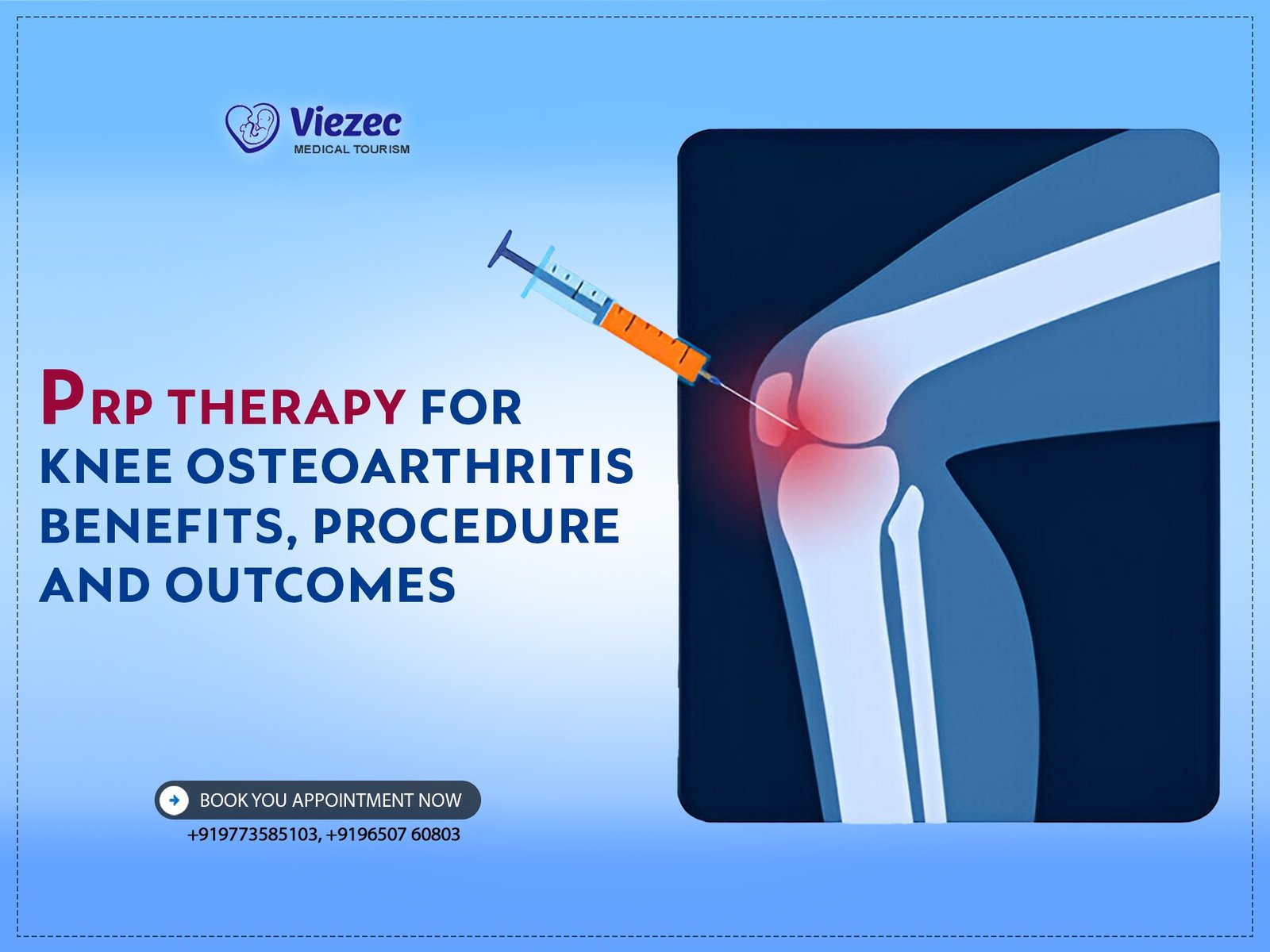
Knee osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown and eventual loss of the cartilage in the knee joint. It is the most common form of arthritis and a leading cause of disability among older adults. The condition leads to pain, stiffness, swelling, and decreased mobility, significantly impacting the quality of life. As the cartilage wears away, bones may rub against each other, causing further damage and pain. Over time, this can lead to bone spurs and reduced joint space, exacerbating symptoms and limiting joint function.
Overview of Platelet-Rich Plasma (PRP) Therapy
Platelet-rich plasma (PRP) therapy is a regenerative treatment that uses the patient’s own blood components to promote healing and tissue repair. PRP is derived from blood that has been processed to concentrate platelets, which are rich in growth factors and proteins essential for healing. When injected into the affected knee joint, PRP aims to reduce inflammation, promote cartilage repair, and alleviate pain. This minimally invasive procedure has gained popularity due to its potential to enhance natural healing processes and its relatively low risk compared to surgical interventions.
Purpose and Scope of the Document
This document aims to provide a comprehensive overview of PRP therapy as a treatment for knee osteoarthritis. It will explore the condition of knee osteoarthritis, detailing its causes, symptoms, and conventional treatments. Additionally, it will delve into the specifics of PRP therapy, including its history, mechanisms, benefits, procedural aspects, clinical outcomes, and potential risks. The goal is to inform patients, healthcare providers, and researchers about the potential of PRP therapy in managing knee osteoarthritis and improving patient outcomes.
