Eye diseases represent a significant health concern globally, affecting millions of individuals and often leading to visual impairment or blindness. These conditions can vary from common refractive errors to more severe diseases like glaucoma, diabetic retinopathy, and age-related macular degeneration (AMD). The impact of these diseases extends beyond the individual, affecting their quality of life, ability to work, and overall well-being. Understanding the scope and nature of these diseases is crucial in devising effective treatments. For instance, age-related macular degeneration is a leading cause of vision loss in older adults, while diabetic retinopathy is a common complication of diabetes, potentially leading to blindness if not managed properly. Retinitis pigmentosa, on the other hand, is a group of rare, genetic disorders that involve a breakdown and loss of cells in the retina.
Importance of Innovative Treatments
The advent of innovative treatments for eye diseases is of paramount importance given the limitations of current therapeutic approaches. Traditional methods often focus on managing symptoms rather than addressing the root causes of the diseases. For example, while anti-VEGF injections are commonly used to treat AMD, they primarily serve to slow the progression of the disease rather than reverse it. Similarly, laser surgeries and medications for glaucoma aim to reduce intraocular pressure but do not restore lost vision. Hence, there is a critical need for treatments that can offer more definitive and curative outcomes. Innovations in medical research and technology are paving the way for such breakthroughs, with stem cell therapy emerging as a promising frontier. Stem cell therapy holds the potential to regenerate damaged tissues, offering hope for more effective and long-lasting treatments.
Introduction to Stem Cell Therapy
Stem cell therapy involves the use of stem cells to repair or replace damaged cells and tissues in the body. Stem cells are unique because of their ability to differentiate into various cell types and their potential to self-renew. This makes them particularly valuable in regenerative medicine. In the context of eye diseases, stem cell therapy aims to restore vision by repairing the damaged retinal cells, regenerating optic nerve cells, or replacing corneal cells. The different types of stem cells used include embryonic stem cells, adult stem cells, and induced pluripotent stem cells (iPSCs), each with its own set of advantages and challenges. Research in this field has shown promising results, with clinical trials demonstrating the potential of stem cell therapy to improve vision and even restore it in some cases. This innovative approach is gradually transforming the landscape of treatment options for various eye diseases.
