Key Takeaways
- 01. Target condition defined:
The article defines sensorineural hearing loss as damage to the inner ear’s hair cells or auditory nerve, which traditional treatments cannot regenerate. - 02. Therapy goal explained:
The treatment uses stem cells to regenerate damaged hair cells and support neural pathways in the inner ear, aiming to restore hearing function. - 03. Experimental status emphasized:
The blog highlights that stem cell therapy for this hearing condition remains experimental, with no large-scale approved clinical trials or guaranteed outcomes. - 04. Indian context highlighted:
India offers access to this therapy through clinics in Delhi and other centres. Details on cost and protocols are available, but patients are advised to consider standard care alongside regenerative options.
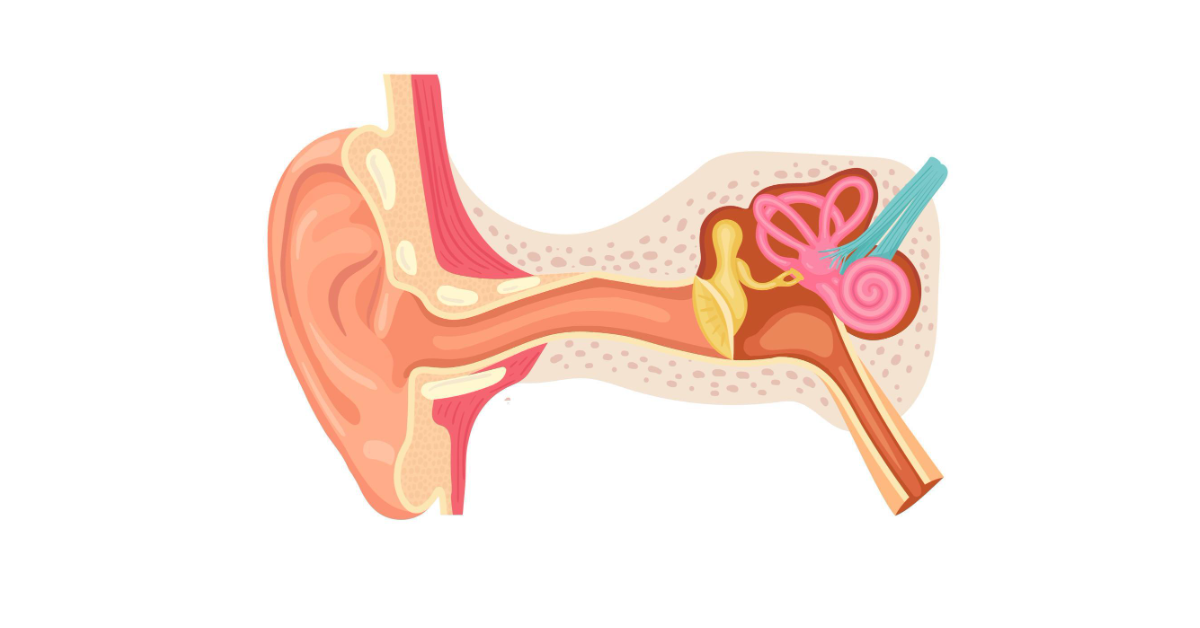
Sensorineural hearing loss (SNHL) primarily affects the inner ear or the pathways connecting the inner ear to the brain. It is linked to damage in the tiny hair-like cells of the cochlea or the auditory nerve that carries sound signals to the brain. When these specialized cells or pathways are damaged, the ability to hear clearly or interpret sounds is compromised. This type of hearing loss results from a reduction in sound level, as well as an inability to hear faint sounds or differentiate between certain speech sounds, making communication challenging.
The inner ear plays a vital role in our ability to hear. The cochlea, a snail-shaped organ filled with fluid and tiny hair cells, is responsible for converting sound waves into electrical impulses. The brain then interprets these impulses as sound. In sensorineural hearing loss, the hair cells may no longer function properly. Because these cells do not regenerate in humans, hearing loss tends to be permanent, differing significantly from conductive hearing loss, which affects the outer or middle ear.
SNHL can range from mild to profound. Mild sensorineural hearing loss might make soft conversations difficult to understand, while severe cases can make hearing almost impossible without amplification devices. The degree and frequency range of hearing loss vary among individuals, affecting one’s perception of high-pitched or low-pitched sounds. Additionally, clarity in speech recognition can be particularly affected, often making conversations in noisy environments especially challenging.
An interesting aspect of SNHL is that it can affect one or both ears. Unilateral sensorineural hearing loss affects just one ear, impacting a person’s ability to localize sound or understand speech in a noisy setting. Bilateral SNHL impacts both ears and can pose significant challenges to hearing and communication. Sometimes, sensorineural hearing loss may have a stable effect, while in other cases, it can progress over time, leading to further challenges in understanding sounds and speech.
When it comes to managing everyday life, individuals with sensorineural hearing loss often experience the world differently. Background noise can feel overwhelming, and distinguishing specific sounds may require more effort. In conversations, for example, comprehending speech may be difficult if multiple people are talking simultaneously. Sounds may seem muffled or distorted, making communication a source of frustration. This loss of auditory detail can also lead to feelings of isolation in social settings, as engagement becomes more taxing.
Cultural and social impacts are also worth noting. Individuals with SNHL may need to make adjustments in their personal and professional lives. The use of visual cues, like lip-reading and body language, becomes increasingly important for effective communication. The challenges they face can influence emotional well-being, leading to a greater emphasis on developing strategies to interact with others and fully engage with the environment. Technology, like hearing aids or assistive listening devices, has improved the ability of many to interact with their surroundings, though it does not restore hearing perfectly.
Additionally, sensorineural hearing loss can influence how individuals perceive music and environmental sounds. Subtleties like the richness of music, nuances in voice tones, or the gentle rustling of leaves may be harder to notice. The sense of balance may also be affected in some cases, as the inner ear plays a key role in equilibrium. People experiencing SNHL may require time to adapt to these sensory differences and learn new ways to engage with auditory experiences.
SNHL also plays a significant role in the way people approach communication strategies. Some individuals use techniques like positioning themselves closer to speakers, avoiding noisy environments, or utilizing specialized auditory training. Advances in communication technology, such as captioning services and real-time translation, have further facilitated smoother interactions. Family members and friends often play a supportive role, contributing to better overall quality of life and helping those with sensorineural hearing loss feel more connected and understood.
Sensorineural symptoms originate from issues within the sensory pathways, particularly related to nerve damage or dysfunction affecting the transmission of signals from sensory organs to the brain. These symptoms commonly involve the auditory and vestibular systems, but they can also impact other senses like vision and balance. The main cause of sensorineural symptoms is usually damage to the hair cells in the inner ear, the auditory nerve, or related neural pathways in the brain.
1. Hearing Loss
Sensorineural hearing loss (SNHL) is one of the most common manifestations. It occurs when the inner ear (cochlea) or the auditory nerve pathway to the brain becomes damaged. This hearing loss is usually permanent. Common causes include aging, noise exposure, infections, head trauma, and certain medications. Individuals with SNHL may find it hard to hear soft sounds and have difficulty understanding speech, even in quiet environments.