Understanding Knee Osteoarthritis
Causes and Risk Factors
Knee osteoarthritis is influenced by various genetic, environmental, and lifestyle factors.
Genetic Factors
Genetics play a significant role in the development of knee osteoarthritis. Certain genetic markers are associated with an increased risk of developing the condition. Family history of osteoarthritis can predispose individuals to similar issues, suggesting a hereditary component. Research indicates that specific genes related to cartilage structure and function, inflammation, and bone density can influence the likelihood of developing OA. Understanding these genetic factors can help identify at-risk individuals and guide early interventions to manage or mitigate the disease’s progression.
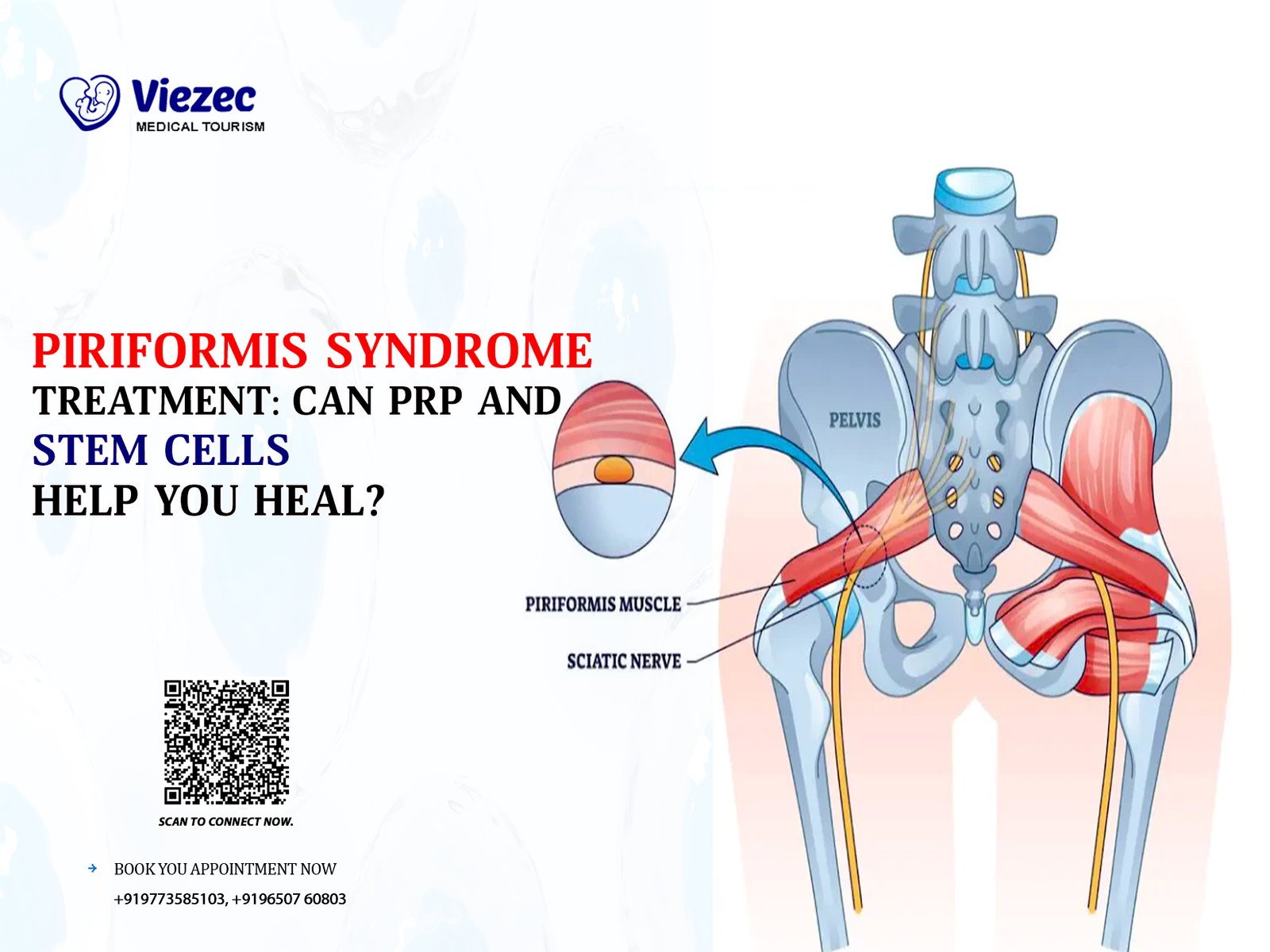
Environmental Influences
Environmental factors, such as occupation and physical activity, significantly impact knee osteoarthritis development. Jobs involving repetitive knee bending, heavy lifting, or prolonged standing can increase the risk. Additionally, previous joint injuries, such as fractures or ligament tears, can lead to post-traumatic osteoarthritis. Environmental pollutants and toxins might also contribute to joint degradation. Identifying and modifying these environmental risks, when possible, can help reduce the incidence of knee osteoarthritis and improve long-term joint health.
