Treatment of autoimmune diseases has long presented a formidable challenge. These conditions, wherein the body’s immune system mistakenly attacks its own tissues, can lead to a wide array of debilitating symptoms and complications. Traditional therapies often focus on managing symptoms rather than addressing the underlying immune dysfunction. However, in recent years, there has been growing interest in the potential of bone marrow transplants to revolutionize the treatment of autoimmune diseases. We will explore the science behind autoimmune diseases, the role of bone marrow transplants in their treatment, and the potential benefits and challenges associated with this approach.
Understanding Autoimmune Diseases
What Are Autoimmune Diseases?
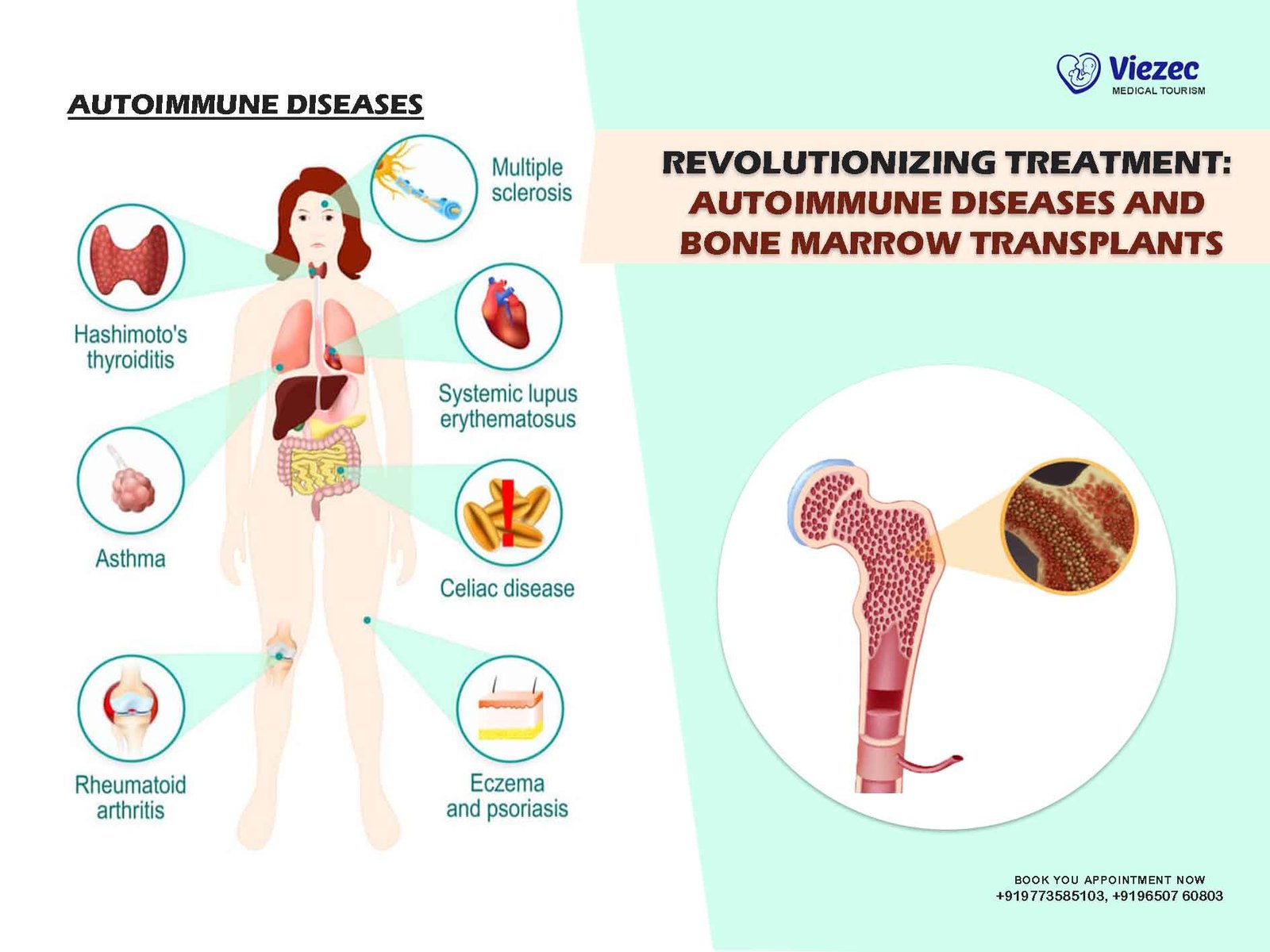
Autoimmune diseases encompass a diverse group of conditions in which the immune system erroneously identifies the body’s own tissues as foreign invaders, leading to inflammation and tissue damage. There are more than 80 known autoimmune diseases, including rheumatoid arthritis, lupus, multiple sclerosis, type 1 diabetes, and Crohn’s disease, among others. These diseases can affect virtually any part of the body, from the skin and joints to organs such as the heart, kidneys, and brain.
