Introduction to MSCs and the Blood-Brain Barrier
What Are Mesenchymal Stem Cells (MSCs)?
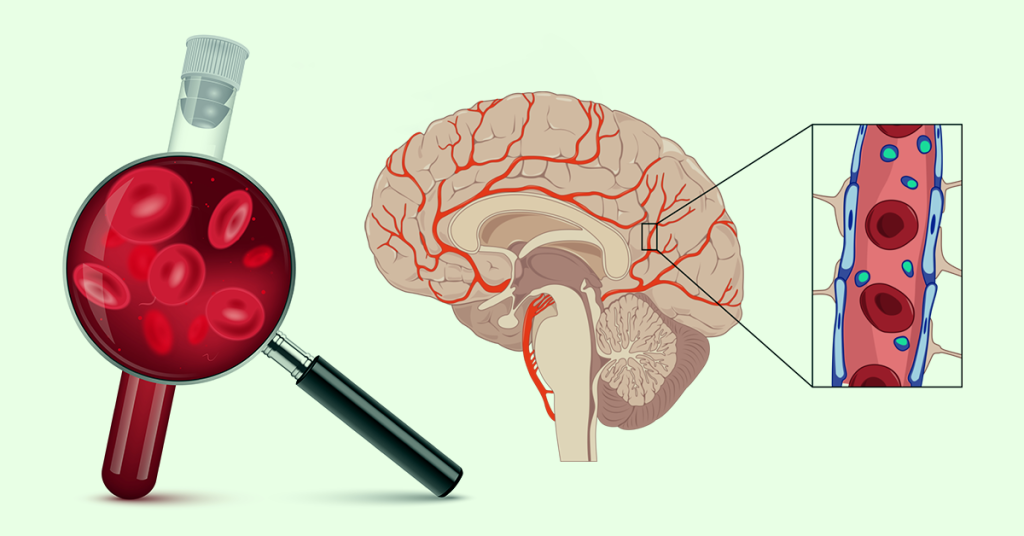
Mesenchymal stem cells, often abbreviated as MSCs, are a remarkable class of adult stem cells with the ability to develop into various tissue types—like bone, cartilage, and fat. While they’re most commonly sourced from bone marrow, MSCs can also be harvested from umbilical cord blood, adipose (fat) tissue, and even dental pulp.
But what makes MSCs truly special isn’t just their versatility in tissue repair—it’s their powerful anti-inflammatory and immune-modulating abilities. These features position MSCs as one of the most promising tools in modern regenerative medicine, offering new hope for conditions once thought untreatable.
Why the Blood-Brain Barrier Matters in Brain Health
Think of the blood-brain barrier (BBB) as the brain’s highly selective security gate. It’s a protective shield that controls what enters and exits the brain’s environment. This barrier defends against toxins and pathogens, keeping the brain stable and functioning smoothly.
However, the same barrier that protects us also limits us—especially when we try to deliver therapeutic agents to the brain. Most drugs, proteins, and even beneficial cells like MSCs struggle to make it through. That’s why scientists have been fascinated with finding ways to help MSCs cross this barrier safely.
The Core Challenge — Crossing the BBB
For a long time, researchers believed MSCs were simply too large and complex to pass through the tightly regulated BBB. And for the most part, they were right. The BBB doesn’t make exceptions easily.
But recent scientific breakthroughs have flipped this narrative. Under certain conditions—like inflammation or with assistance from chemokines—MSCs have been observed migrating across the BBB. This development has sparked new hope in treating devastating neurological diseases like Alzheimer’s, Parkinson’s, and multiple sclerosis.