2. Tinnitus
Tinnitus, or a ringing, buzzing, or hissing sound in the ears, is another common sensorineural symptom. It is often related to nerve damage in the auditory system. Tinnitus can range from mild, occasional sounds to severe, persistent noise that disrupts daily activities. Chronic exposure to loud noise, age-related hearing loss, and ear infections are typical triggers. The brain’s response to missing auditory input is believed to contribute to tinnitus.
3. Dizziness and Vertigo
Sensorineural symptoms can also involve dizziness or vertigo, which are linked to issues with the vestibular system in the inner ear. Vertigo is the sensation of spinning or feeling off-balance. Vestibular neuronitis, Meniere’s disease, and labyrinthitis are conditions often associated with these symptoms. Dizziness may be accompanied by nausea, vomiting, and difficulties with coordination or balance.
4. Balance Problems
Problems with the vestibular system can cause unsteadiness or difficulty maintaining balance. Balance issues may worsen in dark environments, where visual cues are absent, or on uneven surfaces. Individuals may feel a sense of disequilibrium, and in severe cases, these symptoms may lead to falls. Balance dysfunction is common in older adults as part of the natural aging process or as a consequence of inner ear damage.
5. Auditory Processing Disorders
Even when the ability to detect sounds remains intact, sensorineural damage can cause auditory processing disorders. People may struggle to make sense of spoken language, especially in noisy settings. This is due to issues with the brain’s ability to interpret or process sound signals correctly. Common difficulties include misunderstanding conversations and poor localization of sound sources.
6. Hyperacusis
Hyperacusis refers to heightened sensitivity to normal environmental sounds. People experiencing this symptom may find everyday noises painfully loud or uncomfortable. It is often associated with damage to the auditory nerve or inner ear structures. Chronic noise exposure, head trauma, or certain neurological conditions can lead to hyperacusis. Living with this symptom can be challenging and affect social interactions.
7. Reduced Speech Discrimination
Reduced speech discrimination involves difficulty distinguishing between similar speech sounds. Even when sounds are loud enough, people may find it hard to understand conversations. It occurs when the brain’s processing of auditory information is impaired. This symptom is commonly observed in older adults and individuals exposed to ototoxic drugs or chronic noise.
8. Sensory Disintegration
Sensorineural damage can sometimes cause sensory disintegration, where multiple senses fail to work together seamlessly. For example, the brain may have trouble integrating visual and vestibular inputs, leading to difficulties in balance and orientation. This symptom can complicate tasks requiring hand-eye coordination and can contribute to a general sense of confusion or disorientation.
9. Visual Sensorineural Symptoms
In some cases, sensorineural symptoms may affect vision. This can include blurred vision, difficulty focusing, or impaired depth perception. These issues often arise from neural pathways or vestibular dysfunction, as the visual and vestibular systems are closely linked. People may experience visual disturbances when moving their heads or when in motion.
10. Cognitive and Emotional Impact
Persistent sensorineural symptoms can lead to cognitive and emotional difficulties. Hearing loss or chronic dizziness can cause fatigue, stress, and even depression. Individuals may find it hard to concentrate, and the constant effort to understand speech or maintain balance can be mentally exhausting. Social isolation is a significant risk, particularly for those with hearing or balance issues.
Understanding sensorineural symptoms is essential for accurate diagnosis and management. Treatment options may include hearing aids, cochlear implants, balance therapy, or medications to manage vertigo and tinnitus. Ongoing research aims to develop advanced interventions to restore or compensate for lost sensorineural function.
Sensorineural hearing loss (SNHL) is a type of hearing impairment resulting from damage to the inner ear or the auditory nerve pathways. The term “sensorineural” combines the words “sensory” (relating to the sensory cells of the inner ear) and “neural” (referring to the nerve pathways to the brain). Understanding the causes of SNHL is crucial because it affects treatment options and management strategies. Below are the detailed causes of sensorineural hearing loss:
1. Aging (Presbycusis)
Aging, also known as presbycusis, is one of the most common causes of SNHL. As people grow older, the hair cells within the cochlea (the organ of hearing) gradually deteriorate. These cells cannot regenerate, leading to permanent hearing loss. Typically, age-related hearing loss affects higher frequencies first and progresses gradually. Environmental factors, such as prolonged exposure to loud sounds, may accelerate this process. Genetic factors also play a role in the rate and extent of presbycusis. Managing presbycusis usually involves hearing aids to improve communication and enhance the quality of life.
2. Noise Exposure
Repeated exposure to loud noise can damage the hair cells in the cochlea, leading to noise-induced hearing loss. This type of SNHL can occur from occupational noise (e.g., construction work, factory noise), recreational noise (e.g., concerts, loud music), or even sudden, extremely loud sounds (e.g., gunshots or explosions). The extent of damage depends on the volume, duration, and frequency of exposure. Hearing loss caused by noise exposure is often preventable with ear protection and limiting exposure to harmful noise levels. Once damage occurs, however, it is irreversible.
3. Genetic Factors
Genetic predisposition is a significant cause of sensorineural hearing loss. Mutations in specific genes can lead to congenital or progressive hearing loss. Some children are born with genetic forms of hearing loss, while others may develop it later in life. The loss can be syndromic (associated with other medical conditions, such as Usher syndrome or Waardenburg syndrome) or nonsyndromic (hearing loss is the only symptom). Genetic counseling can help families understand the risk factors and the likelihood of transmission to offspring. In some cases, cochlear implants or hearing aids can help.
4. Infections
Certain infections can lead to sensorineural hearing loss. Viral infections such as measles, mumps, rubella, cytomegalovirus, and even influenza can damage the inner ear structures. Bacterial infections, like meningitis, can also result in significant hearing impairment. Some of these infections affect hearing during fetal development if a mother contracts the infection during pregnancy, while others may impact hearing after birth. Vaccinations and good prenatal care can help reduce the risk of infection-related hearing loss. Treatment focuses on managing the hearing loss, often through assistive devices or rehabilitation.
5. Ototoxic Medications
Certain medications are known to be ototoxic, meaning they can damage the inner ear and lead to SNHL. These drugs include some antibiotics (like aminoglycosides), chemotherapy agents (such as cisplatin), diuretics, and high doses of aspirin. The risk depends on the type of drug, dosage, and duration of use. Sometimes, hearing loss caused by ototoxic medications is reversible, but in many cases, the damage is permanent. Patients taking potentially ototoxic medications are monitored for hearing loss, and alternative treatments may be considered if hearing impairment is detected early.
6. Head Trauma
Severe head injuries can lead to damage to the inner ear or auditory nerve, causing sudden sensorineural hearing loss. Trauma from car accidents, falls, or sports injuries may fracture the temporal bone or cause inner ear hemorrhage, disrupting normal hearing. In some cases, damage to the auditory nerve pathways in the brain may occur. Symptoms of hearing loss may present immediately after the injury or develop over time. Treatment options depend on the severity of the damage, and while some cases improve with medical intervention, others may result in permanent hearing loss.