Types of Eye Diseases Treatable with Stem Cell Therapy
Age-related Macular Degeneration (AMD)
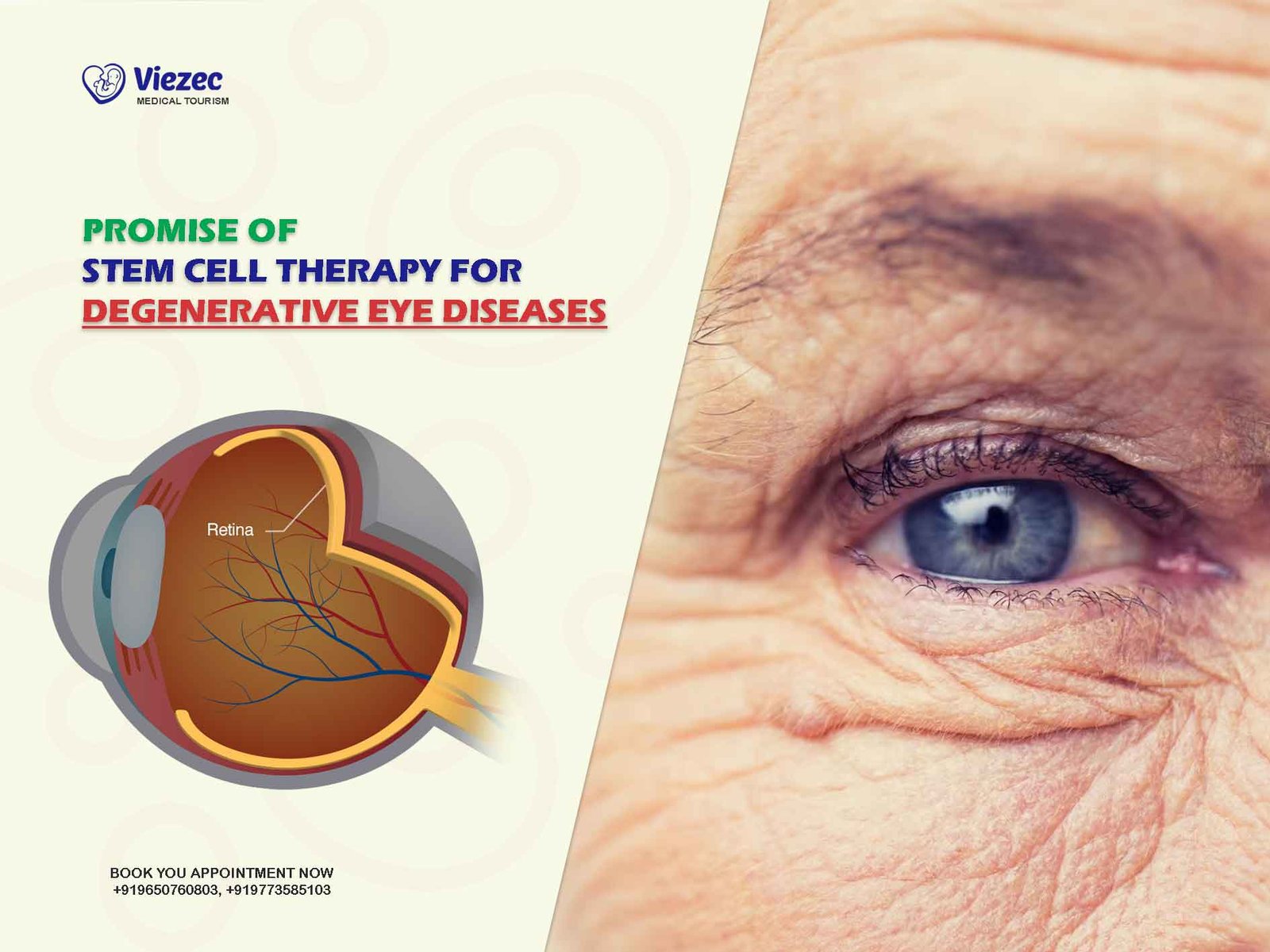
Age-related macular degeneration (AMD) is a degenerative condition that affects the macula, the central part of the retina responsible for sharp, central vision. AMD is a leading cause of vision loss among people aged 50 and older. The disease is categorized into two types: dry AMD and wet AMD. Dry AMD is more common and progresses slowly, causing gradual vision loss, while wet AMD is characterized by the growth of abnormal blood vessels under the retina, leading to rapid and severe vision loss. Current treatments for AMD, such as anti-VEGF injections and laser therapy, primarily focus on managing the symptoms and slowing the progression of the disease. However, these treatments do not restore lost vision, highlighting the need for more effective therapies.
Retinitis Pigmentosa (RP)
Retinitis pigmentosa (RP) is a group of genetic disorders that lead to progressive retinal degeneration and vision loss. The disease typically manifests in childhood or adolescence, initially affecting peripheral vision and night vision before progressing to central vision loss. RP is caused by mutations in various genes responsible for the function and survival of photoreceptor cells in the retina. As the disease progresses, these photoreceptor cells degenerate, leading to vision impairment and eventually blindness. There is currently no cure for RP, and treatment options are limited to supportive measures such as visual aids and mobility training. However, stem cell therapy offers a potential avenue for restoring vision by replacing the damaged photoreceptor cells and supporting retinal function.
Glaucoma
Glaucoma is a group of eye diseases characterized by damage to the optic nerve, often associated with increased intraocular pressure. It is one of the leading causes of irreversible blindness worldwide. Glaucoma can be classified into different types, including primary open-angle glaucoma, angle-closure glaucoma, and secondary glaucoma. The disease progresses slowly and often goes unnoticed until significant vision loss has occurred. Traditional treatments for glaucoma, such as medications, laser therapy, and surgery, aim to lower intraocular pressure and prevent further damage to the optic nerve. However, these treatments do not restore lost vision, underscoring the need for novel therapeutic approaches. Stem cell therapy holds promise for regenerating damaged optic nerve cells and preserving vision.
