerging approaches include remyelinating agents, stem cell-based therapies, and modulators of oligodendrocyte precursor cell differentiation, offering novel treatment strategies for demyelinating disorders.
Innovations in Stem Cell Therapy
Overview of Stem Cell Therapy for MS
Stem cell therapy represents a promising avenue in MS treatment, offering the potential to repair damaged tissues, modulate immune responses, and halt disease progression. Various stem cell sources and transplantation techniques have been investigated, with hematopoietic stem cell transplantation (HSCT) and mesenchymal stem cell (MSC) therapy emerging as leading candidates.
Hematopoietic Stem Cell Transplantation (HSCT)
HSCT involves the infusion of autologous or allogeneic hematopoietic stem cells to reset the immune system and induce immune tolerance. High-dose chemotherapy is administered to deplete autoreactive immune cells, followed by stem cell reinfusion to restore immune function. Clinical trials have demonstrated significant reductions in relapse rates, MRI lesion burden, and disability progression in MS patients undergoing HSCT.
Clinical Efficacy and Safety
HSCT has shown promising clinical efficacy in inducing long-term disease remission and stabilizing neurological function in MS patients, particularly those with aggressive or treatment-resistant disease. However, the procedure carries inherent risks, including infection, cytopenias, and organ toxicities, necessitating careful patient selection and peri-transplant monitoring to optimize safety outcomes.
Patient Selection Criteria
Patient selection criteria for HSCT include disease activity, treatment responsiveness, age, comorbidities, and functional status. Candidates typically exhibit active disease despite conventional therapies, with evidence of relapses, MRI activity, or disability progression. Multidisciplinary evaluation and shared decision-making facilitate individualized treatment recommendations and informed consent.
Mesenchymal Stem Cell (MSC) Therapy
MSC therapy involves the administration of allogeneic or autologous mesenchymal stem cells to modulate immune responses, promote tissue repair, and exert neuroprotective effects. MSCs possess immunomodulatory properties, secreting anti-inflammatory cytokines and growth factors that suppress autoimmune responses and enhance tissue regeneration in MS.
Mechanisms of Action
MSCs exert their therapeutic effects through multiple mechanisms, including inhibition of pro-inflammatory cytokine production, induction of regulatory T cells, promotion of neurotrophic factor secretion, and modulation of microglial activation. These pleiotropic actions contribute to immune regulation, neuroprotection, and remyelination in the CNS, offering potential benefits in MS treatment.
Clinical Trials and Outcomes
Clinical trials investigating MSC therapy in MS have reported promising results in terms of safety, feasibility, and preliminary efficacy outcomes. Improvements in clinical measures, such as relapse rates, disability scores, and MRI parameters, have been observed following MSC administration, highlighting the therapeutic potential of this approach in mitigating disease activity and promoting neurorepair.
Combination Therapies and Treatment Algorithms
Rational Combinations of DMTs with Stem Cell Therapy
Rational combinations of disease-modifying therapies (DMTs) with stem cell therapy represent a synergistic approach to MS treatment, targeting both immune-mediated inflammation and neurodegeneration. Sequential or concurrent administration of DMTs and stem cell transplantation may enhance treatment efficacy, minimize disease activity, and optimize long-term outcomes in selected patient populations.
Personalized Treatment Algorithms in MS Management
Personalized treatment algorithms integrate clinical, radiological, and molecular biomarkers to guide therapeutic decision-making and monitor disease progression in MS. Tailored treatment strategies account for individual patient characteristics, disease subtype, treatment responsiveness, and prognostic factors, optimizing therapeutic outcomes and minimizing adverse effects.
Adapting Treatment Plans Based on Disease Progression
Treatment plans in MS should be dynamic and adaptable, evolving in response to disease progression, treatment response, and patient preferences over time. Regular monitoring, clinical assessments, and shared decision-making facilitate adjustments in treatment intensity, modality, or combination based on evolving disease activity, treatment goals, and patient priorities.
Challenges and Future Directions
Addressing Safety Concerns in Stem Cell Therapy
Safety concerns surrounding stem cell therapy in MS include risks of infection, immune dysregulation, tumorigenesis, and long-term adverse effects. Rigorous preclinical studies, standardized protocols, and close post-transplant monitoring are essential to mitigate risks and ensure patient safety in stem cell-based interventions.