Lifestyle and Dietary Factors
Lifestyle and dietary choices play a crucial role in knee osteoarthritis. Obesity is a significant risk factor, as excess weight puts additional strain on knee joints, accelerating cartilage wear and tear. A diet lacking essential nutrients for joint health, such as omega-3 fatty acids, vitamins, and minerals, can also contribute to the condition. Regular physical activity, maintaining a healthy weight, and a balanced diet rich in anti-inflammatory foods can help manage and prevent knee osteoarthritis. Lifestyle modifications can alleviate symptoms and slow disease progression, improving overall joint function.
Symptoms and Diagnosis
Knee osteoarthritis presents with a range of symptoms that can vary in severity.
Common Symptoms
Common symptoms of knee osteoarthritis include pain, stiffness, swelling, and reduced range of motion. Pain is often worse with activity and relieved by rest but can become persistent as the condition progresses. Stiffness is typically most pronounced in the morning or after periods of inactivity. Swelling results from inflammation and the accumulation of excess joint fluid. Patients may also experience a grating sensation during joint movement due to cartilage loss and bone friction. These symptoms collectively impact daily activities and overall quality of life.
Diagnostic Techniques
Diagnosing knee osteoarthritis involves a combination of clinical evaluation, imaging, and laboratory tests. Clinicians assess symptoms, medical history, and perform a physical examination to evaluate joint tenderness, range of motion, and swelling. Imaging techniques, such as X-rays, MRI, and ultrasound, provide detailed views of the joint structure, revealing cartilage loss, bone spurs, and joint space narrowing. Laboratory tests may include blood work to rule out other conditions and analyze joint fluid for inflammatory markers. Accurate diagnosis is essential for developing an effective treatment plan tailored to the patient’s needs.
Conventional Treatments