7. Autoimmune Inner Ear Disease (AIED)
Autoimmune Inner Ear Disease is a rare condition where the body’s immune system mistakenly attacks the inner ear. This can lead to progressive hearing loss and balance problems. The onset is typically rapid, with hearing loss occurring over weeks or months. Early diagnosis is crucial to prevent further hearing damage. Treatment may involve corticosteroids or other immunosuppressive medications to reduce inflammation. Hearing aids or cochlear implants may be necessary for those with significant hearing loss. Monitoring and ongoing care are vital to managing AIED effectively and preserving as much hearing as possible.
8. Meniere’s Disease
Meniere’s disease is an inner ear disorder that causes episodes of vertigo, tinnitus (ringing in the ears), and fluctuating hearing loss. It is often associated with a buildup of fluid in the inner ear. The exact cause of Meniere’s disease is unknown, but it may be related to viral infections, genetic predisposition, or autoimmune responses. The hearing loss associated with Meniere’s disease is often progressive, worsening over time. While there is no cure, treatments focus on managing symptoms. Medications, lifestyle changes, and in severe cases, surgery may help control vertigo and slow hearing deterioration.
9. Tumors (Acoustic Neuroma)
Acoustic neuroma, also known as vestibular schwannoma, is a benign tumor that develops on the vestibulocochlear nerve. This nerve connects the inner ear to the brain and is responsible for hearing and balance. As the tumor grows, it compresses the nerve, leading to hearing loss, tinnitus, and balance issues. Early diagnosis is essential to prevent further complications. Treatment may involve monitoring, surgical removal, or radiation therapy. While hearing loss from an acoustic neuroma is often permanent, early intervention can help manage other symptoms and improve quality of life.
10. Other Medical Conditions
Several systemic diseases can also cause sensorineural hearing loss. Conditions like diabetes, multiple sclerosis, and stroke can affect the auditory nerve or blood flow to the inner ear, impairing hearing. Metabolic disorders, such as thyroid disease or kidney problems, may also have a negative impact on hearing. Additionally, autoimmune diseases like lupus or rheumatoid arthritis can lead to inner ear damage. Managing the underlying condition often helps stabilize hearing loss, but sometimes, assistive devices like hearing aids or cochlear implants may be necessary to improve communication.
Understanding the various causes of sensorineural hearing loss is essential for diagnosis and treatment. While some forms of SNHL are preventable or manageable, others require lifelong management and adaptation. Regular hearing assessments and protective measures, like avoiding loud noises, are crucial in maintaining good auditory health.
Sensorineural hearing loss (SNHL) results from inner ear damage or issues with the auditory nerve. Diagnosing this type of hearing loss involves understanding its causes, identifying symptoms, and using specialized tests to evaluate hearing function accurately. Here’s a detailed overview of the diagnostic process.
1. Recognizing Symptoms of Sensorineural Hearing Loss
Individuals with SNHL often notice muffled hearing, difficulty understanding speech in noise, and a decreased ability to hear high-pitched sounds. People might complain of tinnitus (ringing in the ears), dizziness, or balance problems. Difficulty understanding conversations, especially in crowded areas, is common. Sudden hearing loss is also a warning sign, requiring immediate medical attention. Accurate diagnosis starts with identifying these symptoms and understanding their impact on daily life. A thorough medical and auditory history provides clues to the hearing loss’s underlying causes.
2. Detailed Medical History
Taking a comprehensive medical history is crucial for diagnosing SNHL. Physicians inquire about past illnesses, noise exposure, and family history of hearing loss. Details about ear infections, head trauma, and any medications taken are also noted. Some drugs, known as ototoxic medications, can damage the inner ear, contributing to SNHL. Genetic predispositions are considered, especially if hearing loss occurs at a young age or has affected other family members. Gathering this information gives insight into potential causes, guiding subsequent tests to narrow down the exact nature of the hearing impairment.
3. Physical Examination of the Ear
A physical examination helps identify obvious issues, like wax buildup or outer ear deformities, that could contribute to hearing loss. An otoscope is used to check the ear canal and eardrum for abnormalities, signs of infection, or damage. Although SNHL typically affects the inner ear or auditory nerve, a physical exam rules out any external or middle ear problems that may mimic sensorineural symptoms. Physicians also inspect for any abnormalities that may indicate broader neurological issues, which could require additional investigations.
4. Audiometric Testing
Audiometric testing is a key component in diagnosing SNHL. An audiologist performs a series of hearing tests, including pure-tone audiometry, speech audiometry, and bone conduction testing. Pure-tone audiometry measures hearing sensitivity across various frequencies, while speech audiometry evaluates how well a person understands spoken words. Bone conduction tests bypass the outer and middle ear, assessing the inner ear directly. The results are plotted on an audiogram, showing the extent and pattern of hearing loss, helping distinguish between sensorineural and other types of hearing loss.
5. Otoacoustic Emissions (OAE) Testing
Otoacoustic emissions (OAE) testing measures the inner ear’s response to sound. When the cochlea (inner ear) functions properly, it produces low-level sound emissions in response to an auditory stimulus. A small probe is placed in the ear canal, which emits sound waves and records the cochlea’s response. Absence or reduction of these emissions suggests damage to the hair cells in the cochlea, which is characteristic of SNHL. OAE testing is especially useful for newborn hearing screening and assessing cochlear function without requiring active responses from the patient.
6. Auditory Brainstem Response (ABR) Testing
Auditory Brainstem Response (ABR) testing evaluates the hearing nerve’s function. Electrodes are placed on the scalp to measure the electrical activity generated by the auditory nerve and brainstem in response to sound. ABR testing is crucial for diagnosing hearing loss in infants or patients who cannot participate in conventional audiometric tests. It can also detect tumors along the auditory nerve pathway or confirm neural pathway integrity. The results help differentiate between cochlear and neural causes of hearing loss, guiding further diagnostic or treatment steps.
7. Imaging Studies: CT and MRI Scans
For more complex cases, imaging studies like computed tomography (CT) or magnetic resonance imaging (MRI) may be necessary. These scans provide detailed images of the inner ear structures, auditory nerve, and surrounding brain tissues. CT scans are useful for identifying congenital malformations or bone abnormalities, while MRI scans are preferred for soft tissue visualization. Imaging can reveal tumors, such as acoustic neuromas, or damage due to trauma. These diagnostic tools are particularly helpful when hearing loss is unilateral (in one ear) or accompanied by neurological symptoms like dizziness or balance disturbances.
8. Electrocochleography (ECoG) Testing
Electrocochleography (ECoG) measures the electrical potentials generated in the cochlea and auditory nerve in response to sound stimuli. This test helps detect inner ear fluid imbalances, like in Ménière’s disease, or other disorders affecting the cochlea. It involves placing electrodes on the scalp and, in some cases, near the eardrum to record responses. ECoG is not commonly used for general hearing loss diagnosis but provides valuable information for specific conditions where fluid pressure or electrical dysfunction in the inner ear is suspected.