Optimizing Treatment Outcomes Through Multidisciplinary Care
Multidisciplinary care models involving neurologists, immunologists, rehabilitation specialists, and allied health professionals are essential for optimizing treatment outcomes and addressing diverse needs in MS management. Holistic approaches encompass medical management, rehabilitation interventions, psychosocial support, and lifestyle modifications, promoting comprehensive care delivery and patient-centered outcomes.
Regulatory and Ethical Considerations in Stem Cell Research
Regulatory frameworks and ethical guidelines governing stem cell research and clinical translation play a critical role in ensuring patient safety, research integrity, and responsible innovation. Transparent reporting, informed consent procedures, ethical oversight, and adherence to Good Clinical Practice (GCP) standards are essential for advancing stem cell therapies in MS and safeguarding patient welfare.
Patient Perspectives and Experiences
Living with MS: Challenges and Coping Mechanisms
Living with MS poses significant physical, emotional, and social challenges for patients and their caregivers. Fatigue, mobility limitations, cognitive impairments, and unpredictable disease course impact daily functioning and quality of life. Coping mechanisms, social support networks, and adaptive strategies help individuals navigate the challenges of MS and maintain resilience in the face of adversity.
Patient-Centered Approaches in Treatment Decision-Making
Patient-centered approaches in MS care prioritize shared decision-making, informed consent, and individualized treatment goals aligned with patient preferences and values. Empowering patients as active participants in treatment decisions fosters autonomy, trust, and therapeutic alliance, enhancing treatment adherence, satisfaction, and overall well-being.
Real-Life Testimonials on Stem Cell Therapy
Real-life testimonials from MS patients undergoing stem cell therapy provide valuable insights into treatment experiences, outcomes, and quality of life improvements. Personal narratives highlight the transformative potential of stem cell interventions in stabilizing disease progression, restoring function, and improving overall health and vitality, inspiring hope and advocacy within the MS community.
Health Economics and Access to Innovative Treatments
Cost-Effectiveness Analysis of Stem Cell Therapy vs. Conventional Treatments
Cost-effectiveness analyses of stem cell therapy versus conventional treatments in MS management evaluate the economic implications, healthcare resource utilization, and long-term outcomes associated with different treatment modalities. While stem cell therapy may entail upfront costs and resource investments, its potential to reduce disease burden, healthcare expenditures, and long-term disability may justify its cost-effectiveness in selected patient populations.
Insurance Coverage and Affordability Issues
Insurance coverage and affordability pose barriers to accessing innovative treatments, including stem cell therapy, for MS patients. Disparities in insurance policies, reimbursement criteria, and out-of-pocket expenses limit equitable access to advanced therapeutic options, exacerbating healthcare disparities and compromising patient outcomes. Advocacy efforts, policy reforms, and healthcare financing reforms are needed to address these access barriers and promote equitable healthcare access for all MS patients.
Equity in Access to Advanced Therapeutic Options
Equity in access to advanced therapeutic options, such as stem cell therapy, requires addressing structural barriers, socioeconomic disparities, and geographic inequalities in healthcare delivery. Comprehensive care models, patient assistance programs, and community outreach initiatives can enhance access to innovative treatments, reduce disparities, and improve health outcomes for underserved populations with MS.
Technological Advances in Monitoring and Management
Remote Monitoring and Telemedicine Solutions
Remote monitoring and telemedicine solutions enable real-time symptom tracking, remote consultations, and virtual healthcare delivery, enhancing access to specialized care and improving patient outcomes in MS management. Telehealth platforms, mobile applications, and wearable devices facilitate remote monitoring of disease activity, treatment adherence, and patient-reported outcomes, promoting proactive disease management and personalized care delivery.
Wearable Devices for Disease Tracking
Wearable devices, such as activity trackers, smartwatches, and biosensors, offer non-invasive tools for monitoring disease activity, physical activity levels, and physiological parameters in MS patients. These devices provide objective data on mobility, sleep quality, and vital signs, enabling personalized interventions, remote monitoring, and early detection of disease exacerbations, thereby optimizing clinical management and treatment outcomes.
