Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare neurological disorder characterized by progressive weakness and impaired sensory function due to damage to the myelin sheath of peripheral nerves. While treatments such as corticosteroids, immunoglobulins, and plasma exchange have been utilized to manage CIDP symptoms, some patients do not respond adequately to these conventional therapies. In recent years, stem cell transplant (SCT) has emerged as a promising option for refractory CIDP cases, offering the potential to halt disease progression and improve neurological function.
Understanding CIDP and its Challenges
CIDP: A Complex Neurological Disorder
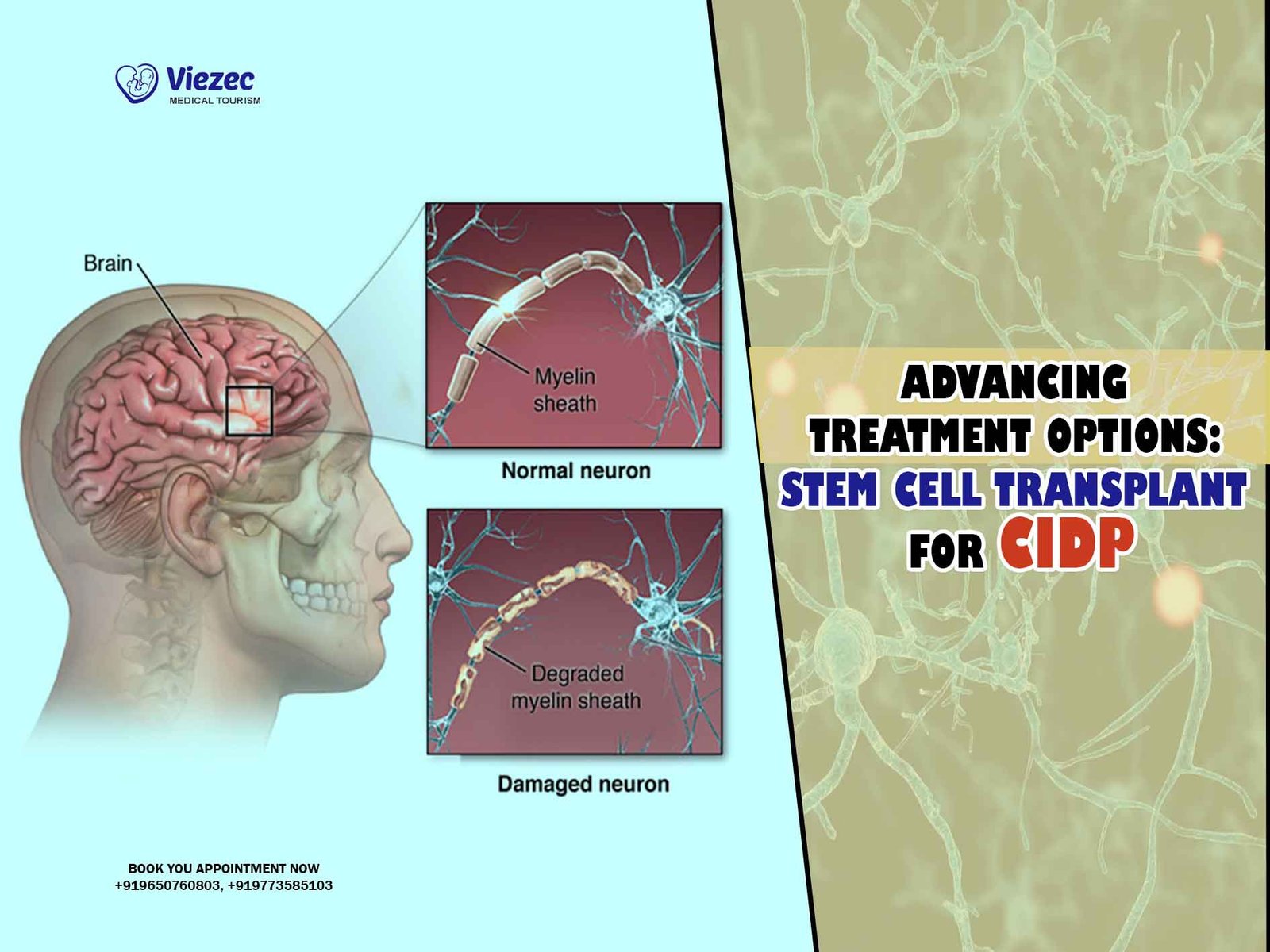
CIDP is considered an autoimmune disorder, where the body’s immune system mistakenly attacks the myelin sheath surrounding peripheral nerves. This leads to inflammation and demyelination, disrupting the transmission of nerve signals and resulting in symptoms such as weakness, sensory loss, and impaired coordination. CIDP is characterized by its chronic nature, with symptoms persisting or relapsing over months or years.