9. Genetic Testing for Inherited Hearing Loss
When hearing loss is suspected to have a genetic cause, genetic testing becomes essential. It identifies mutations linked to hereditary forms of SNHL, which are common in congenital or early-onset hearing loss. Genetic counseling follows the test results, helping families understand the implications, recurrence risks, and potential interventions. This type of testing is particularly beneficial when hearing loss occurs with no apparent environmental cause or when there are other signs of genetic syndromes. Knowing the genetic basis of hearing loss aids in counseling, treatment planning, and sometimes predicting disease progression.
10. Balancing and Vestibular Function Testing
Because SNHL can be associated with balance issues, tests like videonystagmography (VNG) and vestibular evoked myogenic potential (VEMP) are performed. These assess the balance system, which includes the inner ear structures. VNG measures eye movements in response to visual or positional stimuli, while VEMP tests the vestibular (balance) pathways. Balance testing is crucial if a patient reports dizziness or vertigo, symptoms often linked to inner ear disorders. Understanding the connection between hearing and balance issues ensures a more comprehensive diagnosis and informs appropriate treatment options.
Accurately diagnosing sensorineural hearing loss involves a series of detailed and specialized assessments. Audiometric tests, advanced imaging, and genetic testing provide a complete understanding of hearing impairment. Early diagnosis is critical to managing and treating SNHL effectively, which improves quality of life. If you or someone you know is experiencing hearing loss symptoms, consult with a healthcare professional for proper assessment and guidance.
Stem cell therapy is an emerging treatment that offers hope for individuals with sensorineural hearing loss, a condition caused by damage to the inner ear or auditory nerve. Sensorineural hearing loss is typically irreversible, as the hair cells in the cochlea do not regenerate naturally. Stem cell therapy aims to regenerate or repair these damaged structures, restoring hearing capabilities. Here’s an in-depth look at how the procedure works, the science behind it, and what patients might expect:
Understanding Sensorineural Hearing Loss
Sensorineural hearing loss occurs when there’s damage to the hair cells in the cochlea, the auditory nerve, or the auditory pathways in the brain. It is often caused by aging, exposure to loud noise, infections, or genetic factors. Traditional treatments include hearing aids or cochlear implants, which do not restore natural hearing but assist in sound amplification and processing. Stem cell therapy, however, aims to regenerate these damaged parts and restore hearing.
How Stem Cell Therapy Works
Stem cell therapy uses the unique properties of stem cells, which can develop into various types of specialized cells. In sensorineural hearing loss, the goal is to regenerate the hair cells or auditory nerve cells that have been damaged. The two primary sources of stem cells used in this therapy are embryonic stem cells and adult stem cells, such as mesenchymal stem cells (MSCs) derived from bone marrow or adipose tissue. These cells are injected into the cochlea or inner ear, where they can differentiate into hair cells or neurons.
Types of Stem Cells Used
- Embryonic Stem Cells: These cells are pluripotent and can develop into any cell type, making them highly versatile. They are extracted from embryos, which has ethical concerns but high regenerative potential.
- Adult Stem Cells (Mesenchymal Stem Cells): These cells are multipotent, meaning they can develop into several but not all types of cells. They are harvested from the patient’s bone marrow, fat tissue, or even the umbilical cord.
- Induced Pluripotent Stem Cells (iPSCs): These are adult cells reprogrammed to behave like embryonic stem cells. They offer fewer ethical concerns and have broad applicability.
The Stem Cell Procedure
- Harvesting Stem Cells: If adult stem cells are used, they are extracted from the patient’s bone marrow or adipose tissue under local anesthesia. If embryonic stem cells or iPSCs are used, they are prepared in a lab setting.
- Cell Preparation: The harvested stem cells are processed and purified in a lab to ensure they are viable and ready for therapeutic use. This step includes culturing the cells to increase their numbers and programming them to differentiate into hair cells or neurons.
- Injection into the Cochlea: The inner ear is accessed surgically, and the stem cells are injected directly into the cochlea. The procedure is delicate, and precision is crucial to avoid further damage. Sometimes, stem cells are injected into the bloodstream, but this is less common for hearing loss treatments.
- Monitoring and Rehabilitation: After the injection, the patient is monitored for cell integration and hearing improvements. Rehabilitation, including hearing tests and auditory training, may be part of the recovery process.
Mechanism of Action
Once injected into the cochlea, the stem cells work by:
- Regenerating Hair Cells: Stem cells can differentiate into hair cells that replace the damaged ones in the cochlea, improving the ear’s ability to convert sound vibrations into electrical signals for the brain.
- Repairing the Auditory Nerve: For some patients, stem cells can regenerate damaged auditory nerve fibers, improving the transmission of sound signals to the brain.
- Reducing Inflammation and Promoting Healing: Stem cells can release anti-inflammatory factors, enhancing the healing environment in the inner ear.
Stem cell therapy for sensorineural hearing loss is a promising but experimental treatment. It has the potential to regenerate damaged hair cells and repair the auditory nerve, potentially restoring natural hearing. However, more research and clinical trials are needed before it becomes widely available. As the science progresses, individuals with hearing loss may soon have new treatment options that could improve their quality of life. If you are interested, consult a specialist to explore the latest advancements in stem cell therapy for hearing restoration.
Stem cells have unique regenerative properties that hold the potential to replace damaged or lost inner ear cells. The idea is that stem cells, which can differentiate into various cell types, can be used to regenerate or repair cochlear hair cells and auditory neurons. By doing so, they offer the possibility of restoring hearing. Scientists have made significant progress in understanding how to coax stem cells to develop into hair cells and integrate successfully into the inner ear.
Types of Stem Cells Used
Several types of stem cells are being explored for hearing restoration:
- Embryonic Stem Cells (ESCs): These are pluripotent cells that can become any type of cell in the body. They have shown promise in regenerating inner ear structures in lab settings.
- Induced Pluripotent Stem Cells (iPSCs): These are adult cells reprogrammed to a pluripotent state. They are valuable for personalized treatment and have been used to generate hair cells in studies.
- Mesenchymal Stem Cells (MSCs): Found in bone marrow and fat tissue, MSCs have anti-inflammatory and protective effects. They are being tested for their ability to promote hearing recovery through the release of healing factors.
How Stem Cell Treatment Works
The process involves harvesting stem cells, either from the patient or a donor, and cultivating them to become the desired cell type, such as hair cells or neurons. These cells are then introduced into the cochlea or surrounding areas, where they aim to integrate and function as the original cells. This integration could restore the auditory pathway and improve hearing. Early trials focus on ensuring that stem cells can survive, differentiate, and form functional connections with auditory nerves.