Conventional treatments for knee osteoarthritis aim to alleviate symptoms and improve joint function.
Medication and Pain Management
Medication and pain management are primary approaches to treating knee osteoarthritis. Over-the-counter pain relievers like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce pain and inflammation. In some cases, prescription medications, including stronger analgesics or corticosteroids, may be necessary. Topical creams and gels can provide localized relief. These medications help manage symptoms but do not address the underlying cartilage damage. Patients must work with healthcare providers to find the most effective and safe medication regimen.
Physical Therapy
Physical therapy plays a crucial role in managing knee osteoarthritis. It involves exercises designed to strengthen the muscles around the knee, improve flexibility, and enhance joint stability. Physical therapists also educate patients on proper body mechanics and movement techniques to reduce strain on the knee. Modalities such as heat, ice, ultrasound, and electrical stimulation may be used to alleviate pain and inflammation. Regular physical therapy sessions can help maintain joint function, reduce pain, and improve the overall quality of life for individuals with knee osteoarthritis.
Surgical Options
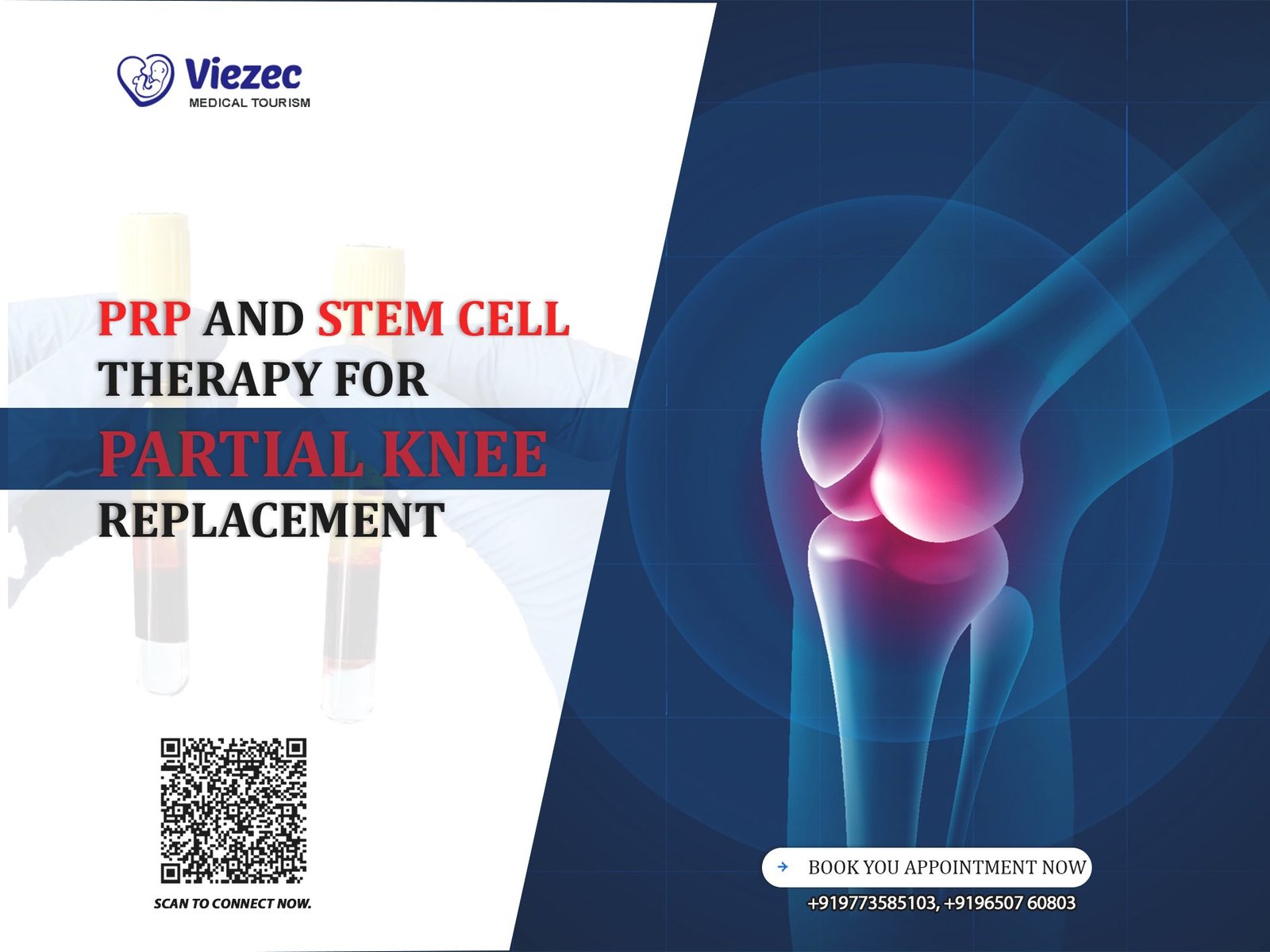
Surgical options are considered when conservative treatments fail to relieve knee osteoarthritis symptoms. Arthroscopy involves minimally invasive techniques to clean out the joint and remove damaged tissue. Osteotomy is a procedure that realigns the bones to reduce pressure on the knee joint. In severe cases, partial or total knee replacement may be necessary, where damaged joint surfaces are replaced with prosthetic components. These surgical interventions aim to restore joint function, alleviate pain, and improve mobility. However, surgery carries risks and requires a comprehensive evaluation of the patient’s overall health.
PRP Therapy: An Overview
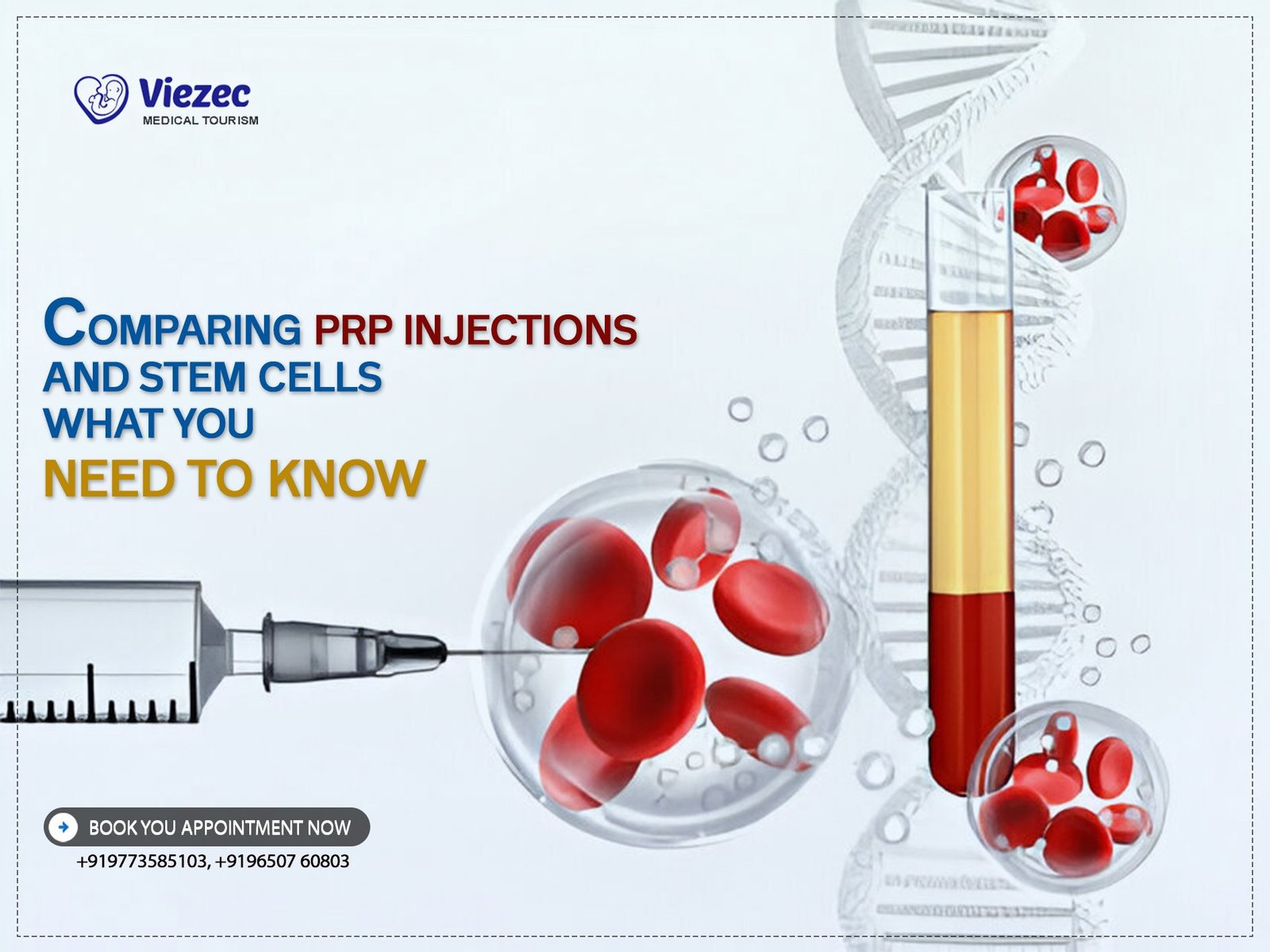
What is Platelet-Rich Plasma?
