Bone marrow transplantation (BMT) has revolutionized the treatment of various hematological disorders, providing a potential cure for conditions like leukemia, lymphoma, and aplastic anemia. This medical procedure involves replacing damaged or diseased bone marrow with healthy stem cells, which can be harvested from the patient (autologous transplant) or a donor (allogeneic transplant). The success of BMT largely depends on the compatibility between the donor and recipient, which traditionally has relied on finding a perfect or near-perfect human leukocyte antigen (HLA) match. As a result, finding suitable donors has been one of the most significant challenges in expanding the availability and success rates of bone marrow transplants.
Definition and Importance of Haploidentical Transplants
Haploidentical bone marrow transplantation refers to the use of a donor who is a partial genetic match, sharing at least half of the HLA genes with the recipient. This type of transplant opens new avenues for patients who do not have a fully matched sibling or unrelated donor. Haploidentical transplants significantly broaden the donor pool, making potentially life-saving treatments available to a larger number of patients. The importance of haploidentical transplants lies in their ability to bridge the genetic gap that often leaves many patients without a viable donor option, thus offering hope and new treatment possibilities where none existed before.
Historical Context and Evolution of Transplant Techniques
The history of bone marrow transplantation dates back to the mid-20th century when the procedure was first attempted with limited success due to complications such as graft-versus-host disease (GVHD) and infections. Over the decades, advances in immunosuppressive therapies, donor selection, and supportive care have significantly improved outcomes. The concept of haploidentical transplantation emerged as a response to the critical need for more donor options. Initially met with skepticism due to high risks of complications, the technique has evolved with innovative approaches to immunosuppression and better understanding of HLA mismatches, leading to its current status as a viable and increasingly common treatment option.
