Neurological disorders encompass a wide range of conditions that affect the brain, spinal cord, and nerves throughout the body. These disorders can result in a variety of symptoms, including motor, sensory, and cognitive impairments, significantly impacting an individual’s quality of life. Two prominent neurological disorders are Multiple Sclerosis (MS) and Motor Neuron Disease (MND), each with distinct pathophysiologies, symptoms, and treatment approaches. Understanding these disorders is crucial for early diagnosis, effective management, and improving patient outcomes. This article delves into the key differences between MS and MND, providing a comprehensive overview of each condition.
Importance of Understanding MS and MND
Understanding the differences between Multiple Sclerosis and Motor Neuron Disease is vital for both medical professionals and the general public. MS primarily affects the central nervous system, causing demyelination of nerve fibers, while MND involves the degeneration of motor neurons responsible for controlling voluntary muscles. Accurate diagnosis and differentiation between these two disorders can lead to more targeted treatments, better management strategies, and improved patient support. Additionally, increased awareness and knowledge about MS and MND can foster empathy, reduce stigma, and encourage research funding for these debilitating conditions.
Defining Multiple Sclerosis (MS)
What is Multiple Sclerosis?
Multiple Sclerosis is a chronic autoimmune disorder that affects the central nervous system (CNS), which includes the brain and spinal cord. In MS, the immune system mistakenly attacks the protective sheath (myelin) that covers nerve fibers, leading to inflammation and subsequent damage. This demyelination disrupts the normal flow of electrical impulses along the nerves, resulting in a wide range of neurological symptoms. MS can cause physical, cognitive, and emotional challenges, and its progression and severity can vary greatly among individuals.
Types of Multiple Sclerosis
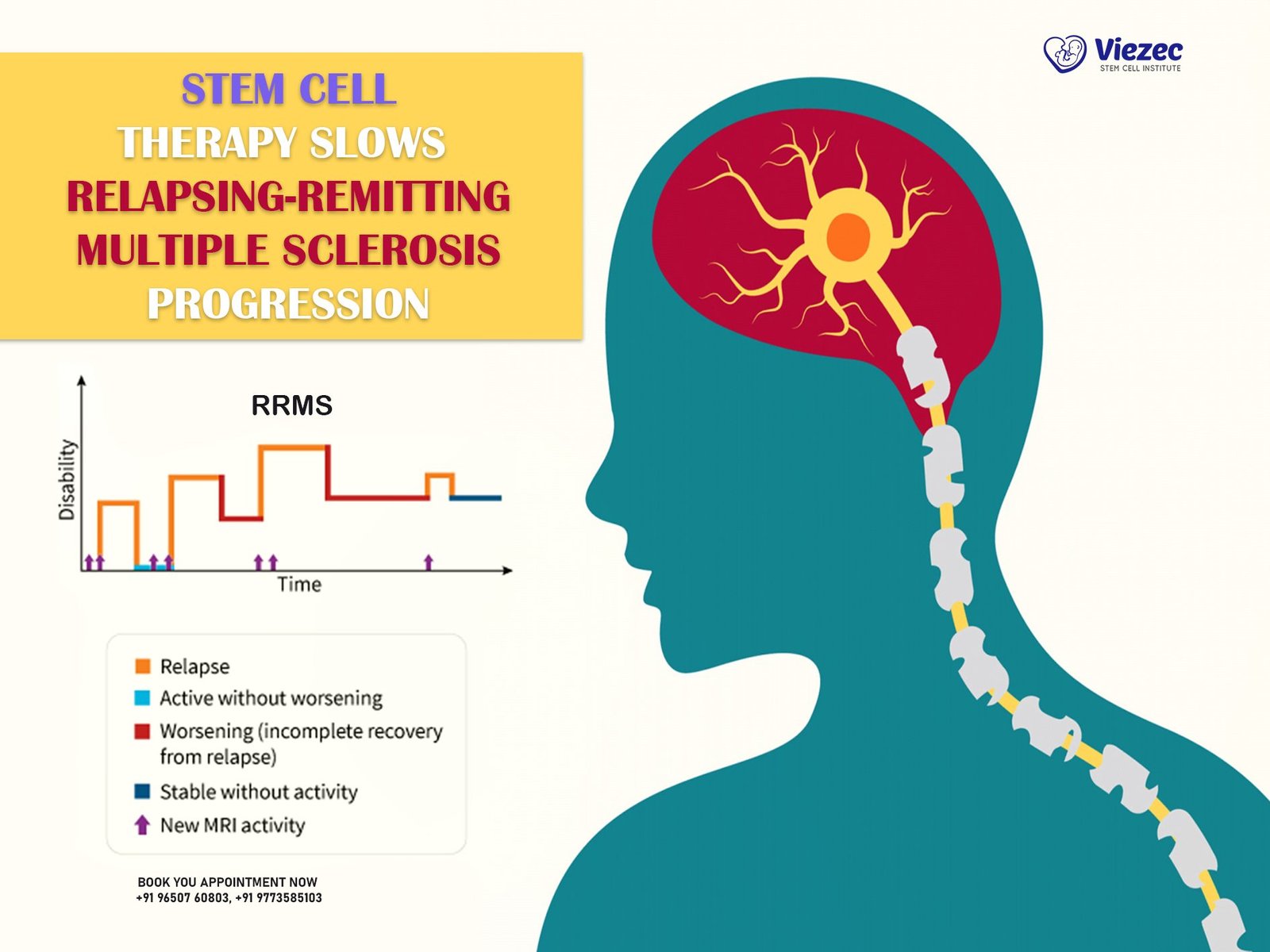
Relapsing-Remitting MS (RRMS)
Relapsing-Remitting MS is the most common form of MS, characterized by episodes of new or worsening symptoms (relapses) followed by periods of partial or complete recovery (remissions). During remission, symptoms may improve or disappear entirely, but the disease remains active, and relapses can occur unpredictably. RRMS affects approximately 85% of individuals diagnosed with MS and often transitions to secondary-progressive MS over time.
Primary-Progressive MS (PPMS)
Primary-Progressive MS is a less common form of MS, affecting about 10-15% of individuals with the disease. Unlike RRMS, PPMS is characterized by a steady progression of neurological impairment from the onset, without distinct relapses or remissions. Symptoms gradually worsen over time, and the rate of progression can vary. PPMS can be more challenging to diagnose and treat due to its continuous nature.