Stem cell therapy represents a beacon of hope for those with sensorineural hearing loss. Although it’s still in the experimental stages, ongoing research and trials are paving the way for potentially groundbreaking treatments. For now, hearing aids and cochlear implants remain the standard, but with continued advancements, a world where natural hearing can be restored may not be too far away. Keep an eye on emerging clinical studies to stay informed about the latest in hearing restoration breakthroughs.
Would you like more information on clinical trials, research centers, or expert interviews? Feel free to ask!
Stem cell implantation for sensorineural hearing loss in India has emerged as a promising therapy, with research showing its potential to regenerate auditory hair cells and neurons in the cochlea. These cells are crucial for converting sound vibrations into neural signals, which are often damaged in sensorineural hearing loss.
How It Works
The procedure involves collecting stem cells, typically from the patient’s bone marrow or fat tissue. In infants, umbilical cord stem cells are preferred. These cells are then purified in a lab and implanted into the inner ear. They differentiate into functional auditory cells, aiming to restore hearing over time.
Success Rates and Benefits
Early research and clinical trials have shown success rates between 85% and 95%. Many patients report significant improvements, with some seeing faster results than others. The treatment is relatively low-risk and minimally invasive, without long-term side effects. However, it remains experimental, as large-scale clinical trials are still ongoing.
Costs and Availability
In India, the cost of stem cell therapy for hearing loss depend on many actors like the clinic, type of stem cells used, and number of sessions influence the overall expense. India stands out as a hub for medical tourism, offering top-tier facilities at competitive prices compared to Western nations.
While stem cell therapy offers hope, it is essential to weigh its experimental nature and consult specialists for tailored advice.
Stem cell therapy is a promising approach for sensorineural hearing loss (SNHL), a condition where damage occurs to the hair cells, auditory nerve, or other structures in the inner ear. The core mechanisms involve regeneration and repair of damaged or lost cells within the auditory system. Understanding how stem cells work in this context provides hope for reversing or mitigating hearing loss.
Types of Stem Cells Used
Stem cells used for treating sensorineural hearing loss mainly include embryonic stem cells, mesenchymal stem cells (MSCs), and induced pluripotent stem cells (iPSCs). These stem cells possess the unique ability to self-renew and differentiate into various cell types, including inner ear sensory cells and neurons. The choice of stem cells depends on the therapeutic goals, such as regenerating hair cells or repairing damaged auditory neurons.
- Embryonic Stem Cells (ESCs): These are pluripotent cells derived from early-stage embryos. ESCs can differentiate into any cell type, including hair cells and supporting cells in the cochlea. However, their use raises ethical concerns and potential risks, such as tumor formation.
- Mesenchymal Stem Cells (MSCs): Derived from bone marrow, adipose tissue, or umbilical cord blood, MSCs are multipotent cells capable of differentiating into various tissues. MSCs secrete bioactive molecules that reduce inflammation, promote tissue repair, and support cell regeneration in the cochlea.
- Induced Pluripotent Stem Cells (iPSCs): These are adult cells reprogrammed to a pluripotent state, enabling them to become any cell type. iPSCs are genetically similar to the patient’s cells, minimizing the risk of immune rejection. They can be used to generate inner ear cells for personalized treatment.
Mechanism of Action
The mechanism of stem cell therapy for SNHL involves several steps:
- Cell Replacement and Regeneration: The primary goal is to replace lost or damaged hair cells in the cochlea. Stem cells can differentiate into hair cell-like cells and integrate into the cochlear structure, restoring the function of sound transmission. This process involves the transformation of stem cells into progenitor cells, which further differentiate into mature hair cells.
- Neuroprotection and Repair: Besides replacing hair cells, stem cells help in repairing the auditory nerve. The secretion of neurotrophic factors by MSCs or iPSCs supports the survival and growth of auditory neurons. This repair mechanism enhances the connection between hair cells and the auditory nerve, improving signal transmission to the brain.
- Paracrine Effects: Stem cells release various growth factors, cytokines, and exosomes that create a regenerative microenvironment. These paracrine factors modulate inflammation, reduce oxidative stress, and promote cell survival and tissue healing. They play a crucial role in cochlear repair and regeneration.
- Immune Modulation: Stem cells have the ability to modulate the immune response, preventing excessive inflammation that can further damage inner ear structures. This immune-modulatory effect is crucial in creating a conducive environment for tissue regeneration and reducing chronic inflammation that might impede healing.
The ultimate goal is to develop safe and effective stem cell-based therapies that can restore hearing and improve the quality of life for those with sensorineural hearing loss. Advances in genetic engineering and bioinformatics are expected to accelerate progress in this field, making stem cell therapy a viable option for auditory restoration.
Sensorineural hearing loss (SNHL) is the most common type of permanent hearing loss, caused by damage to the inner ear structures, specifically the hair cells within the cochlea, or to the auditory nerve. Traditionally, SNHL treatments have been limited to hearing aids or cochlear implants. However, advancements in regenerative medicine, particularly stem cell therapy, have sparked hope for restoring hearing by repairing or regenerating damaged cells in the auditory system.
How Stem Cell Therapy Works for SNHL
Stem cell therapy aims to repair damaged inner ear structures by using the regenerative capabilities of stem cells. These cells can transform into various specialized cell types, such as hair cells or neurons, and help restore lost functions. The goal is to replace or rejuvenate damaged or lost hair cells in the cochlea or regenerate the auditory nerve.
Improvements Observed After Stem Cell Therapy
1. Hearing Function Enhancement
Several clinical studies and experimental models have shown significant improvements in hearing thresholds. Patients and animal models have demonstrated partial restoration of hearing sensitivity. In some cases, improved hearing thresholds were measurable on audiograms. These findings suggest that stem cells can successfully regenerate hair cells in the cochlea, contributing to improved sound detection.
2. Tinnitus Reduction
Individuals with SNHL often suffer from tinnitus, a persistent ringing or buzzing sound in the ears. Stem cell therapy has been reported to reduce the severity of tinnitus symptoms. As damaged hair cells and nerve pathways are repaired or replaced, the abnormal auditory signals associated with tinnitus can decrease, providing relief to patients.
3. Improved Speech Recognition
Another notable improvement after stem cell therapy is better speech recognition. People with SNHL often struggle to understand speech, especially in noisy environments. By regenerating damaged hair cells and enhancing synaptic connections, stem cell therapy has shown the potential to improve the clarity of speech and overall sound processing, making conversations easier to follow.
4. Regeneration of Cochlear Hair Cells
Animal studies have demonstrated the regeneration of cochlear hair cells following stem cell injections. These new hair cells are critical for translating sound waves into electrical signals sent to the brain. The reestablishment of functional hair cells contributes to improved hearing capabilities and helps prevent further auditory deterioration.
5. Neuroprotection and Synaptic Restoration
Stem cell therapy is believed to offer neuroprotective benefits, safeguarding the auditory nerve and restoring synaptic connections between hair cells and nerve fibers. This not only improves hearing but also helps maintain the integrity of the auditory pathway. Some studies have shown restored synaptic connections, leading to better sound signal transmission to the brain.