Platelet-rich plasma (PRP) is a concentrated form of plasma derived from the patient’s blood, containing a high concentration of platelets. Platelets are small blood cells that play a crucial role in healing and tissue repair. They contain growth factors, proteins, and other bioactive molecules essential for regenerating damaged tissues. PRP is prepared by collecting a blood sample, processing it through centrifugation to separate the components, and extracting the platelet-rich layer. This PRP is then injected into the affected area, promoting natural healing processes and reducing inflammation.
History and Development of PRP Therapy
PRP therapy has a long history and has evolved significantly over the years. Initially used in the 1970s in oral and maxillofacial surgery, its applications have expanded to various medical fields, including orthopedics, sports medicine, and dermatology. Early research demonstrated its potential in enhancing wound healing and tissue regeneration. Advancements in technology and a better understanding of PRP’s biological effects have led to its widespread adoption. Today, PRP therapy is used to treat a range of musculoskeletal conditions, including knee osteoarthritis, with growing evidence supporting its efficacy.
Mechanism of Action
Platelet Function and Growth Factors
Platelets play a central role in the mechanism of PRP therapy. When injected into the affected area, platelets release growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF). These growth factors stimulate cell proliferation, collagen production, and tissue regeneration. They also enhance the formation of new blood vessels, improving blood supply to the damaged tissues. This biological activity accelerates healing, reduces inflammation, and promotes the repair of damaged cartilage in knee osteoarthritis.
Biological Impact on Knee Osteoarthritis
The biological impact of PRP on knee osteoarthritis is multifaceted. PRP injections reduce inflammation by modulating the activity of inflammatory cells and cytokines. They promote the synthesis of extracellular matrix components, enhancing cartilage repair and regeneration. PRP also stimulates the proliferation of chondrocytes, the cells responsible for maintaining healthy cartilage. Additionally, PRP enhances the production of hyaluronic acid, improving joint lubrication and reducing friction. These combined effects alleviate pain, improve joint function, and slow the progression of knee osteoarthritis.
Benefits of PRP Therapy for Knee Osteoarthritis
Pain Relief
One of the primary benefits of PRP therapy for knee osteoarthritis is pain relief. PRP injections reduce inflammation and modulate pain pathways, providing significant symptom relief. Patients often experience a reduction in pain intensity and frequency, allowing them to engage in daily activities with greater ease. The analgesic effects of PRP can last for several months, offering a longer duration of relief compared to conventional treatments. By addressing the underlying causes of pain, PRP therapy improves the overall quality of life for individuals with knee osteoarthritis.
Improved Joint Function
PRP therapy significantly improves joint function in individuals with knee osteoarthritis. The regenerative effects of PRP enhance cartilage repair and reduce inflammation, leading to increased joint mobility and flexibility. Patients often report improved ability to perform daily tasks and participate in physical activities. Strengthening the muscles around the knee joint further supports functional improvements. By restoring joint function, PRP therapy helps individuals maintain an active lifestyle and reduces the risk of secondary complications associated with reduced mobility.
Reduced Inflammation
PRP therapy effectively reduces inflammation in the knee joint, a key factor in osteoarthritis progression. The growth factors and bioactive molecules in PRP modulate the inflammatory response, decreasing the production of pro-inflammatory cytokines and mediators. This reduction in inflammation alleviates pain, swelling, and stiffness, providing symptomatic relief. By addressing inflammation at its source, PRP therapy offers a targeted approach to managing knee osteoarthritis, unlike conventional treatments that primarily focus on symptom control.
Delay in Disease Progression
PRP therapy has the potential to delay the progression of knee osteoarthritis. By promoting cartilage repair and regeneration, PRP helps preserve joint structure and function. The anti-inflammatory effects of PRP further contribute to slowing disease progression. Early intervention with PRP therapy can prevent or delay the need for more invasive treatments such as joint replacement surgery. This disease-modifying potential makes PRP a valuable option in the comprehensive management of knee osteoarthritis, especially for individuals in the early to moderate stages of the condition.