Genetic Compatibility and Challenges
Understanding Genetic Matching in Transplantation
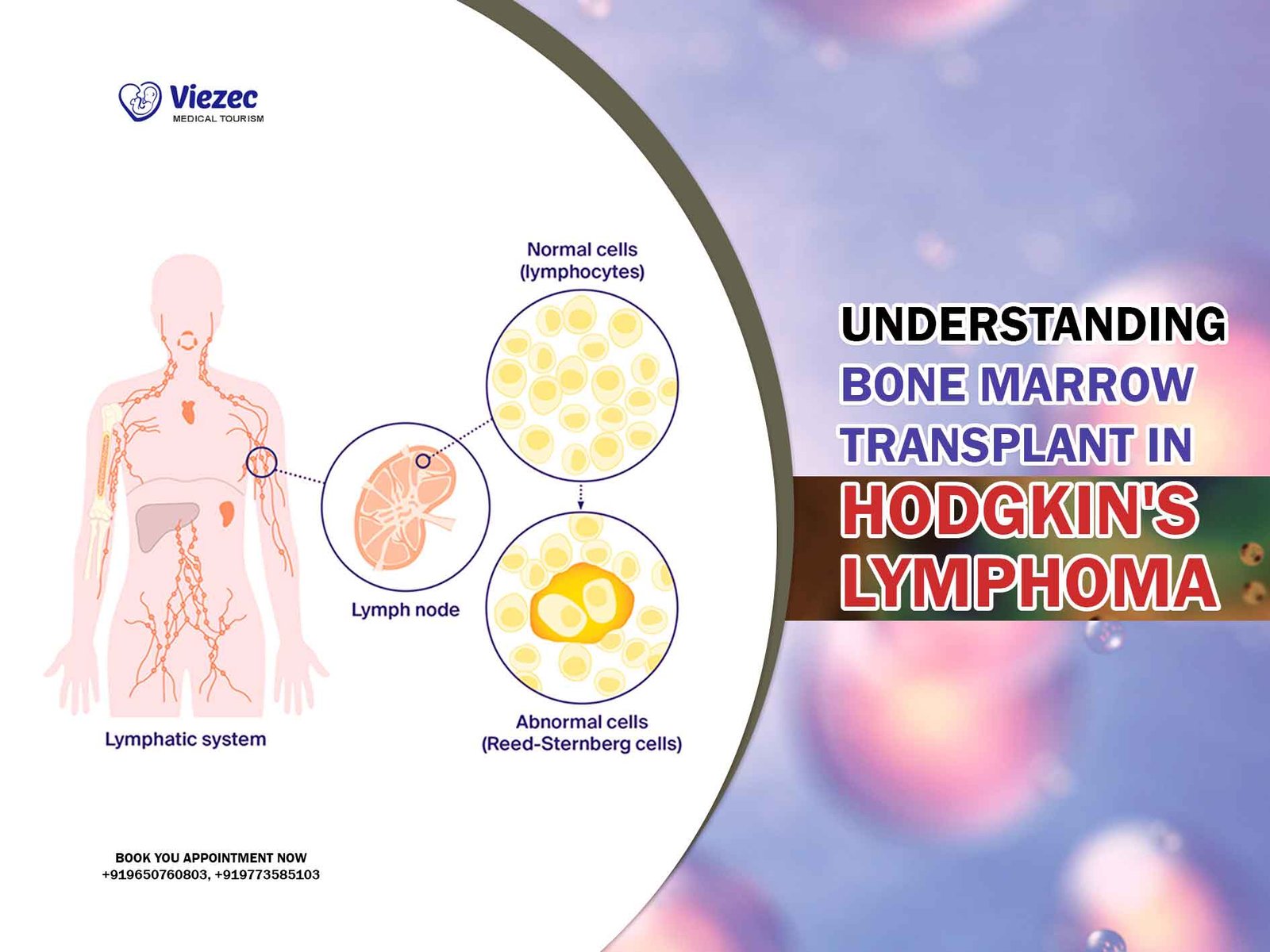
Genetic matching in bone marrow transplantation is crucial to minimize the risk of GVHD and ensure the graft’s success. The human leukocyte antigen (HLA) system, a group of genes located on chromosome 6, plays a vital role in the immune system’s ability to distinguish between self and non-self. In transplantation, the closer the HLA match between donor and recipient, the lower the risk of immune complications. Traditionally, finding a fully matched donor has been challenging, especially for patients from diverse ethnic backgrounds. This has driven the need to explore alternative donor sources, such as haploidentical donors, to increase the chances of finding a suitable match.
Haploidentical vs. Matched Sibling and Unrelated Donors
Haploidentical donors, who share half of the HLA genes with the recipient, offer a readily available source of stem cells, particularly when a fully matched sibling or unrelated donor is not found. While matched sibling donors provide the best outcomes due to close genetic compatibility, they are available for only about 30% of patients. Unrelated donor registries expand this pool but still leave many without matches. Haploidentical transplantation, therefore, serves as a critical alternative, though it comes with unique challenges such as increased risk of GVHD and graft failure due to the partial genetic mismatch.
Immunological Barriers and Risks
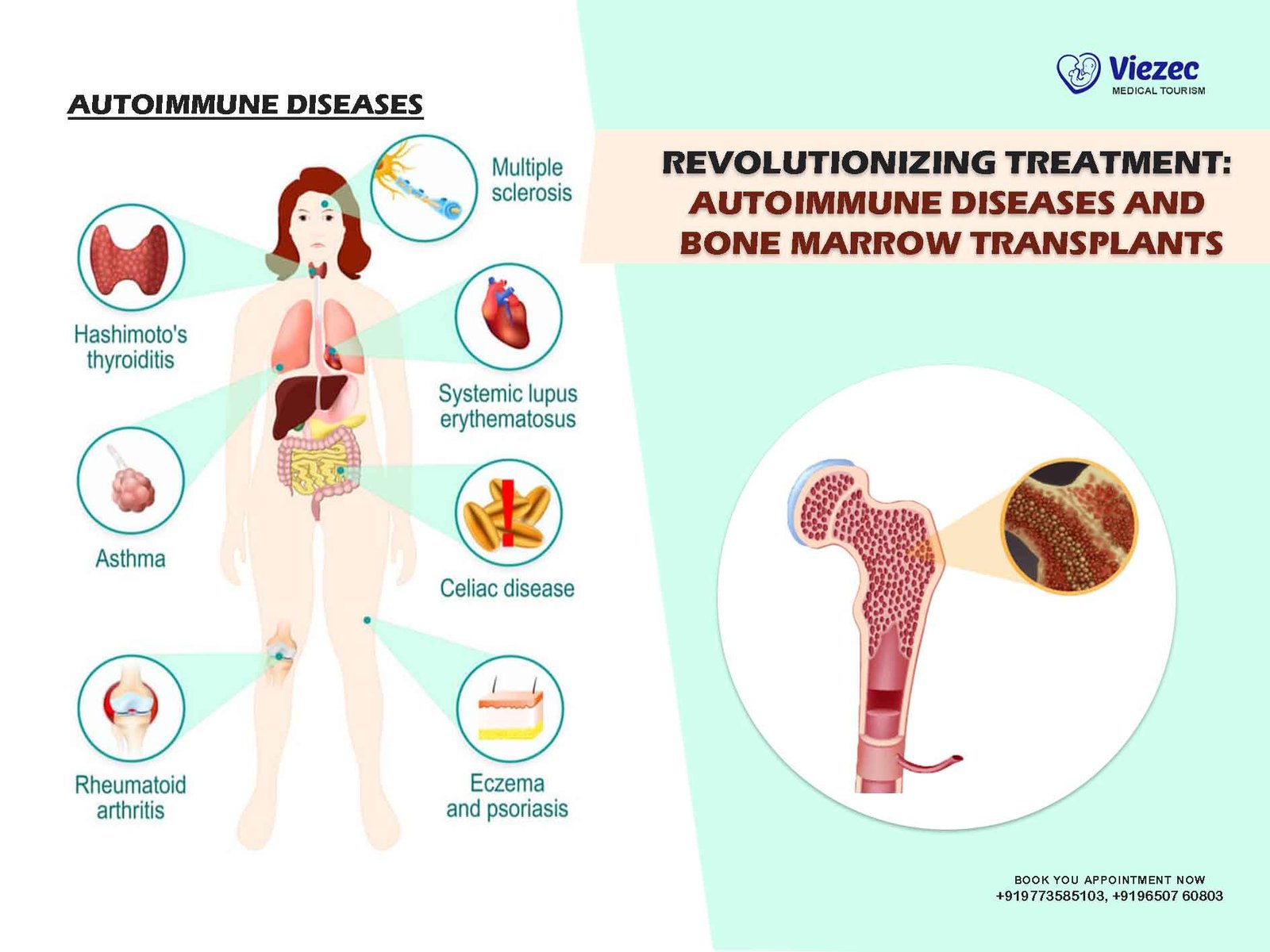