Stem cell therapy represents a groundbreaking approach to treating sensorineural hearing loss. While significant progress has been made, ongoing research is needed to fine-tune the technology and make it widely accessible. For now, the observed improvements—such as enhanced hearing thresholds, reduced tinnitus, and better speech recognition—provide hope for a future where hearing loss can be effectively treated through regenerative medicine.
At Viezec, we understand the profound impact that sensorineural hearing loss can have on an individual’s life. That’s why we are dedicated to providing advanced stem cell therapy to help address this condition. Our promise is to offer cutting-edge, scientifically-backed treatments with a focus on restoring hearing and improving quality of life for our patients. Here’s what sets our stem cell therapy for sensorineural hearing loss apart:
1. State-of-the-Art Stem Cell Technology
We utilize the most recent advancements in stem cell research to provide patients with a promising solution to sensorineural hearing loss. Our stem cell therapy uses mesenchymal stem cells (MSCs), which have shown significant potential in regenerating damaged sensory cells in the inner ear. These cells are carefully harvested, cultured, and prepared for use in treating hearing impairments. Our approach is designed to target the root cause of the condition, repairing and regenerating damaged tissues in the cochlea, and promoting overall hearing recovery.
2. Personalized Treatment Plans
At Viezec, we believe in offering personalized treatment plans tailored to the unique needs of each patient. We understand that no two cases of sensorineural hearing loss are the same, so our team of specialists works closely with you to assess your condition and recommend the most effective stem cell therapy plan. Through comprehensive diagnostic testing and consultations, we ensure that our treatments are the best fit for your specific hearing restoration goals.
3. Comprehensive Care from Start to Finish
We’re committed to guiding you through the entire stem cell therapy process, from the initial consultation to post-treatment recovery. Our multidisciplinary team of experts provides ongoing support, monitoring your progress and ensuring the best possible outcome. At Viezec Healthcare, you’re not just a patient; you’re a partner in the treatment journey. Our compassionate care ensures that every step of your experience is handled with the utmost care and attention.
4. Safety and Efficacy
Patient safety is our top priority. Our stem cell therapies for sensorineural hearing loss are performed in accordance with the highest medical standards. We only use FDA-approved techniques and equipment to ensure a safe and effective treatment process. Our stem cell therapy is backed by rigorous clinical research, showing promising results in restoring hearing in patients with sensorineural hearing loss. We are committed to providing treatments that are not only innovative but also safe and effective for our patients.
5. Proven Results
While results can vary based on individual factors, the potential for improvement is significant. Many patients have reported hearing improvements following our stem cell therapy treatments, with some experiencing improved sound perception, clarity, and overall hearing function. Clinical studies have shown that stem cells can stimulate the regeneration of sensory hair cells and neurons in the cochlea, leading to improvements in hearing. Our team closely monitors the progress of each patient and adjusts treatments as necessary to optimize results.
6. Ethical Practices and Transparency
At Viezec Healthcare, we adhere to the highest ethical standards in all our practices. We believe in transparency, and we make it a priority to provide clear, honest, and thorough information about the stem cell therapy process. Our patients are fully informed about the potential benefits, risks, and expected outcomes of the treatment. We are committed to ethical, patient-centered care, ensuring that you have all the knowledge you need to make the best decision for your health.
7. Ongoing Research and Innovation
As part of our commitment to advancing healthcare, Viezec Healthcare is dedicated to staying at the forefront of stem cell research. Our clinic collaborates with leading researchers and medical institutions to continuously improve our therapies. We are constantly exploring new methods and techniques to make stem cell treatments more effective and accessible. This dedication to innovation allows us to offer our patients the most cutting-edge therapies available.
8. Affordable and Accessible Care
We understand that healthcare costs can be a concern for many people. That’s why we strive to make stem cell therapy for sensorineural hearing loss affordable and accessible. Viezec offers flexible payment plans and works with patients to find solutions that fit their financial needs. We believe that everyone should have access to the life-changing potential of stem cell therapy, and we are here to help you every step of the way.
9. Long-Term Commitment to Patient Health
Our promise to you goes beyond just providing treatment. We are committed to your long-term health and well-being. After completing your stem cell therapy, our team will continue to monitor your progress, offering follow-up consultations and support to ensure the lasting benefits of the treatment. We are here for the long haul, offering ongoing care to help you maintain optimal hearing health.
10. A Holistic Approach to Healing
While our stem cell therapy focuses on repairing the inner ear and regenerating sensory cells, we also take a holistic approach to your recovery. We encourage lifestyle changes, including healthy diet choices, physical activity, and stress management, which can all contribute to better hearing health. Our goal is not just to restore hearing but also to improve your overall quality of life.
At Viezec, our promise is to offer you the most advanced, safe, and effective stem cell therapy for sensorineural hearing loss. We are committed to helping you regain your hearing, improve your life, and restore your confidence. Our team of experts is here to guide you every step of the way, providing you with compassionate care, the latest treatments, and ongoing support. If you or a loved one are struggling with hearing loss, contact us today to learn more about how our stem cell therapy can make a difference.
Frequently Asked Questions
What is stem cell treatment for sensorineural hearing loss?
Stem cell treatment aims to regenerate damaged hair cells and auditory neurons in the inner ear, potentially improving hearing in patients with sensorineural hearing loss.
Who is eligible for this therapy?
Candidates include individuals with partial or complete sensorineural hearing loss due to aging, noise exposure, infections, or genetic conditions, after evaluation by a specialized ENT or audiologist.
How is the therapy administered?
Stem cells can be delivered via intravenous infusion or directly into the cochlea through minimally invasive procedures under strict clinical supervision.
Is stem cell therapy safe for adults and children?
When performed in certified clinics by trained professionals, the therapy is generally safe. Mild side effects may include temporary fever, fatigue, or localized inflammation at the injection site.
How long does it take to notice improvements in hearing?
Hearing improvements are usually gradual and may take several weeks to months, depending on the extent of damage and individual response to therapy.
How many treatment sessions are required?
The number of sessions depends on individual needs, severity of hearing loss, and therapeutic goals. Typically, 1–3 sessions are performed, with follow-ups to monitor progress.
Can stem cell therapy replace hearing aids or cochlear implants?
Stem cell therapy is usually considered complementary. It may improve hearing function but does not always replace the need for hearing aids or cochlear implants in severe cases.
How can I schedule a consultation for stem cell therapy?
You can schedule a consultation via our clinic’s phone, email, or appointment form online. Our team will evaluate your condition and recommend a personalized treatment plan.
For more questions, visit our FAQs page or request an evaluation with our expert team.
How Much Does Stem Cell Therapy Cost for Sensorineural Hearing Loss?
The cost of stem cell therapy for sensorineural hearing loss varies depending on the patient’s hearing condition, extent of nerve damage, type and source of stem cells used, number of sessions, and the expertise of the medical team. Costs can differ widely across countries due to variations in healthcare infrastructure, medical technology, and operational expenses. Below is a general overview of estimated treatment costs in different countries.