Diabetic Retinopathy
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina. It is a leading cause of blindness in adults of working age. The disease progresses through different stages, starting with mild non-proliferative diabetic retinopathy and advancing to severe non-proliferative and proliferative diabetic retinopathy. In the advanced stages, abnormal blood vessels grow on the surface of the retina, leading to bleeding, scarring, and vision loss. Current treatments for diabetic retinopathy, such as laser therapy, anti-VEGF injections, and vitrectomy, aim to manage the symptoms and prevent further vision loss. However, these treatments do not reverse the damage, highlighting the potential of stem cell therapy to repair and regenerate the damaged retinal tissues.
Corneal Diseases
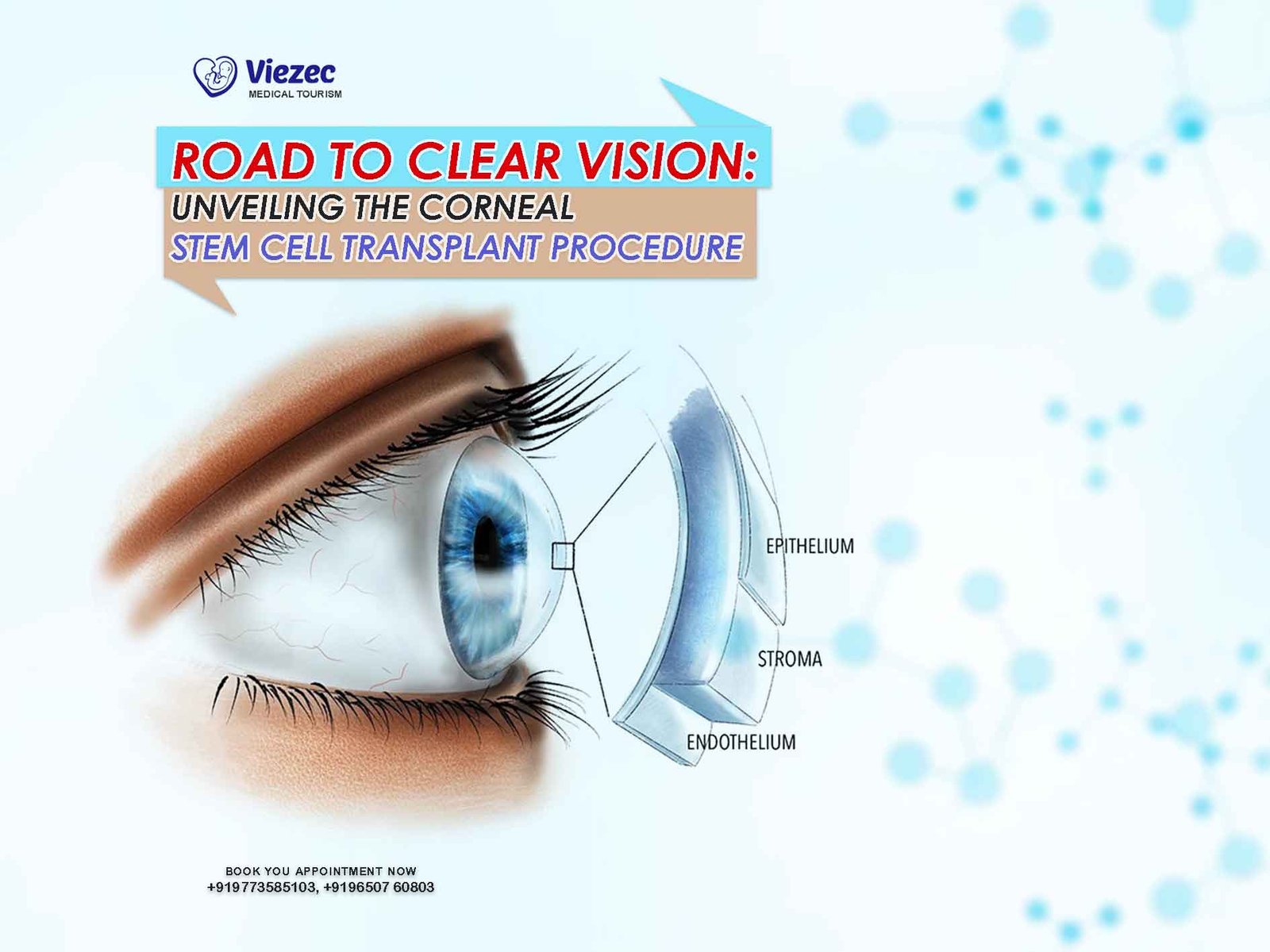
Corneal diseases encompass a wide range of conditions that affect the cornea, the clear, outer layer of the eye. These conditions can result from infections, injuries, genetic disorders, and degenerative diseases. Common corneal diseases include keratoconus, Fuchs’ endothelial dystrophy, and corneal ulcers. These diseases can lead to corneal scarring, thinning, and loss of transparency, ultimately affecting vision. Traditional treatments for corneal diseases include medications, corneal transplantation, and laser surgery. However, these treatments have limitations, such as the risk of graft rejection and limited availability of donor corneas. Stem cell therapy offers a potential solution by promoting the regeneration of corneal cells and restoring the integrity and function of the cornea.
Understanding Stem Cells
Types of Stem Cells
Embryonic Stem Cells
Embryonic stem cells (ESCs) are derived from the inner cell mass of the blastocyst, an early-stage embryo. These cells are pluripotent, meaning they have the ability to differentiate into any cell type in the body. This characteristic makes ESCs highly valuable for regenerative medicine, including the treatment of eye diseases. However, the use of ESCs raises ethical concerns because their derivation involves the destruction of the embryo. Despite these concerns, ESCs have been used in various research studies and clinical trials to explore their potential in treating retinal diseases, corneal disorders, and other eye conditions. The ability of ESCs to generate different types of retinal cells and support retinal function has shown promising results in preclinical studies.
Adult Stem Cells