Comparative Benefits over Other Treatments
PRP therapy offers several comparative benefits over conventional treatments for knee osteoarthritis. Unlike medications that provide temporary symptom relief, PRP addresses the underlying causes of pain and inflammation, promoting long-term healing. Physical therapy requires ongoing commitment, while PRP offers sustained benefits with fewer sessions. Compared to surgical options, PRP is minimally invasive, with lower risks and shorter recovery times. These advantages make PRP an attractive option for individuals seeking effective and less invasive treatments for knee osteoarthritis.
PRP Therapy Procedure
Pre-Treatment Evaluation
Medical History and Examination
The pre-treatment evaluation for PRP therapy begins with a thorough medical history and examination. Healthcare providers assess the patient’s overall health, knee pain severity, and previous treatments. A detailed medical history helps identify any contraindications or underlying conditions that may affect the therapy’s efficacy. Physical examination includes evaluating the range of motion, joint stability, and areas of tenderness. This comprehensive assessment ensures that PRP therapy is appropriate for the patient’s specific condition and sets the foundation for a successful treatment plan.
Imaging and Laboratory Tests
Imaging and laboratory tests are crucial components of the pre-treatment evaluation for PRP therapy. Imaging techniques such as X-rays, MRI, and ultrasound provide detailed views of the knee joint, helping to assess the extent of cartilage damage, joint space narrowing, and presence of bone spurs. Laboratory tests may include blood work to rule out other conditions and ensure the patient’s overall health is suitable for the procedure. Joint fluid analysis can help confirm the diagnosis of osteoarthritis. These diagnostic tools aid in creating a tailored treatment plan for optimal results.
Preparation of PRP
Blood Collection
The preparation of PRP begins with blood collection. A healthcare professional draws a small amount of blood, typically from the patient’s arm. The amount of blood required depends on the specific PRP preparation protocol and the treatment area. This step is minimally invasive and similar to a standard blood draw. The collected blood is then processed to separate the various components and concentrate the platelets. Proper blood collection is essential to ensure the quality and efficacy of the PRP used in the therapy.
Centrifugation Process
Centrifugation is a critical step in preparing PRP. The collected blood is placed in a centrifuge, a machine that spins at high speeds to separate its components based on density. This process typically involves two centrifugation steps. In the first step, the blood is separated into plasma, red blood cells, and a platelet-rich layer. In the second step, the platelet-rich layer is further concentrated. The goal is to obtain a high concentration of platelets and growth factors in a small volume of plasma, which is essential for effective PRP therapy.
PRP Extraction
PRP extraction is the final step in the preparation process. After centrifugation, the concentrated platelet-rich plasma is carefully extracted from the rest of the blood components. This extraction is done under sterile conditions to prevent contamination. The resulting PRP contains a high concentration of platelets, growth factors, and bioactive molecules essential for tissue repair and regeneration. The prepared PRP is then ready for injection into the affected knee joint. Ensuring the purity and concentration of PRP is crucial for achieving optimal therapeutic outcomes.
Administration of PRP
Injection Techniques
The administration of PRP involves precise injection techniques to ensure effective delivery to the affected area. The PRP is injected directly into the knee joint using a fine needle. Healthcare providers may use various injection techniques, such as intra-articular or peri-articular injections, depending on the specific condition and target tissues. The goal is to distribute the PRP evenly within the joint space, maximizing its therapeutic potential. Proper injection techniques minimize discomfort and enhance the efficacy of the treatment.
Ultrasound Guidance
Ultrasound guidance is often used during PRP administration to enhance accuracy and effectiveness. Ultrasound imaging provides real-time visualization of the knee joint, allowing healthcare providers to precisely locate the target area and avoid surrounding structures. This guidance ensures that the PRP is injected into the most affected areas, optimizing the delivery of growth factors and bioactive molecules. Using ultrasound guidance improves the safety and outcomes of PRP therapy, particularly in complex cases or when targeting specific joint regions.
Post-Treatment Care
Immediate Aftercare
Immediate aftercare following PRP therapy is crucial for optimal results. Patients are advised to rest the treated knee and avoid strenuous activities for the first few days. Applying ice packs can help reduce swelling and discomfort. Healthcare providers may recommend pain relievers if needed, but NSAIDs are usually avoided as they can interfere with the PRP’s action. Keeping the injection site clean and monitoring for any signs of infection is essential. Following these aftercare instructions helps facilitate the healing process and maximize the benefits of PRP therapy.
Long-term Follow-up
Long-term follow-up is an integral part of PRP therapy for knee osteoarthritis. Regular follow-up appointments allow healthcare providers to monitor the patient’s progress, assess the treatment’s effectiveness, and make any necessary adjustments to the care plan. Patients may be advised to undergo physical therapy to enhance joint function and strength. Periodic imaging and clinical evaluations help track the condition’s progression and ensure sustained benefits. Ongoing communication between patients and healthcare providers is vital for managing knee osteoarthritis effectively.