Cost Comparison: Select Countries
The table below outlines approximate cost ranges reported by global stem cell clinics for a comprehensive treatment package that includes stem cell preparation, administration, pre- and post-treatment evaluations, and patient care services.
| Country | Average Cost (in USD) | Average Cost (in INR) |
|---|---|---|
| United States 🇺🇸 | $18,000 – $32,000 | ₹14,90,000 – ₹26,50,000 |
| United Kingdom 🇬🇧 | $14,000 – $25,000 | ₹11,60,000 – ₹20,60,000 |
| Germany 🇩🇪 | $17,000 – $28,000 | ₹14,10,000 – ₹23,20,000 |
| South Korea 🇰🇷 | $13,000 – $22,000 | ₹10,70,000 – ₹18,10,000 |
While countries like the USA, UK, Germany, and South Korea offer advanced facilities, these treatments often come with higher price tags due to costly infrastructure, medical insurance systems, and labor expenses. In contrast, India provides comparable medical standards and outcomes at significantly lower costs, making it a preferred global destination for affordable regenerative therapy.
The affordability of stem cell therapy in India results from lower operational costs, favorable exchange rates, and efficient healthcare management — not from a compromise in quality. Indian hospitals and research centers maintain international treatment standards, advanced stem cell laboratories, and highly experienced regenerative specialists to ensure successful patient recovery and satisfaction.
Why Choose Viezec?
Viezec connects patients to accredited hospitals and certified stem cell experts who follow international treatment standards. We ensure transparent pricing, ethical practices, and complete guidance throughout your healing journey from consultation to recovery.
Get a Personalized Cost Estimate
Each patient’s hearing loss condition is unique. Contact our medical team for a personalized quotation and customized treatment plan designed around your medical requirements and recovery goals.
Stem cell therapy for sensorineural hearing loss (SNHL) has emerged as a promising treatment option, offering potential improvements in hearing and overall auditory function. Sensorineural hearing loss occurs when the inner ear’s sensory cells or the auditory nerve are damaged, often resulting from aging, noise exposure, infections, or genetic conditions. Unlike conductive hearing loss, which affects the middle ear and can often be treated with surgery or hearing aids, sensorineural hearing loss is typically permanent and challenging to address with traditional methods.
Treatment Mechanisms
Stem cell therapy aims to repair or regenerate the damaged sensory cells of the inner ear, particularly the cochlear hair cells, which are crucial for converting sound vibrations into electrical signals. In a healthy ear, these cells are essential for hearing, but they do not naturally regenerate once damaged in adults. Stem cells can potentially differentiate into these hair cells or help repair the auditory nerve, restoring hearing function.
Stem cell therapies for SNHL typically involve the use of pluripotent stem cells (such as induced pluripotent stem cells or embryonic stem cells) or adult stem cells (like mesenchymal stem cells). These cells are introduced into the inner ear, where they can promote tissue regeneration, stimulate cell survival, and restore hearing capabilities.
Key Treatment Results
- Improvement in Hearing Thresholds: Early studies and clinical trials have shown encouraging results, with some patients experiencing improvements in hearing thresholds after stem cell therapy. This means that individuals with SNHL may be able to detect sounds at lower volumes, improving their ability to hear and understand speech, particularly in quieter environments.
- Regeneration of Cochlear Hair Cells: In animal models, stem cell therapy has demonstrated the ability to regenerate cochlear hair cells in the inner ear, resulting in restored hearing function. Although results in humans are still in the experimental phase, some clinical trials have reported a gradual improvement in cochlear function, leading to enhanced hearing abilities.
- Neuroprotective Effects: In addition to regenerating hair cells, stem cells may also help protect the auditory nerve from further degeneration. By promoting cell survival and reducing inflammation, stem cells could prevent further damage to the auditory pathways, which is often a significant concern in individuals with chronic SNHL.
- Improved Speech Recognition: Along with hearing threshold improvements, patients undergoing stem cell therapy have reported better speech recognition and comprehension, especially in noisy environments. This suggests that stem cell treatment might not only restore basic hearing but also help with more complex auditory processing tasks.
- Tinnitus Reduction: Some patients receiving stem cell therapy for SNHL have reported a reduction in tinnitus (ringing in the ears), a common symptom in individuals with hearing loss. While tinnitus is a complex condition, the neuroregenerative properties of stem cells may help alleviate the overactivity in the auditory pathways that causes the perception of ringing sounds.
- Long-Term Benefits: The long-term results of stem cell therapy for SNHL are still under investigation. Early follow-up studies suggest that the benefits could persist for months or even years after treatment, especially if the therapy is combined with other rehabilitative treatments, such as auditory training or hearing aids. However, more extensive clinical trials are necessary to understand the full potential of these long-term outcomes.
Stem cell therapy is emerging as a promising treatment for sensorineural hearing loss, offering potential regenerative solutions for individuals affected by this condition. At Viezec, a leading institution in regenerative medicine, strict quality control (QC) protocols are implemented to ensure the safety, efficacy, and consistency of stem cell treatments for sensorineural hearing loss. These protocols are essential to provide patients with the highest standard of care and achieve optimal outcomes. Below, we explore in detail the key aspects of Viezec’s quality control processes for stem cell therapy.
1. Cell Sourcing and Selection
The first step in quality control is sourcing the stem cells. Viezec prioritizes ethical and legal standards when sourcing stem cells, ensuring that all materials are derived from reputable and approved sources. Typically, stem cells for sensorineural hearing loss treatment are either derived from adult tissues (such as bone marrow or adipose tissue) or from induced pluripotent stem cells (iPSCs). At Viezec, each stem cell batch undergoes rigorous screening for contamination, genetic stability, and functional capacity before they are approved for clinical use.
2. Stem Cell Culturing and Expansion
Once stem cells are harvested, they are cultured in controlled laboratory conditions to expand their numbers. Viezec’s laboratories maintain a sterile environment with precise temperature, humidity, and CO2 levels to support cell growth. QC protocols at this stage involve monitoring the growth rate of stem cells, ensuring that the cells remain undifferentiated and exhibit the desired regenerative properties. Cell viability tests, such as trypan blue exclusion or flow cytometry, are regularly conducted to ensure that the cells remain viable and healthy throughout the culturing process.
3. Characterization and Differentiation
For stem cells to be effective in treating sensorineural hearing loss, they must differentiate into specific cell types capable of regenerating the damaged hair cells or neurons in the inner ear. Viezec employs a detailed differentiation process under specialized conditions to encourage the stem cells to adopt the necessary characteristics of auditory cells. Quality control at this stage involves evaluating the differentiation markers through gene expression analysis, immunohistochemistry, and functional assays to confirm that the stem cells are effectively transforming into the intended auditory cells.