Adult stem cells, also known as somatic stem cells, are found in various tissues throughout the body. These cells are multipotent, meaning they can differentiate into a limited range of cell types related to their tissue of origin. In the context of eye diseases, adult stem cells such as mesenchymal stem cells (MSCs) and limbal stem cells have been studied for their regenerative potential. MSCs can be isolated from bone marrow, adipose tissue, and other sources, and they have shown promise in promoting retinal repair and reducing inflammation. Limbal stem cells, located at the border of the cornea and the sclera, are essential for maintaining corneal transparency and integrity. Transplantation of limbal stem cells has been successfully used to treat limbal stem cell deficiency and restore corneal function.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are generated by reprogramming adult cells, such as skin or blood cells, to a pluripotent state. This process involves introducing specific genes that reset the cells to an embryonic-like state. iPSCs have the same differentiation potential as ESCs, but they circumvent the ethical issues associated with embryo destruction. iPSCs can be derived from the patient’s own cells, reducing the risk of immune rejection. In eye research, iPSCs have been used to generate retinal cells, corneal cells, and other ocular cell types for disease modeling, drug testing, and potential therapeutic applications. The use of iPSCs in clinical trials for retinal diseases has shown encouraging results, demonstrating their potential to restore vision.
Mechanisms of Action in Eye Therapy
The mechanisms by which stem cells exert their therapeutic effects in eye diseases are multifaceted. Stem cells can differentiate into specific retinal or corneal cells, replacing damaged or lost cells and restoring tissue function. They also secrete various growth factors, cytokines, and extracellular vesicles that promote tissue repair, reduce inflammation, and enhance cell survival. For example, in AMD and RP, stem cells can replace degenerated photoreceptor cells and support retinal pigment epithelium (RPE) cells, improving retinal function and preserving vision. In glaucoma, stem cells can potentially regenerate damaged optic nerve cells and protect against further degeneration. In diabetic retinopathy, stem cells can repair damaged blood vessels and reduce retinal inflammation. The ability of stem cells to modulate the immune response and promote a regenerative microenvironment further enhances their therapeutic potential.