Clinical Outcomes and Research Findings
Efficacy Studies
Short-Term Outcomes
Efficacy studies have demonstrated promising short-term outcomes for PRP therapy in treating knee osteoarthritis. Patients typically report significant reductions in pain and improvements in joint function within a few weeks of treatment. Clinical trials have shown that PRP injections can provide relief comparable to or better than conventional treatments such as corticosteroids or hyaluronic acid injections. The anti-inflammatory and regenerative effects of PRP contribute to these positive outcomes, making it an effective short-term solution for knee osteoarthritis symptoms.
Long-Term Outcomes
Long-term outcomes of PRP therapy for knee osteoarthritis are also encouraging. Research indicates that the benefits of PRP can persist for several months to years, offering sustained relief from pain and improved joint function. Studies have shown that PRP can slow the progression of osteoarthritis, delaying the need for more invasive treatments like joint replacement surgery. Long-term follow-up of patients treated with PRP has revealed continued improvements in quality of life and reduced reliance on pain medications, highlighting the therapy’s lasting impact.
Comparative Studies
PRP vs. Corticosteroids
Comparative studies between PRP and corticosteroids have shown that PRP offers distinct advantages. While corticosteroid injections provide rapid pain relief, their effects are often short-lived, and repeated use can lead to joint damage. PRP, on the other hand, promotes long-term healing and regeneration without the adverse effects associated with corticosteroids. Patients treated with PRP report longer-lasting pain relief and improved joint function compared to those receiving corticosteroids, making PRP a more favorable option for sustainable osteoarthritis management.
PRP vs. Hyaluronic Acid
PRP therapy has also been compared to hyaluronic acid injections, another common treatment for knee osteoarthritis. Studies have found that PRP provides superior pain relief and functional improvement compared to hyaluronic acid. The regenerative properties of PRP, which enhance cartilage repair and reduce inflammation, contribute to its greater efficacy. While hyaluronic acid primarily acts as a lubricant and shock absorber, PRP addresses the underlying causes of osteoarthritis, offering more comprehensive and long-lasting benefits for patients.
Patient Satisfaction and Quality of Life
Patient satisfaction and quality of life significantly improve with PRP therapy for knee osteoarthritis. Surveys and studies consistently show high levels of patient satisfaction due to the reduction in pain, increased mobility, and improved daily functioning. Patients appreciate the minimally invasive nature of the treatment and the absence of significant side effects. The enhanced quality of life, ability to perform routine activities, and delayed need for surgical interventions contribute to the positive reception of PRP therapy among knee osteoarthritis patients.
Risks and Considerations
Potential Side Effects
Common Side Effects
PRP therapy is generally safe, but some common side effects may occur. These include mild pain, swelling, and bruising at the injection site. Patients may experience temporary stiffness or discomfort in the treated knee. These side effects are typically short-lived and resolve within a few days. Proper aftercare and adherence to medical advice can help minimize these effects. Patients should be informed about these potential side effects before treatment to set realistic expectations and ensure they are adequately prepared.
Rare Complications
Rare complications of PRP therapy are infrequent but can include infection, allergic reactions, and nerve or tissue damage. Infection at the injection site is a concern, but strict sterile techniques during the procedure minimize this risk. Allergic reactions to PRP are uncommon since it is derived from the patient’s own blood. Nerve or tissue damage is rare and usually associated with improper injection techniques. Healthcare providers should discuss these rare complications with patients to ensure informed consent and address any concerns.
Contraindications
Medical Conditions
Certain medical conditions can contraindicate PRP therapy for knee osteoarthritis. Patients with bleeding disorders, severe anemia, or active infections are typically not suitable candidates. Conditions that affect platelet function or blood clotting can compromise the effectiveness of PRP and increase the risk of complications. Additionally, patients with certain autoimmune diseases or cancers may not be ideal candidates. A thorough medical evaluation and consultation with a healthcare provider are essential to determine the suitability of PRP therapy based on individual health conditions.
Patient Eligibility Criteria
Patient eligibility criteria for PRP therapy include factors such as overall health, severity of knee osteoarthritis, and previous treatments. Ideal candidates are those with mild to moderate osteoarthritis who have not responded adequately to conventional treatments. Patients should have realistic expectations about the outcomes and be willing to follow post-treatment care instructions. Eligibility also depends on the ability to undergo blood collection and the absence of contraindications. A comprehensive evaluation by a healthcare provider ensures that PRP therapy is appropriate and likely to be effective.
Cost and Accessibility
Insurance Coverage
The cost of PRP therapy can be a consideration for many patients. Currently, PRP therapy is often considered experimental or not standard by insurance companies, leading to limited coverage. Patients may need to pay out-of-pocket for the treatment, which can be expensive. Some insurance plans may cover PRP therapy if it is deemed medically necessary or if other treatments have failed. Patients should consult their insurance providers and healthcare providers to understand the coverage options and potential out-of-pocket costs.
Availability of Treatment Centers
The availability of PRP therapy varies by location and the expertise of healthcare providers. Specialized clinics and orthopedic centers often offer PRP therapy, but access may be limited in certain areas. Patients may need to travel to specialized centers for treatment. The increasing popularity and evidence supporting PRP therapy are leading to wider availability, but it is essential to seek treatment from experienced and qualified healthcare providers to ensure safety and efficacy. Patients should research and choose reputable centers with a track record of successful PRP treatments.
