Depression is one of the most pressing health challenges of our time—affecting millions globally and resisting conventional treatments in far too many cases. While antidepressants, therapy, and lifestyle changes help some, others are left navigating a cycle of temporary relief and recurring symptoms. That’s where stem cell therapy is beginning to change the conversation.
This article explores the groundbreaking potential of stem cells to go beyond symptom management and address the biological root causes of depression. From encouraging neural regeneration and reducing brain inflammation to repairing emotional circuitry damaged by trauma, stem cell therapy represents a fundamentally new approach to healing the mind.
Backed by early research, animal studies, and emerging clinical trials, the science is promising—but still evolving. We break down the types of stem cells, how they might interact with the brain, what the current data says, and where the therapy stands in terms of accessibility, cost, and ethical considerations.
Whether you’re a healthcare provider, a patient seeking new hope, or simply curious about the future of mental health treatment, this deep dive offers a clear and inspiring look at how regenerative medicine could transform the way we treat depression—one cell at a time.
The Mental Health Crisis—Why We Need New Solutions
Depression by the Numbers: A Global Epidemic
Depression is more than just feeling down—it’s a widespread mental health disorder that affects over 280 million people worldwide, according to the World Health Organization (2023). In the United States, nearly 1 in 5 adults experience mental illness each year, and depression is one of the most commonly diagnosed conditions. It’s also the leading cause of disability worldwide, often disrupting relationships, careers, and overall quality of life.
Despite increased awareness, depression remains underdiagnosed and undertreated in many communities. The emotional toll is immense, but the economic burden—estimated in the hundreds of billions annually—adds to the urgency for better solutions.
The Limitations of Current Treatments
Today’s most common treatments—antidepressants like SSRIs, cognitive behavioral therapy (CBT), and lifestyle modifications—help many, but not all. In fact, studies show that up to 30% of patients have treatment-resistant depression, meaning they’ve tried multiple therapies with little or no relief. Even for those who do respond, the process can take weeks or months, and relapse is common.
This points to a frustrating truth: current treatments often manage symptoms without addressing root causes.
Why Innovation Is No Longer Optional
We’re at a crossroads. The rising demand for effective, lasting solutions is colliding with the limits of traditional treatment models. Depression is a complex, deeply individual condition, influenced by genetics, trauma, inflammation, and neurobiology. A cookie-cutter approach just doesn’t cut it anymore.
That’s why the field of regenerative medicine and especially stem cell therapy—is generating so much excitement. It offers a fundamentally different approach: healing the brain from the inside out. Not just managing symptoms, but potentially repairing the systems that drive them.
Stem Cells 101: A Regenerative Powerhouse
What Are Stem Cells?
Stem cells are the body’s master builders raw, unspecialized cells that have the unique ability to develop into many different cell types. Think of them as nature’s repair crew, capable of replacing damaged cells, supporting healing, and regenerating tissue in areas where the body struggles to fix itself.
There are two main characteristics that set stem cells apart:
-
Self-renewal – they can make copies of themselves.
-
Differentiation – they can transform into specialized cells like neurons, muscle cells, or blood cells.