Underlying Mechanisms
The exact cause of autoimmune diseases remains elusive, but they are thought to arise from a combination of genetic predisposition and environmental triggers. In individuals with a genetic susceptibility, exposure to certain environmental factors such as infections, toxins, or stressors may initiate an abnormal immune response. This response involves the activation of various immune cells, including T cells, B cells, and antibodies, which target and attack the body’s own tissues.
Challenges in Treatment
Treating autoimmune diseases poses significant challenges due to their complex and multifactorial nature. Traditional approaches typically involve the use of immunosuppressive drugs to dampen the immune response and alleviate symptoms. While these medications can provide relief for some patients, they often come with side effects and may only offer temporary benefits. Moreover, they do not address the underlying immune dysfunction, leaving patients susceptible to disease flares and progression over time.
Role of Bone Marrow Transplants
What Is a Bone Marrow Transplant?
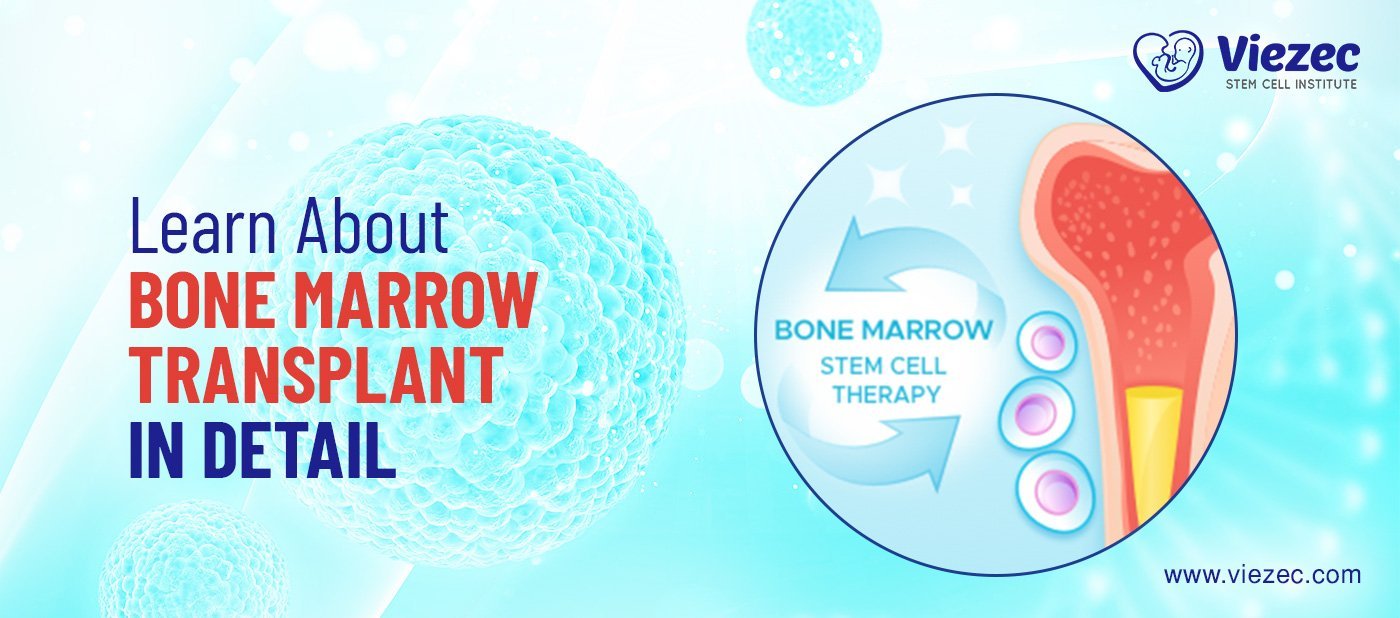
A bone marrow transplant, also known as a hematopoietic stem cell transplant (HSCT), is a procedure in which diseased or damaged bone marrow is replaced with healthy stem cells. These stem cells, which can differentiate into various blood cell types, are typically obtained from either the patient (autologous transplant) or a compatible donor (allogeneic transplant). The goal of the transplant is to replenish the patient’s immune system with healthy cells capable of restoring normal immune function.