The primary immunological barriers in haploidentical transplantation include GVHD, where the donor’s immune cells attack the recipient’s tissues, and graft rejection, where the recipient’s immune system rejects the donor cells. Managing these risks requires a delicate balance of immunosuppression to prevent GVHD while allowing the donor cells to engraft and function properly. Advances in conditioning regimens, such as post-transplant cyclophosphamide, have been pivotal in reducing GVHD incidence and improving transplant outcomes. Despite these advances, managing these immunological challenges remains a critical aspect of haploidentical transplantation.
Advances in Overcoming Genetic Disparity
Innovations in the field of immunology and transplantation medicine have led to significant advances in overcoming the genetic disparities inherent in haploidentical transplantation. Techniques such as T-cell depletion, which removes specific immune cells from the donor graft, and the use of immunomodulatory drugs, have been crucial in reducing the risk of GVHD. Additionally, ongoing research into the role of regulatory T cells and other immune-modulating therapies holds promise for further improving outcomes. These advancements have made haploidentical transplants a safer and more effective option for patients lacking fully matched donors.
Patient and Donor Selection Criteria
Criteria for Patient Eligibility
Determining patient eligibility for haploidentical transplantation involves a comprehensive assessment of the individual’s disease status, overall health, and previous treatment history. Patients with high-risk hematologic malignancies, such as acute leukemias, or those with relapsed or refractory diseases are often considered candidates. Other factors include the patient’s age, comorbid conditions, and performance status. The goal is to identify patients who are likely to benefit from the procedure while minimizing the risks of complications. Pre-transplant evaluations typically include detailed physical examinations, imaging studies, and laboratory tests to ensure that the patient is fit for the intense conditioning regimens required for transplantation.