Evidence-Based Approach in Stem Cell Therapy
Importance of Clinical Trials
Clinical trials are essential for evaluating the safety, efficacy, and long-term outcomes of stem cell therapies for eye diseases. These trials follow rigorous protocols to ensure that the treatments are tested in a controlled and systematic manner. By enrolling patients in clinical trials, researchers can gather valuable data on the therapeutic effects, potential side effects, and overall impact of stem cell treatments. The importance of clinical trials lies in their ability to provide evidence-based information that guides clinical practice and informs regulatory decisions. For instance, phase I clinical trials focus on assessing the safety and feasibility of the treatment, while phase II and III trials evaluate its efficacy and optimal dosage. Successful clinical trials can lead to the approval and widespread adoption of stem cell therapies for eye diseases.
Current Research and Findings
Current research in stem cell therapy for eye diseases is rapidly advancing, with numerous studies and trials underway. For example, research on stem cell transplantation for AMD has shown promising results in animal models and early-phase clinical trials. Studies have demonstrated the potential of stem cells to regenerate RPE cells and photoreceptor cells, improving retinal function and preserving vision. Similarly, research on stem cell therapy for RP has explored the use of iPSCs and MSCs to replace degenerated photoreceptor cells and support retinal health. In glaucoma, stem cell-based approaches aim to regenerate damaged optic nerve cells and protect against further degeneration. The findings from these studies provide a strong foundation for further research and development of stem cell therapies for various eye diseases.
Case Studies and Success Stories
Case studies and success stories highlight the potential of stem cell therapy to transform the treatment of eye diseases. For instance, a landmark case involved the use of iPSC-derived RPE cells to treat a patient with advanced AMD. The patient experienced significant improvements in vision, demonstrating the therapeutic potential of stem cell transplantation. Another notable case involved the use of limbal stem cell transplantation to restore vision in a patient with limbal stem cell deficiency. The patient achieved long-term corneal clarity and improved visual acuity, showcasing the effectiveness of stem cell therapy in corneal diseases. These success stories provide hope and inspiration for patients and researchers, underscoring the transformative potential of stem cell therapy in restoring vision and improving quality of life.
Stem Cell Therapy for Age-related Macular Degeneration (AMD)
Pathophysiology of AMD
Age-related macular degeneration (AMD) is a complex disease characterized by the progressive degeneration of the macula, the central part of the retina responsible for sharp, central vision. The pathophysiology of AMD involves multiple factors, including genetic predisposition, oxidative stress, and inflammation. In dry AMD, the accumulation of drusen, yellow deposits under the retina, leads to retinal atrophy and loss of photoreceptor cells. In wet AMD, the growth of abnormal blood vessels under the retina causes leakage and bleeding, leading to rapid and severe vision loss. Understanding the underlying mechanisms of AMD is crucial for developing effective treatments. Research has shown that oxidative damage to RPE cells and the subsequent degeneration of photoreceptors play a central role in the progression of AMD.
Treatment Protocols
Stem cell therapy for AMD involves the transplantation of stem cells to replace damaged RPE cells and support retinal function. Different types of stem cells, including ESCs, iPSCs, and MSCs, have been investigated for their potential in treating AMD. The treatment protocol typically involves the isolation and expansion of stem cells, followed by their differentiation into RPE cells. These RPE cells are then transplanted into the subretinal space, where they integrate with the host tissue and restore retinal function. Preclinical studies and early-phase clinical trials have demonstrated the safety and feasibility of this approach. The use of stem cells to regenerate RPE cells and photoreceptor cells holds promise for improving vision and halting the progression of AMD.
Clinical Outcomes and Evidence
Clinical outcomes of stem cell therapy for AMD have shown encouraging results, with patients experiencing improvements in vision and retinal function. In a notable clinical trial, patients with advanced dry AMD received subretinal transplantation of iPSC-derived RPE cells. The treatment was well-tolerated, and some patients showed significant improvements in visual acuity and retinal sensitivity. Another study involving ESC-derived RPE cells demonstrated similar outcomes, with patients experiencing stabilization or improvement in vision. These findings provide strong evidence for the potential of stem cell therapy to treat AMD. However, long-term follow-up and larger clinical trials are needed to confirm the efficacy and safety of this approach. The promising results from these studies highlight the potential of stem cell therapy to transform the treatment landscape for AMD.