Future Directions in PRP Therapy
Advances in PRP Technology
Innovations in PRP Preparation
Advances in PRP technology are enhancing the efficacy and consistency of the therapy. Innovations in PRP preparation techniques, such as standardized centrifugation protocols and automated systems, are improving the concentration and quality of PRP. These advancements ensure a higher yield of growth factors and bioactive molecules, optimizing the therapeutic potential. Researchers are also exploring methods to customize PRP formulations based on individual patient needs and specific conditions. These innovations hold promise for more effective and tailored PRP treatments for knee osteoarthritis.
Enhanced Injection Techniques
Enhanced injection techniques are being developed to improve the precision and effectiveness of PRP therapy. Ultrasound-guided injections are becoming more common, allowing for accurate placement of PRP in the targeted areas. Techniques such as microneedling and advanced delivery systems are being explored to enhance tissue penetration and distribution. These improvements aim to maximize the therapeutic benefits of PRP by ensuring that the growth factors reach the most affected tissues. Continued advancements in injection techniques will contribute to better outcomes and patient satisfaction.
Ongoing and Future Research
Clinical Trials
Ongoing and future clinical trials are critical for advancing PRP therapy for knee osteoarthritis. Researchers are conducting studies to further understand the optimal protocols, dosages, and frequencies of PRP injections. Clinical trials are also exploring the long-term effects of PRP therapy and its efficacy in different patient populations. Comparative studies with other treatments continue to provide valuable insights. The growing body of evidence from these trials will help refine PRP therapy, establish best practices, and potentially lead to broader acceptance and standardization.
Emerging Applications
Emerging applications of PRP therapy are expanding its potential beyond knee osteoarthritis. Researchers are investigating the use of PRP in treating other musculoskeletal conditions, such as tendonitis, ligament injuries, and muscle strains. PRP is also being explored in fields like dermatology for wound healing and hair restoration. The versatility of PRP and its regenerative properties open up new avenues for treatment across various medical specialties. Continued research and innovation will likely lead to the discovery of additional therapeutic applications for PRP.
Integrative Approaches
Combining PRP with Other Therapies
Integrative approaches that combine PRP with other therapies are showing promise in enhancing treatment outcomes. Combining PRP with physical therapy, hyaluronic acid injections, or stem cell therapy can provide synergistic effects. These combinations can optimize the healing environment, promote cartilage repair, and improve joint function. Research is ongoing to determine the most effective integrative strategies and protocols. By leveraging the strengths of multiple therapies, integrative approaches aim to provide comprehensive and personalized treatment for knee osteoarthritis.
Holistic Management of Osteoarthritis
Holistic management of osteoarthritis incorporates PRP therapy as part of a broader treatment plan. This approach includes lifestyle modifications, nutritional support, physical therapy, and complementary therapies like acupuncture and yoga. Holistic management focuses on addressing the root causes of osteoarthritis, promoting overall health and well-being, and preventing disease progression. Integrating PRP therapy into a holistic plan can enhance its benefits and improve patient outcomes. This comprehensive approach empowers patients to take an active role in managing their condition and achieving long-term joint health.
Frequently Asked Questions
1) What is PRP therapy for knee osteoarthritis?
PRP therapy uses a small sample of your blood processed to concentrate platelets, then injects it into the knee joint. Platelet growth factors can help reduce inflammation, support tissue repair, and improve function. It’s a minimally invasive option that may complement physiotherapy and lifestyle modifications for osteoarthritis management.
2) How effective is PRP for knee osteoarthritis?
Many studies report meaningful pain reduction and improved function after PRP injections compared with placebo or hyaluronic acid in some cases. Outcomes depend on disease severity, number of injections, and rehab adherence. PRP is not a cure, but it may delay escalation to stronger pain medications or surgery for select patients.
3) How long does PRP relief last for knee OA?
Relief commonly lasts 6–12 months for many patients, sometimes longer with a series of injections and ongoing strengthening. Results vary by age, activity level, and cartilage damage. Maintenance sessions may be considered if symptoms gradually return and your clinician agrees that repeat PRP is appropriate.
4) How many PRP sessions are needed?
Protocols vary, but clinicians often recommend 1–3 injections spaced a few weeks apart. A single injection may help, while a short series can extend benefits for some patients. Your plan should be individualized after evaluation, imaging review, and a discussion of goals, comorbidities, and recovery timeline.
5) Is PRP safe for knee osteoarthritis?
PRP is generally well tolerated because it uses your own blood. Temporary soreness, swelling, or stiffness can occur for a few days. Serious complications are uncommon when performed by trained clinicians under sterile technique. Always discuss medications, bleeding risks, and contraindications before scheduling treatment.
6) Who should avoid or delay PRP?
People with active infection, poorly controlled bleeding disorders, severe anemia, or certain cancers may not be candidates. Recent NSAID use can affect platelet function and may be paused per clinician guidance. Your doctor will review medical history, imaging, and goals to confirm if PRP is appropriate.
For more information or to schedule a consultation, visit us online.