Identifying Suitable Donors
Family Member Matching
Finding a suitable donor is a critical step in the transplantation process. Haploidentical donors are usually first-degree relatives, such as parents, siblings, or children, who share half of the HLA genes with the recipient. The selection process involves HLA typing to confirm the degree of genetic match. In some cases, multiple family members may be potential donors, allowing for selection based on other factors such as health status and donor availability. The use of family members as donors not only increases the likelihood of finding a match but also facilitates a quicker and more coordinated transplantation process.
HLA Typing and Compatibility Testing
HLA typing is a sophisticated laboratory technique used to determine the specific HLA antigens present in both the donor and recipient. This process involves analyzing the DNA of white blood cells to identify the HLA alleles. Compatibility testing aims to find the closest possible match to reduce the risk of transplant-related complications. Even in haploidentical transplants, where a perfect match is not possible, a thorough understanding of the specific mismatches can help tailor the conditioning regimen and post-transplant care to improve outcomes.
Ethical and Social Considerations
The ethical and social considerations in haploidentical transplantation revolve around informed consent, donor autonomy, and the psychological impact on both donors and recipients. Ensuring that donors fully understand the risks and benefits of donation is crucial. Additionally, the decision to proceed with a haploidentical transplant often involves weighing the urgency of the patient’s medical need against the potential risks. Social dynamics within the family, including pressure to donate and the emotional toll on relationships, must be carefully managed to support both donors and recipients through the process.
Psychological Impact on Donors and Recipients
The psychological impact of haploidentical transplantation on both donors and recipients is profound. Donors may experience anxiety and stress related to the medical procedures and potential complications, while recipients face the emotional burden of undergoing a high-risk treatment. Comprehensive psychosocial support, including counseling and mental health services, is essential to address these challenges. Long-term follow-up care should also include regular assessments of psychological well-being to ensure that both donors and recipients receive the support they need throughout their recovery.
Transplantation Procedure
Pre-Transplant Conditioning
Chemotherapy Protocols
Pre-transplant conditioning involves intensive chemotherapy to eradicate the patient’s diseased bone marrow and suppress the immune system to prevent graft rejection. Chemotherapy protocols vary depending on the patient’s disease, overall health, and the degree of HLA mismatch. Commonly used regimens include agents such as cyclophosphamide, fludarabine, and busulfan. These drugs help create a favorable environment for the donor stem cells to engraft and proliferate. The intensity of the conditioning regimen is tailored to balance the need for effective disease control with the patient’s ability to tolerate the treatment.
Radiation Therapy
In addition to chemotherapy, radiation therapy is sometimes used in the conditioning regimen to enhance the eradication of malignant cells and further suppress the immune system. Total body irradiation (TBI) is a common approach, delivering a uniform dose of radiation to the entire body. The use of TBI can be particularly beneficial in treating certain leukemias and lymphomas. However, it also carries risks of long-term side effects, such as damage to healthy tissues and organs. Therefore, the decision to include radiation therapy in the conditioning regimen is carefully considered based on the patient’s individual circumstances.
Harvesting Bone Marrow
Bone Marrow Aspiration
Harvesting bone marrow involves collecting stem cells from the donor’s bone marrow, typically from the pelvic bones. This procedure, known as bone marrow aspiration, is performed under general or regional anesthesia. During the procedure, a needle is inserted into the bone, and the marrow is extracted into a syringe. The collected marrow is then processed to isolate the stem cells needed for transplantation. Bone marrow aspiration is a relatively safe procedure, but it may cause temporary discomfort and fatigue in the donor.
Peripheral Blood Stem Cell Collection
An alternative to bone marrow aspiration is peripheral blood stem cell (PBSC) collection, which involves mobilizing stem cells from the bone marrow into the bloodstream using medications like granulocyte colony-stimulating factor (G-CSF). Once the stem cells are in the bloodstream, they are collected through a process called apheresis, which separates the stem cells from the blood and returns the remaining blood components to the donor. PBSC collection is less invasive than bone marrow aspiration and has become the preferred method for many donors and transplant centers due to its efficiency and reduced recovery time.