Stem Cell Therapy for Retinitis Pigmentosa (RP)
Pathophysiology of RP
Retinitis pigmentosa (RP) is a group of genetic disorders characterized by the progressive degeneration of photoreceptor cells in the retina. The disease is caused by mutations in various genes that are essential for the function and survival of photoreceptors. RP typically manifests in childhood or adolescence, initially affecting peripheral vision and night vision. As the disease progresses, patients experience a gradual loss of central vision, leading to blindness. The pathophysiology of RP involves the degeneration of rod photoreceptors, followed by the secondary loss of cone photoreceptors. This progressive cell death leads to retinal thinning and functional impairment. Understanding the genetic and molecular mechanisms underlying RP is crucial for developing targeted treatments.
Treatment Protocols
Stem cell therapy for RP aims to replace the degenerated photoreceptor cells and support retinal health. Different types of stem cells, including ESCs, iPSCs, and MSCs, have been investigated for their potential in treating RP. The treatment protocol typically involves the isolation and expansion of stem cells, followed by their differentiation into photoreceptor cells or retinal progenitor cells. These cells are then transplanted into the subretinal space, where they integrate with the host tissue and restore retinal function. Preclinical studies and early-phase clinical trials have demonstrated the feasibility of this approach. The use of stem cells to regenerate photoreceptor cells and support retinal health holds promise for improving vision and halting the progression of RP.
Clinical Outcomes and Evidence
Clinical outcomes of stem cell therapy for RP have shown promising results, with patients experiencing improvements in vision and retinal function. In a notable clinical trial, patients with advanced RP received subretinal transplantation of iPSC-derived retinal progenitor cells. The treatment was well-tolerated, and some patients showed significant improvements in visual acuity and retinal sensitivity. Another study involving MSC-derived photoreceptor cells demonstrated similar outcomes, with patients experiencing stabilization or improvement in vision. These findings provide strong evidence for the potential of stem cell therapy to treat RP. However, long-term follow-up and larger clinical trials are needed to confirm the efficacy and safety of this approach. The promising results from these studies highlight the potential of stem cell therapy to transform the treatment landscape for RP.
Stem Cell Therapy for Glaucoma
Pathophysiology of Glaucoma
Glaucoma is a group of eye diseases characterized by damage to the optic nerve, often associated with increased intraocular pressure. The disease progresses slowly and often goes unnoticed until significant vision loss has occurred. The pathophysiology of glaucoma involves the degeneration of retinal ganglion cells (RGCs) and the optic nerve, leading to vision impairment and blindness. Increased intraocular pressure is a major risk factor for glaucoma, but other factors such as impaired blood flow to the optic nerve and neuroinflammation also play a role. Understanding the underlying mechanisms of glaucoma is crucial for developing effective treatments. Research has shown that oxidative stress, mitochondrial dysfunction, and neuroinflammation contribute to the degeneration of RGCs and the progression of glaucoma.
Treatment Protocols
Stem cell therapy for glaucoma aims to regenerate damaged RGCs and protect against further degeneration. Different types of stem cells, including ESCs, iPSCs, and MSCs, have been investigated for their potential in treating glaucoma. The treatment protocol typically involves the isolation and expansion of stem cells, followed by their differentiation into RGCs or neuroprotective cells. These cells are then transplanted into the optic nerve or the vitreous cavity, where they integrate with the host tissue and support retinal function. Preclinical studies and early-phase clinical trials have demonstrated the feasibility of this approach. The use of stem cells to regenerate RGCs and protect against neurodegeneration holds promise for preserving vision and slowing the progression of glaucoma.