Potential Mechanisms of Action
Bone marrow transplants hold promise for the treatment of autoimmune diseases due to their ability to reset the immune system. The high-dose chemotherapy or radiation used to deplete the existing bone marrow also targets the aberrant immune cells responsible for the autoimmune response. Subsequent infusion of healthy stem cells allows for the regeneration of a new immune system with a restored balance between regulatory and effector immune cells. This resetting of the immune system may help halt the autoimmune process and promote tolerance to self-antigens.
Evidence from Clinical Studies
While bone marrow transplants have been utilized for decades in the treatment of hematological malignancies such as leukemia and lymphoma, their application to autoimmune diseases is a more recent development. Clinical studies investigating the use of HSCT for autoimmune diseases have shown promising results, particularly in patients with severe, treatment-resistant disease. For example, a landmark trial published in 2017 demonstrated long-term remission in a significant proportion of patients with multiple sclerosis following autologous HSCT.
Considerations for Patient Selection
Patient selection is critical to the success of bone marrow transplantation for autoimmune diseases. Candidates are typically individuals with severe, refractory disease who have failed conventional therapies and face a high risk of disability or mortality. Factors such as disease duration, activity, and organ involvement are taken into account when evaluating eligibility for transplant. Additionally, patients must undergo rigorous pre-transplant screening to assess their overall health and suitability for the procedure.
Benefits and Challenges
Potential Benefits
The potential benefits of bone marrow transplants for autoimmune diseases are manifold. Unlike traditional immunosuppressive therapies, which merely manage symptoms, HSCT offers the possibility of achieving sustained remission or even cure. By resetting the immune system, transplant recipients may experience long-term suppression of disease activity and a reduced need for ongoing medication. Furthermore, the durability of treatment responses observed in some patients suggests that HSCT may alter the natural course of autoimmune diseases, preventing relapses and progression.
Challenges and Risks
Despite the promise of HSCT, several challenges and risks must be considered. The procedure itself carries inherent risks, including infection, bleeding, and graft-versus-host disease (in allogeneic transplants). Additionally, the intensive conditioning regimen required for HSCT can cause significant toxicity and may result in long-term complications such as infertility and secondary malignancies. Furthermore, while many patients experience significant improvements in disease activity following transplant, not all achieve durable remission, and relapses can occur.
Future Directions
Refinement of Techniques
Advances in transplant techniques and supportive care have the potential to further improve outcomes and reduce complications associated with HSCT for autoimmune diseases. Strategies to minimize the toxicity of conditioning regimens, such as the use of reduced-intensity or non-myeloablative approaches, are being explored. Additionally, refinement of patient selection criteria and better understanding of the underlying immunological mechanisms may help optimize transplant outcomes and identify those most likely to benefit from the procedure.
Combination Therapies
The future of HSCT in the treatment of autoimmune diseases may also involve the development of combination therapies that integrate transplant with other immune-modulating agents. For example, the use of biologic agents targeting specific immune pathways, such as anti-CD20 monoclonal antibodies or cytokine inhibitors, in conjunction with HSCT may enhance treatment efficacy and reduce the risk of disease relapse. Similarly, emerging approaches such as chimeric antigen receptor (CAR) T-cell therapy hold promise for achieving more targeted and durable immune modulation.
The treatment landscape for autoimmune diseases is evolving rapidly, driven by advances in our understanding of immune dysregulation and therapeutic strategies. Bone marrow transplantation represents a paradigm shift in the management of these conditions, offering the potential for long-term remission or even cure in select patients. While challenges and risks remain, ongoing research and clinical experience continue to refine transplant techniques and improve outcomes. With further innovation and collaboration, HSCT has the potential to revolutionize the treatment of autoimmune diseases and improve the lives of millions of patients worldwide.