Transplant Infusion and Immediate Care
The actual transplantation process involves infusing the harvested stem cells into the recipient’s bloodstream, similar to a blood transfusion. This procedure is typically performed in a specialized transplant unit with close monitoring for any immediate reactions. Post-infusion, the focus is on supportive care to manage side effects and complications, such as nausea, infections, and organ dysfunction. The patient remains in the hospital for several weeks to ensure the stem cells engraft and begin producing healthy blood cells. This period is critical for monitoring and addressing any complications promptly.
Post-Transplant Monitoring and Care
Graft Versus Host Disease (GVHD) Management
Managing GVHD is one of the most significant challenges following haploidentical transplantation. GVHD occurs when the donor’s immune cells attack the recipient’s tissues, leading to a range of symptoms from mild skin rashes to severe organ damage. Immunosuppressive medications, such as corticosteroids and calcineurin inhibitors, are used to prevent and treat GVHD. Early detection and prompt management of GVHD are crucial to improving patient outcomes. Ongoing research into new therapies and biomarkers for GVHD holds promise for more effective and targeted treatments in the future.
Infection Prevention and Control
Patients undergoing haploidentical transplantation are at high risk for infections due to the immunosuppressive nature of the conditioning regimen and the prolonged period of immune reconstitution. Infection prevention and control measures include prophylactic antibiotics, antifungal, and antiviral medications. Strict hygiene protocols and protective isolation practices are also implemented to minimize exposure to pathogens. Regular monitoring for signs of infection and prompt treatment of any infectious complications are essential components of post-transplant care.
Long-term Follow-up and Quality of Life
Long-term follow-up care is crucial for monitoring the patient’s recovery and addressing any late effects of the transplantation. Regular check-ups, blood tests, and imaging studies are conducted to assess the patient’s hematologic status and detect any recurrence of the underlying disease. Additionally, long-term follow-up includes managing chronic GVHD, monitoring for secondary cancers, and addressing any psychosocial issues. Improving the quality of life for transplant recipients is a key focus, involving multidisciplinary support from healthcare providers, mental health professionals, and social workers.
Clinical Outcomes and Research
Success Rates and Prognostic Factors
The success rates of haploidentical transplantation have improved significantly over the years, with survival rates now comparable to those of matched unrelated donor transplants. Prognostic factors influencing outcomes include the patient’s disease status at the time of transplant, the degree of HLA mismatch, and the effectiveness of GVHD prevention strategies. Early-stage disease and good performance status are associated with better outcomes. Ongoing research aims to refine conditioning regimens, enhance GVHD management, and develop novel therapies to further improve survival rates and reduce complications.
Comparative Studies with Other Transplant Types
Comparative studies have shown that haploidentical transplants can achieve outcomes similar to those of matched sibling and unrelated donor transplants, particularly with advances in GVHD prophylaxis and supportive care. These studies highlight the potential of haploidentical transplantation to fill the gap for patients without fully matched donors. Differences in outcomes are often attributed to variations in conditioning regimens, donor selection criteria, and post-transplant care protocols. Continued comparative research is essential to identify best practices and optimize treatment strategies across different types of transplants.
Innovative Therapies and Future Directions
Immunotherapy and T-cell Engineering
Innovative therapies, such as immunotherapy and T-cell engineering, are transforming the landscape of haploidentical transplantation. Techniques like chimeric antigen receptor (CAR) T-cell therapy and natural killer (NK) cell therapy are being integrated into transplant protocols to enhance anti-tumor activity and reduce the risk of relapse. These approaches harness the body’s immune system to target and eliminate residual disease, offering a promising addition to traditional transplantation methods. Ongoing clinical trials are exploring the safety and efficacy of these novel therapies in combination with haploidentical transplants.