Clinical Outcomes and Evidence
Clinical outcomes of stem cell therapy for glaucoma have shown promising results, with patients experiencing improvements in vision and retinal function. In a notable clinical trial, patients with advanced glaucoma received intravitreal injection of MSC-derived neuroprotective cells. The treatment was well-tolerated, and some patients showed significant improvements in visual acuity and retinal sensitivity. Another study involving iPSC-derived RGCs demonstrated similar outcomes, with patients experiencing stabilization or improvement in vision. These findings provide strong evidence for the potential of stem cell therapy to treat glaucoma. However, long-term follow-up and larger clinical trials are needed to confirm the efficacy and safety of this approach. The promising results from these studies highlight the potential of stem cell therapy to transform the treatment landscape for glaucoma.
Stem Cell Therapy for Diabetic Retinopathy
Pathophysiology of Diabetic Retinopathy
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina. The disease progresses through different stages, starting with mild non-proliferative diabetic retinopathy and advancing to severe non-proliferative and proliferative diabetic retinopathy. In the advanced stages, abnormal blood vessels grow on the surface of the retina, leading to bleeding, scarring, and vision loss. The pathophysiology of diabetic retinopathy involves multiple factors, including hyperglycemia, oxidative stress, inflammation, and vascular dysfunction. Chronic high blood sugar levels damage the retinal blood vessels, leading to leakage and ischemia. Understanding the underlying mechanisms of diabetic retinopathy is crucial for developing effective treatments.
Treatment Protocols
Stem cell therapy for diabetic retinopathy aims to repair damaged blood vessels and reduce retinal inflammation. Different types of stem cells, including ESCs, iPSCs, and MSCs, have been investigated for their potential in treating diabetic retinopathy. The treatment protocol typically involves the isolation and expansion of stem cells, followed by their differentiation into vascular endothelial cells or retinal progenitor cells. These cells are then transplanted into the retina or injected into the vitreous cavity, where they integrate with the host tissue and support retinal function. Preclinical studies and early-phase clinical trials have demonstrated the feasibility of this approach. The use of stem cells to repair damaged blood vessels and reduce retinal inflammation holds promise for improving vision and halting the progression of diabetic retinopathy.
Clinical Outcomes and Evidence
Clinical outcomes of stem cell therapy for diabetic retinopathy have shown promising results, with patients experiencing improvements in vision and retinal function. In a notable clinical trial, patients with advanced diabetic retinopathy received intravitreal injection of MSC-derived vascular endothelial cells. The treatment was well-tolerated, and some patients showed significant improvements in visual acuity and retinal sensitivity. Another study involving iPSC-derived retinal progenitor cells demonstrated similar outcomes, with patients experiencing stabilization or improvement in vision. These findings provide strong evidence for the potential of stem cell therapy to treat diabetic retinopathy. However, long-term follow-up and larger clinical trials are needed to confirm the efficacy and safety of this approach. The promising results from these studies highlight the potential of stem cell therapy to transform the treatment landscape for diabetic retinopathy.
Stem Cell Therapy for Corneal Diseases
Pathophysiology of Corneal Diseases
Corneal diseases encompass a wide range of conditions that affect the cornea, the clear, outer layer of the eye. These conditions can result from infections, injuries, genetic disorders, and degenerative diseases. Common corneal diseases include keratoconus, Fuchs’ endothelial dystrophy, and corneal ulcers. These diseases can lead to corneal scarring, thinning, and loss of transparency, ultimately affecting vision. The pathophysiology of corneal diseases involves multiple factors, including genetic predisposition, environmental factors, and immune-mediated damage. Understanding the underlying mechanisms of corneal diseases is crucial for developing effective treatments. Research has shown that inflammation, oxidative stress, and cell apoptosis contribute to corneal damage and disease progression.
Treatment Protocols
Stem cell therapy for corneal diseases aims to promote the regeneration of corneal cells and restore the integrity and function of the cornea. Different types of stem cells, including ESCs, iPSCs, and limbal stem cells, have been investigated for their potential in treating corneal diseases. The treatment protocol typically involves the isolation and expansion of stem cells, followed by their differentiation into corneal epithelial cells or endothelial cells. These cells are then transplanted onto the corneal surface or injected into the corneal stroma, where they integrate with the host tissue and support corneal regeneration. Preclinical studies and early-phase clinical trials have demonstrated the feasibility of this approach. The use of stem cells to regenerate corneal cells and restore corneal transparency holds promise for improving vision and halting the progression of corneal diseases.