Artificial Intelligence in Treatment Optimization
Artificial intelligence (AI) and machine learning algorithms hold promise in optimizing treatment algorithms, predicting disease trajectories, and identifying personalized therapeutic targets in MS management. AI-powered decision support systems analyze multi-modal data, including clinical, imaging, genomic, and biomarker profiles, to guide treatment selection, monitor treatment response, and optimize therapeutic outcomes, revolutionizing precision medicine approaches in MS care.
Global Collaborations and Research Consortia
International Efforts in MS Research
International collaborations and research consortia facilitate knowledge exchange, data sharing, and collaborative research efforts to advance understanding of MS pathogenesis, treatment outcomes, and healthcare delivery across diverse populations and healthcare settings. Collaborative initiatives, such as the Multiple Sclerosis International Federation (MSIF) and the International Progressive MS Alliance, foster interdisciplinary collaboration, research synergy, and global advocacy to accelerate progress in MS research and care.
Collaborative Networks for Clinical Trials
Collaborative networks for clinical trials, such as the National Institutes of Health (NIH)-funded Clinical and Translational Science Awards (CTSA) program and the European Medicines Agency (EMA)-endorsed European Clinical Research Infrastructure Network (ECRIN), facilitate multicenter trials, standardize research protocols, and harmonize data collection methodologies to generate robust evidence and accelerate translation of research findings into clinical practice.
Sharing of Best Practices and Data Harmonization
Sharing of best practices and data harmonization initiatives promote standardization, reproducibility, and comparability of research outcomes in MS research and clinical practice. Open-access repositories, data sharing platforms, and collaborative registries enable researchers to share data, tools, and resources, fostering transparency, collaboration, and innovation in MS research and healthcare delivery on a global scale.
Community Support and Advocacy
Role of Patient Advocacy Groups in Shaping Research and Policy
Patient advocacy groups play a vital role in raising awareness, advocating for research funding, and shaping policy priorities to address the unmet needs of MS patients and caregivers. These organizations provide educational resources, support services, and advocacy platforms to empower individuals affected by MS, amplify their voices, and drive positive change in research, healthcare, and social policies.
Supportive Services for MS Patients and Caregivers
Supportive services for MS patients and caregivers encompass a range of psychosocial, educational, and practical interventions to address holistic needs and enhance quality of life. Support groups, counseling services, caregiver training programs, and respite care initiatives provide emotional support, practical assistance, and coping strategies to navigate the challenges of MS and promote resilience in individuals and families affected by the disease.
Empowering Patients Through Education and Advocacy
Empowering patients through education and advocacy initiatives fosters informed decision-making, self-management skills, and active participation in healthcare decision-making. Patient education programs, self-help resources, and advocacy training empower individuals to become knowledgeable advocates, engage in shared decision-making with healthcare providers, and advocate for their rights and preferences in MS care and research.
Towards a Holistic Approach to MS Care
Integration of Conventional and Innovative Therapies
Integration of conventional and innovative therapies in MS care represents a paradigm shift towards a holistic, patient-centered approach that addresses the complex and multifaceted nature of the disease. Combining disease-modifying therapies, symptomatic management, rehabilitation interventions, and emerging therapeutic modalities enables tailored treatment strategies that optimize clinical outcomes, enhance quality of life, and promote holistic well-being in individuals with MS.
Patient-Centric Care Models for Optimal Outcomes
Patient-centric care models emphasize collaboration, communication, and shared decision-making between patients, caregivers, and healthcare providers to ensure individualized treatment plans that align with patient preferences, values, and goals. Holistic care delivery encompasses medical, psychosocial, and rehabilitative interventions that address physical, emotional, and social dimensions of MS, empowering patients to actively participate in their care and achieve optimal outcomes.
MS Research and Treatment Paradigms
MS research and treatment paradigms aim to advance understanding of disease mechanisms, identify novel therapeutic targets, and translate scientific discoveries into innovative therapies that improve outcomes and quality of life for individuals with MS. Collaborative research efforts, technological innovations, and patient-centered approaches hold promise in shaping the future landscape of MS care, driving progress towards effective treatments, and ultimately, a cure for this complex and debilitating condition.