Gene Editing and Personalized Medicine
Gene editing technologies, such as CRISPR-Cas9, hold significant potential for personalized medicine in haploidentical transplantation. These technologies allow for precise modifications of donor or recipient cells to enhance compatibility and reduce the risk of complications. Personalized medicine approaches aim to tailor conditioning regimens, immunosuppressive therapies, and supportive care based on the individual’s genetic and clinical profile. This personalized approach promises to improve outcomes and reduce the long-term side effects of transplantation, paving the way for more effective and patient-specific treatments.
Case Studies and Real-world Applications
Case studies and real-world applications of haploidentical transplantation provide valuable insights into the practical challenges and successes of this treatment approach. These studies highlight the diversity of patient populations, the variability in clinical practice, and the impact of new therapies and protocols. Real-world data help refine transplant guidelines, improve patient selection criteria, and enhance post-transplant care strategies. Sharing experiences and outcomes from different transplant centers worldwide contributes to the collective knowledge and continuous improvement of haploidentical transplantation practices.
Ethical, Legal, and Policy Considerations
Informed Consent and Patient Autonomy
Ensuring informed consent and respecting patient autonomy are fundamental ethical principles in haploidentical transplantation. Patients and donors must receive comprehensive information about the risks, benefits, and potential outcomes of the procedure. This includes a clear explanation of the transplant process, possible complications, and long-term follow-up requirements. Informed consent involves a collaborative decision-making process where patients and their families are actively engaged in understanding their treatment options and making choices aligned with their values and preferences.
Regulatory and Institutional Guidelines
Regulatory and institutional guidelines play a crucial role in maintaining the safety and ethical standards of haploidentical transplantation. These guidelines encompass donor selection, conditioning regimens, GVHD management, and post-transplant care protocols. Adherence to these guidelines ensures consistency and quality across different transplant centers. Regulatory bodies, such as the Food and Drug Administration (FDA) and European Medicines Agency (EMA), provide oversight and approval for new therapies and clinical trials, ensuring that advancements in transplantation are evidence-based and safe for patients.
Access to Transplantation and Healthcare Disparities
Access to haploidentical transplantation is influenced by healthcare disparities, including socioeconomic factors, geographic location, and availability of specialized transplant centers. Efforts to improve access involve expanding donor registries, increasing public awareness, and reducing financial barriers. Addressing healthcare disparities is essential to ensure that all patients, regardless of their background, have the opportunity to benefit from this life-saving treatment. Policymakers, healthcare providers, and advocacy groups must work together to create equitable access to transplantation services.
International Perspectives and Collaborative Efforts
International collaboration is vital in advancing the field of haploidentical transplantation. Sharing knowledge, resources, and best practices across countries enhances the quality and effectiveness of transplant programs globally. Collaborative research initiatives, such as multinational clinical trials and data-sharing platforms, contribute to a deeper understanding of transplantation biology and improve patient outcomes. International organizations, such as the World Marrow Donor Association (WMDA), facilitate cooperation and support the development of global standards and guidelines for haploidentical transplantation.
FAQs
1. What is a haploidentical bone marrow transplant?
A haploidentical bone marrow transplant involves using a donor who shares half of the HLA genes with the recipient, typically a parent, sibling, or child. This type of transplant expands the donor pool, making it possible for more patients to receive potentially life-saving treatments.
2. What are the risks associated with haploidentical transplantation?
The primary risks include graft-versus-host disease (GVHD), where the donor’s immune cells attack the recipient’s tissues, and infections due to the immunosuppressive conditioning regimen. Advances in immunosuppression and supportive care have significantly reduced these risks.
3. How is a suitable donor selected for a haploidentical transplant?
Suitable donors are usually first-degree relatives who share half of the HLA genes with the recipient. HLA typing and compatibility testing are conducted to confirm the genetic match. Family members are often preferred due to their availability and quick coordination.
4. What are the long-term outcomes of haploidentical transplantation?
Long-term outcomes have improved significantly, with survival rates now comparable to those of matched unrelated donor transplants. Factors influencing outcomes include the patient’s disease status, the degree of HLA mismatch, and advancements in GVHD prevention and management.
For more detailed information and resources, please visit us online or contact your healthcare provider.