Challenges in CIDP Treatment
Managing CIDP presents several challenges. Firstly, the variable and unpredictable nature of the disease makes it difficult to determine the most effective treatment approach for individual patients. Secondly, while conventional therapies such as corticosteroids and immunoglobulins can provide symptom relief for many patients, a significant proportion do not respond adequately or experience intolerable side effects. Additionally, long-term use of these therapies may be associated with adverse effects such as infections, diabetes, and osteoporosis.
Promise of Stem Cell Transplantation
Stem Cells: A Regenerative Approach
Stem cells have garnered considerable attention in the field of regenerative medicine due to their unique ability to differentiate into various cell types and repair damaged tissues. In the context of CIDP, stem cell transplantation offers a novel therapeutic strategy by targeting the underlying immune dysfunction and promoting nerve regeneration.
Mechanism of Action
The rationale behind stem cell transplantation in CIDP lies in its immunomodulatory effects. By resetting the immune system, stem cells can potentially suppress the aberrant immune response responsible for attacking the peripheral nerves. Moreover, stem cells may promote remyelination and nerve repair, further enhancing neurological function in CIDP patients.
Types of Stem Cell Transplantation
Stem cell transplantation can be broadly categorized into autologous and allogeneic approaches. In autologous transplantation, stem cells are harvested from the patient’s own body, typically from bone marrow or peripheral blood, and then reintroduced following conditioning therapy. Allogeneic transplantation, on the other hand, involves using stem cells sourced from a compatible donor.
Clinical Evidence and Outcomes
While research on stem cell transplantation for CIDP is still in its early stages, several studies have reported promising outcomes. A systematic review published in the Journal of Neurology in 2022 analyzed data from multiple clinical trials and observational studies involving SCT in CIDP patients. The review found that a significant proportion of patients achieved clinical improvement following stem cell transplantation, with some experiencing long-term remission of symptoms.
Considerations and Challenges
Patient Selection
Identifying suitable candidates for stem cell transplantation is crucial to maximizing treatment efficacy and minimizing risks. Patient selection criteria may include disease severity, responsiveness to conventional therapies, and absence of significant comorbidities. Additionally, thorough pre-transplant evaluation is essential to assess the patient’s overall health status and potential risks associated with the procedure.
Safety and Adverse Events
While stem cell transplantation holds promise as a treatment for CIDP, it is not without risks. The conditioning regimen used to prepare the patient’s immune system for transplantation can be associated with significant toxicity, including infections, organ damage, and secondary malignancies. Moreover, the long-term effects of stem cell transplantation on immune function and neurological outcomes require further investigation.
Cost and Accessibility
Stem cell transplantation is a complex and resource-intensive procedure that may not be readily available or affordable for all CIDP patients. Factors such as healthcare coverage, access to specialized medical centers, and logistical considerations can pose barriers to accessing this treatment option. Addressing issues of cost and accessibility is essential to ensuring equitable access to stem cell transplantation for eligible patients.
Future Directions and Research Opportunities
Refinement of Treatment Protocols
Ongoing research efforts are focused on optimizing stem cell transplantation protocols for CIDP, with the aim of improving treatment outcomes and minimizing associated risks. This includes exploring alternative conditioning regimens, refining patient selection criteria, and investigating the use of novel stem cell sources or delivery methods.
Biomarkers and Predictive Factors
The identification of biomarkers and predictive factors associated with treatment response is another area of active investigation. By better understanding the underlying mechanisms of CIDP and the immune response to stem cell transplantation, researchers hope to develop biomarker-based strategies for patient stratification and personalized treatment approaches.
Combination Therapies
Combining stem cell transplantation with other immunomodulatory agents or neuroprotective therapies represents a promising strategy for enhancing treatment efficacy in CIDP. Preclinical studies have shown synergistic effects between stem cells and adjunctive therapies, suggesting the potential for combination approaches to improve clinical outcomes and durability of response.
Stem cell transplantation holds considerable promise as a therapeutic option for patients with refractory CIDP, offering the potential for disease modification and long-term symptom relief. While further research is needed to refine treatment protocols, elucidate mechanisms of action, and address safety concerns, early clinical evidence suggests that stem cell transplantation may represent a significant advance in the management of this challenging neurological disorder. By harnessing the regenerative potential of stem cells, we may pave the way for more effective and personalized treatment strategies for CIDP patients in the future.