Clinical Outcomes and Evidence
Clinical outcomes of stem cell therapy for corneal diseases have shown promising results, with patients experiencing improvements in vision and corneal function. In a notable clinical trial, patients with advanced corneal disease received transplantation of limbal stem cells. The treatment was well-tolerated, and some patients showed significant improvements in visual acuity and corneal clarity. Another study involving iPSC-derived corneal endothelial cells demonstrated similar outcomes, with patients experiencing stabilization or improvement in vision. These findings provide strong evidence for the potential of stem cell therapy to treat corneal diseases. However, long-term follow-up and larger clinical trials are needed to confirm the efficacy and safety of this approach. The promising results from these studies highlight the potential of stem cell therapy to transform the treatment landscape for corneal diseases.
Challenges and Ethical Considerations
Ethical Issues in Stem Cell Research
The use of stem cells, particularly ESCs, raises significant ethical concerns because their derivation involves the destruction of embryos. This ethical dilemma has sparked debates and regulatory challenges worldwide. Some argue that the potential benefits of stem cell therapy, such as curing debilitating diseases and restoring vision, justify the use of ESCs. Others contend that alternative sources of stem cells, such as iPSCs, should be prioritized to avoid ethical issues. The ethical considerations extend beyond the use of ESCs to include issues related to informed consent, patient safety, and the potential for exploitation. Ensuring ethical standards and transparency in stem cell research is crucial for maintaining public trust and advancing the field responsibly.
Regulatory and Approval Processes
The regulatory and approval processes for stem cell therapies involve rigorous evaluations to ensure their safety, efficacy, and quality. Regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require comprehensive preclinical and clinical data before approving stem cell-based treatments. The approval process includes multiple phases of clinical trials, starting with phase I trials to assess safety and feasibility, followed by phase II and III trials to evaluate efficacy and optimal dosage. Ensuring compliance with regulatory standards is essential for the successful translation of stem cell therapies from the laboratory to the clinic. The regulatory landscape is continuously evolving to keep pace with advancements in stem cell research and address emerging challenges.
Addressing Patient Concerns
Addressing patient concerns is crucial for the successful implementation of stem cell therapies. Patients may have questions about the safety, efficacy, and long-term outcomes of these treatments. Providing clear and accurate information, obtaining informed consent, and ensuring patient safety are essential components of ethical stem cell therapy. Additionally, addressing concerns related to the cost and accessibility of stem cell treatments is important for ensuring equitable access to these innovative therapies. Patient education and engagement play a vital role in building trust and fostering a positive outlook toward stem cell therapies. By addressing patient concerns and providing transparent information, healthcare providers can enhance patient confidence and facilitate the adoption of stem cell-based treatments.
FAQs
What is stem cell therapy?
A: Stem cell therapy involves the use of stem cells to repair or replace damaged cells and tissues in the body. In the context of eye diseases, stem cell therapy aims to restore vision by repairing damaged retinal cells, regenerating optic nerve cells, or replacing corneal cells.
Which eye diseases can be treated with stem cell therapy?
A: Stem cell therapy has shown potential in treating various eye diseases, including age-related macular degeneration (AMD), retinitis pigmentosa (RP), glaucoma, diabetic retinopathy, and corneal diseases.
What types of stem cells are used in eye disease treatment?
A: Different types of stem cells used in eye disease treatment include embryonic stem cells (ESCs), adult stem cells (such as mesenchymal stem cells and limbal stem cells), and induced pluripotent stem cells (iPSCs).
Are there any risks associated with stem cell therapy for eye diseases?
A: While stem cell therapy holds promise, it also carries potential risks, such as immune rejection, tumor formation, and ethical concerns. Clinical trials are essential to evaluate the safety and efficacy of these treatments.
How can I access stem cell therapy for eye diseases?
A: Access to stem cell therapy for eye diseases typically involves participation in clinical trials or seeking treatment at specialized medical centers. It is important to consult with a healthcare provider to explore available options and determine eligibility.