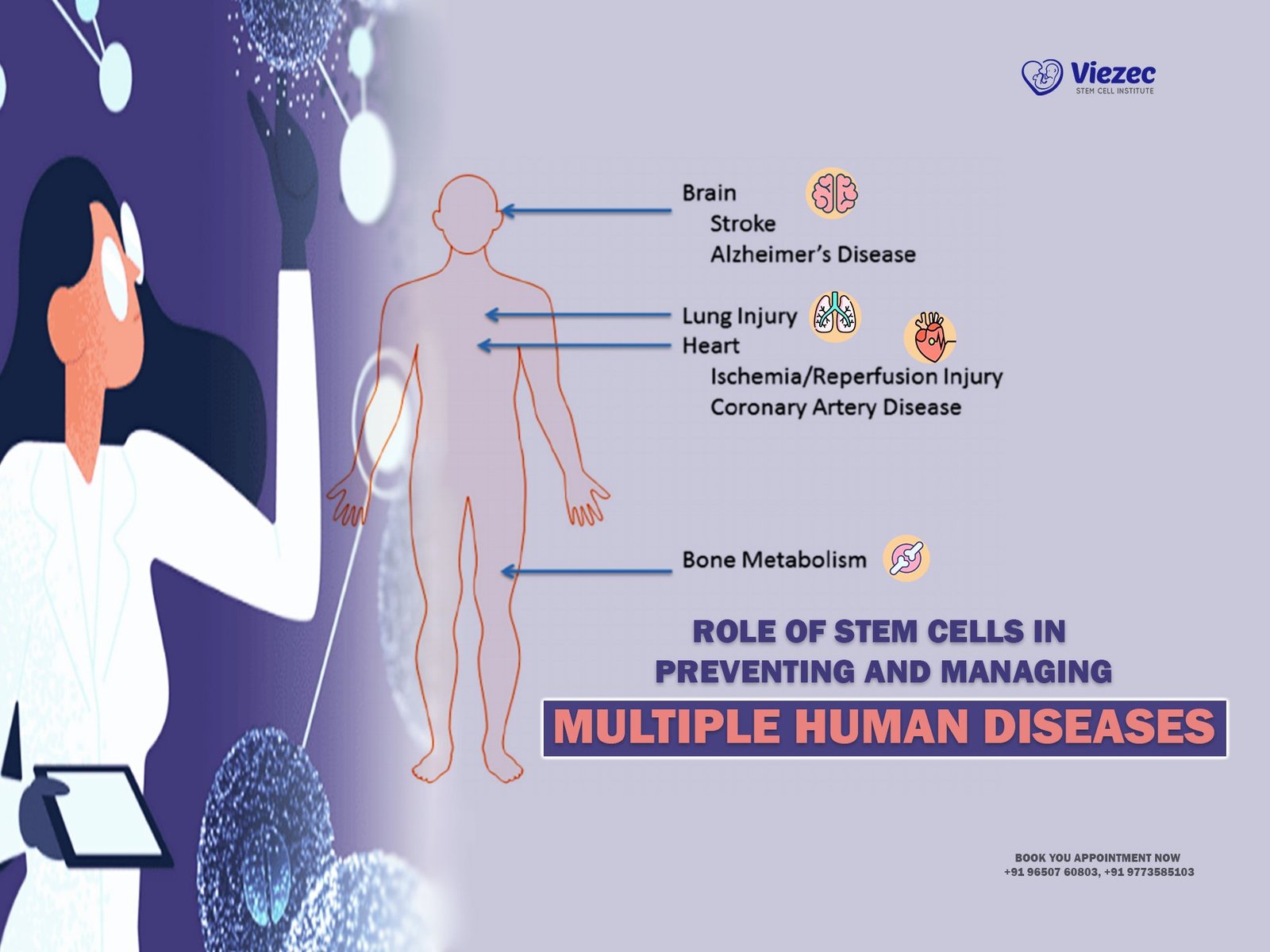
This ability to both multiply and adapt makes them incredibly valuable for treating a wide range of diseases—from spinal cord injuries to heart failure, and now, potentially, mental health disorders like depression.
The Main Types: Embryonic vs. Adult Stem Cells
Stem cells come in a few forms, each with different capabilities and considerations:
-
Embryonic Stem Cells (ESCs): These are pluripotent, meaning they can become virtually any cell in the body. They’re derived from early-stage embryos and have the greatest potential for regeneration—but also raise ethical and regulatory concerns.
-
Adult Stem Cells: More specifically, mesenchymal stem cells (MSCs) are a type of adult stem cell commonly used in medical research and therapy. Found in bone marrow, fat tissue, and umbilical cords, these cells are multipotent—able to become a limited range of cell types, including neurons and glial cells. Because they’re typically harvested from the patient or donor tissue, they come with fewer ethical issues and a lower risk of rejection.