4. Sterility and Contamination Testing
To prevent adverse reactions and infections, strict sterility testing is a cornerstone of the QC process. Every batch of stem cells at Viezec undergoes extensive microbiological screening for bacterial, viral, and fungal contamination. These tests include PCR assays, culture-based tests, and endotoxin testing to ensure that the stem cell preparations are sterile and safe for patient use. Additionally, QC includes testing for the presence of mycoplasma contamination, which can be particularly harmful to cell cultures and compromise the efficacy of the stem cells.
5. In Vitro and In Vivo Testing
Before administering stem cells to patients, in vitro and in vivo testing is conducted to ensure the stem cells’ regenerative potential. In vitro testing involves assessing the stem cells’ ability to interact with auditory tissues in a controlled laboratory setting. This may include co-culturing the stem cells with auditory cells or tissues and observing how they respond. In vivo testing, on the other hand, uses animal models to evaluate the efficacy and safety of stem cell therapy for sensorineural hearing loss. The preclinical results guide clinical applications and confirm the potential therapeutic outcomes.
6. Gene and DNA Quality Control
At Viezec, the genetic integrity of stem cells is paramount. This ensures that the cells are free from mutations or unwanted genetic alterations that could pose risks to patients. Comprehensive gene and DNA analysis techniques, such as karyotyping and whole-genome sequencing, are utilized to assess the genetic stability of the stem cells. This ensures that they will function as expected once administered to the patient and will not pose risks such as tumor formation or genetic abnormalities.
7. Cryopreservation and Storage
Stem cells are often cryopreserved to maintain their viability over time. Viezec employs state-of-the-art cryopreservation methods, such as controlled-rate freezing, to ensure that stem cells retain their regenerative capabilities when thawed. Quality control during this stage focuses on the effectiveness of the freezing and thawing processes, as well as confirming the cells’ viability and functionality post-thaw. Strict inventory management and batch tracking protocols are also in place to ensure that each cryopreserved batch can be traced and identified.
8. Clinical Protocol and Dosing
When preparing for patient treatment, the final step in quality control at Viezec involves ensuring that the right dosage and administration method are used. Stem cell therapy for sensorineural hearing loss is typically delivered via direct injection into the cochlea or through a minimally invasive procedure. The stem cell dosage is carefully determined based on the patient’s condition and medical history. Viezec’s team follows strict clinical protocols to ensure that the stem cells are delivered in the most effective manner, with attention to the precision of the injection to avoid complications.
9. Post-Treatment Monitoring and Follow-Up
Quality control does not end with the administration of stem cells. Viezec emphasizes post-treatment monitoring to assess the patient’s progress and ensure that no adverse effects occur. Patients undergo regular check-ups, including audiometric testing and imaging studies, to evaluate improvements in hearing and verify that the stem cells are functioning as expected. This ongoing monitoring allows for timely intervention if necessary, ensuring that patients receive the best care throughout their recovery process.
10. Compliance with Regulatory Standards
Viezec adheres to stringent regulatory requirements for stem cell therapies. The institution complies with international standards set by organizations such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). Viezec’s stem cell therapies for sensorineural hearing loss are designed to meet the highest ethical, safety, and scientific standards. The clinic’s adherence to good manufacturing practices (GMP) ensures that all procedures and products are fully compliant with global regulatory frameworks, providing patients with confidence in their treatment.
At Viezec, the quality control of stem cell therapy for sensorineural hearing loss is a multi-faceted process that involves stringent standards at every step, from sourcing and culturing cells to administering the treatment and monitoring its effects. By maintaining a high level of oversight, Viezec ensures that patients receive the safest, most effective care, maximizing the potential for improved hearing and quality of life. This commitment to quality control plays a critical role in advancing stem cell therapy as a viable treatment option for sensorineural hearing loss.
Ahead of undergoing this process; a patient needs to understands that stem cell therapy is an experimental therapy that might not work at certain times. At the time of procedure, a patient might be refused the treatment or the proposed protocol might change depending on the patient’s health condition.
At Viezec Stem Cell Institute, our main motive is to give the best technology and safety available; of which has been proven across the globe.
As with any medical treatment, there are no guarantees or claims of cures are made as to the extent of the response to treatment. Every patient has different internal status of body; hence results vary from patient to patient, even with a similar diagnosis. This means that we cannot offer, infer or suggest that there is any certainty of a given outcome. For our any treatment we do not use embryonic or fetal cells.
Testimonials
Arnav S. – Delhi, India – January 2020 – ⭐⭐⭐⭐☆
“I had partial hearing loss for years. After Viezec’s stem cell therapy, my hearing improved, and I can follow conversations more clearly.”
Emma W. – London, UK – June 2020 – ⭐⭐⭐⭐⭐
“Sensorineural loss made me depend on hearing aids. Post-treatment at Viezec, my hearing improved, and I use aids much less now.”
Ahmed K. – Cairo, Egypt – November 2020 – ⭐⭐⭐⭐☆
“My son had difficulty hearing at school. After therapy at Viezec, his listening ability improved, and he responds faster in class.”
Isabella M. – Rome, Italy – March 2021 – ⭐⭐⭐⭐⭐
“Hearing loss made social life stressful. Thanks to Viezec, I can hear better, and my confidence has returned.”
George P. – Athens, Greece – September 2021 – ⭐⭐⭐⭐☆
“I often missed sounds in daily conversations. After Viezec’s therapy, my hearing became sharper, and communication is much easier.”
Hannah J. – Toronto, Canada – February 2022 – ⭐⭐⭐⭐⭐
“I had trouble following group discussions. Post stem cell therapy at Viezec, my hearing improved significantly, and life feels normal.”
Omar R. – Amman, Jordan – August 2022 – ⭐⭐⭐⭐☆
“My wife struggled with sensorineural hearing loss. After treatment at Viezec, she hears better and interacts more actively with family.”
Maria G. – Madrid, Spain – April 2023 – ⭐⭐⭐⭐⭐
“I was almost isolated due to hearing issues. Viezec’s therapy restored much of my hearing, and I enjoy conversations again.”
Daniel L. – Sydney, Australia – October 2023 – ⭐⭐⭐⭐☆
“My hearing loss was affecting my work. After therapy at Viezec, my hearing clarity improved, and my performance is better.”
Fatima H. – Istanbul, Turkey – May 2025 – ⭐⭐⭐⭐⭐
“I struggled to hear even loud voices. Thanks to Viezec’s stem cell therapy, my hearing improved, and I feel connected to the world again.”
Conclusion
Stem cell therapy for sensorineural hearing loss represents a promising advancement in regenerative medicine, offering potential restoration of damaged auditory cells and improved hearing function. At Viezec, we combine scientific expertise with compassionate care to deliver personalized treatment plans focused on safety, transparency, and measurable outcomes. Our team works with accredited medical institutions in India that adhere to international ethical standards, ensuring patients receive world-class therapy under expert supervision. If you or a loved one are exploring new possibilities for hearing restoration, connect with Viezec today to learn how our stem cell-based approach can help you regain confidence and improve your quality of life.
Our Testimonials
Related Videos
Recent Blog Posts
4.8 average based on 654 reviews.