How Stem Cells Could Help the Brain Heal
When it comes to depression, the real promise of stem cells lies in their potential to regenerate the brain’s internal landscape.
Here’s how they might work:
-
Promoting neurogenesis: They may stimulate the growth of new neurons, especially in areas like the hippocampus, which is often shrunken in people with depression.
-
Reducing inflammation: Chronic inflammation has been linked to mood disorders. Stem cells can release anti-inflammatory molecules that may calm this immune response.
-
Supporting connectivity: They might help repair or form new synaptic connections between neurons critical for healthy emotional regulation and cognitive function.
While the exact mechanisms are still being studied, early research suggests stem cells could address the biological underpinnings of depression, not just the symptoms.
Depression and the Brain: What’s Really Happening?
The Role of Neuroplasticity and Neurogenesis
The brain is not a static organ—it’s constantly changing, adapting, and reshaping itself through a process known as neuroplasticity. This flexibility allows us to learn new things, bounce back from setbacks, and form new memories. Alongside this, neurogenesis—the growth of new neurons, especially in the hippocampus—is essential for emotional resilience and cognitive clarity.
But in people with depression, these processes often slow down or stall entirely. Research shows that depression is linked to reduced neuroplasticity and impaired neurogenesis, particularly in brain regions responsible for emotion regulation, memory, and decision-making. Without the brain’s natural capacity to adapt and repair, negative thought patterns become deeply ingrained and harder to break.
Inflammation, Stress, and Neuron Loss
Depression isn’t just psychological—it has a biological footprint. One major factor? Chronic stress. When we’re under prolonged stress, the body releases high levels of cortisol, a hormone that, over time, can harm the brain.
This stress-induced damage contributes to:
-
Increased inflammation in the brain
-
Reduced connectivity between neurons
-
Loss of brain volume in areas like the prefrontal cortex and hippocampus
Neuroscientists are increasingly recognizing inflammation as a major player in mood disorders. Inflammatory markers are often elevated in people with depression, suggesting the immune system might be in overdrive, attacking the brain’s own cells and structures.
The Hidden Damage Chronic Depression Can Cause
Depression that lingers for years doesn’t just affect how someone feels—it can physically reshape the brain. Studies have linked long-term depression with:
-
Shrinkage in the hippocampus (memory center)
-
Thinning of the prefrontal cortex (decision-making and personality)
-
Lower white matter density (communication between brain regions)
This structural damage helps explain why depression can lead to trouble concentrating, memory issues, emotional numbness, and even slower movement or speech.
Why the Brain’s Ability to Regenerate Matters
Here’s where the concept of healing gets exciting: if the brain can regenerate, then recovery isn’t just possible—it’s biological.
That’s where stem cell therapy enters the picture. By boosting neurogenesis, dampening inflammation, and repairing damaged neural networks, stem cells offer hope for restoring what depression has worn down. Instead of just coping, patients could one day rebuild.
How Stem Cells Could Transform Depression Treatment
Encouraging Neural Growth and Rewiring
One of the most exciting potentials of stem cell therapy in depression is its ability to support the growth of new neurons and rebuild neural networks. In people struggling with chronic depression, the brain’s wiring often becomes rigid or degraded—especially in areas tied to emotion regulation, motivation, and memory.
Stem cells, particularly mesenchymal stem cells (MSCs), have shown the ability to:
-
Stimulate neurogenesis (the growth of new brain cells)
-
Enhance synaptic plasticity, helping the brain form new connections
-
Release growth factors like BDNF (brain-derived neurotrophic factor), which is crucial for healthy brain function
This kind of “rewiring” could restore emotional flexibility and reduce the cognitive fog many people experience with depression.
Reducing Inflammation and Rebalancing Brain Chemistry
There’s growing evidence that neuroinflammation is a key driver of depression, particularly in individuals who don’t respond well to standard treatments. Elevated levels of pro-inflammatory cytokines can interfere with serotonin production and disrupt communication between brain regions.
Stem cells offer a natural anti-inflammatory effect. They release molecules that calm immune overactivity in the brain, creating a more balanced and healing environment. This may help restore:
-
Serotonin and dopamine regulation (key mood-related neurotransmitters)
-
HPA axis function, which controls how we respond to stress
-
Overall mood stability and energy levels
In essence, stem cells may treat the source, not just the symptoms.
Repairing Emotional Circuitry Damaged by Trauma
Many cases of depression—especially those tied to early-life trauma, PTSD, or chronic stress—involve damage to specific areas of the brain, like the amygdala and hippocampus. These regions are responsible for processing emotion, fear, and memory.
Preliminary studies suggest stem cells may help rejuvenate these regions by:
-
Reducing trauma-related inflammation
-
Supporting the regrowth of healthy neural tissue
-
Improving emotional regulation and resilience
For those who feel stuck in cycles of fear, sadness, or emotional numbness, stem cells could offer a path toward deep and lasting recovery—not just management.
Final Thoughts: A New Era in Depression Treatment?
Hope, Hype, or Both?
Stem cell therapy is one of the most talked-about developments in modern medicine—and for good reason. It promises something that current depression treatments rarely do: the potential to repair and regenerate the brain, not just manage symptoms.
But while the excitement is real, it’s important to stay grounded. Most stem cell treatments for depression are still in the experimental phase, and large-scale clinical trials are needed to fully understand their safety, effectiveness, and long-term impact. There’s also the risk of commercial hype getting ahead of the science, especially with unregulated clinics offering unproven therapies.
That said, even cautious experts agree: we’re on the cusp of something big. Stem cells represent a fundamental shift in how we think about mental illness—from a lifelong condition to something potentially treatable at the root level.
What Patients Should Know Before Considering Stem Cell Therapy
If you’re exploring stem cell therapy as an option, here are a few things to keep in mind:
-
Do your research: Only consider clinics and providers involved in clinical trials or backed by peer-reviewed evidence. Be wary of bold claims without scientific backing.
-
Talk to a trusted healthcare provider: Your doctor can help you evaluate the risks and benefits in the context of your unique medical history.
-
Understand the limitations: While promising, stem cell therapy is not yet FDA-approved for depression, and most insurance plans won’t cover it.
-
Stay hopeful, but realistic: Keep an open mind to emerging science, but avoid quick fixes. The best breakthroughs often take time.
Exploring Stem Cell Treatment for Depression in India
For individuals struggling with depression—especially those who haven’t found relief through conventional methods—stem cell therapy may offer a beacon of hope. And for those exploring treatment options outside of their home country, India is quickly emerging as a global hub for regenerative medicine.
Why India?
India offers a unique combination of cutting-edge medical infrastructure, internationally accredited clinics, and cost-effective treatment options. Stem cell therapy in India is guided by evolving ethical standards and scientific rigor, with many providers offering advanced care at a fraction of the cost compared to Western countries.
Patients considering medical travel for depression treatment will find that India provides:
-
Skilled specialists in regenerative and psychiatric medicine
-
Personalized treatment protocols based on the latest research
-
Comprehensive support services for international patients
-
Affordability, often with transparent package pricing
Viezec: A Trusted Partner in Regenerative Medicine
One of the leading providers in this space is Viezec Stem Cell Institute. Known for its patient-first approach, Viezec collaborates with top-tier hospitals and research labs to offer advanced stem cell therapy for depression and other neurological disorders.
Here’s what sets Viezec apart:
-
Use of ethically sourced mesenchymal stem cells (MSCs) with proven safety profiles
-
A focus on treatment-resistant and chronic depression cases
-
End-to-end care, including travel coordination, pre-treatment consultation, and post-treatment follow-up
-
A multidisciplinary team of neurologists, psychiatrists, and regenerative specialists
Viezec’s mission is to help patients not only manage their symptoms—but reclaim their lives through scientifically supported, regenerative care.