Secondary-Progressive MS (SPMS)
Secondary-Progressive MS is a stage of MS that follows an initial relapsing-remitting course. Over time, the disease transitions to a more progressive form, with a gradual worsening of symptoms and fewer or no relapses. SPMS can occur many years after the initial diagnosis of RRMS and represents a significant shift in the disease course. The progression in SPMS can be steady or occur in steps, with occasional plateaus.
Progressive-Relapsing MS (PRMS)
Progressive-Relapsing MS is the rarest form of MS, characterized by a progressive course from the onset, similar to PPMS, but with occasional acute relapses. Unlike RRMS, individuals with PRMS do not experience periods of remission. Instead, they continue to experience a steady decline in function, with intermittent relapses that further exacerbate symptoms. PRMS affects a small percentage of individuals with MS and is often more challenging to manage.
Causes and Risk Factors
The exact cause of Multiple Sclerosis remains unknown, but it is believed to result from a combination of genetic and environmental factors. Genetic predisposition plays a role, as individuals with a family history of MS are at a higher risk. Environmental factors, such as low vitamin D levels, smoking, and certain viral infections, may also contribute to the development of MS. Additionally, MS is more prevalent in women and typically diagnosed between the ages of 20 and 40. Understanding these risk factors is essential for identifying individuals at higher risk and developing preventive strategies.
Defining Motor Neuron Disease (MND)
What is Motor Neuron Disease?
Motor Neuron Disease is a group of progressive neurological disorders that affect the motor neurons, the nerve cells responsible for controlling voluntary muscle movements. The most common form of MND is Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease. MND leads to the degeneration and death of motor neurons, resulting in muscle weakness, atrophy, and loss of voluntary control. Over time, MND can affect speech, swallowing, and breathing, significantly impacting an individual’s quality of life and leading to severe disability.
Types of Motor Neuron Disease
Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis is the most prevalent form of MND, accounting for the majority of cases. ALS affects both upper and lower motor neurons, leading to progressive muscle weakness, twitching, and atrophy. Symptoms typically start in the limbs or bulbar muscles (responsible for speech and swallowing) and gradually spread to other parts of the body. ALS is characterized by a relentless progression, and the majority of individuals with ALS succumb to respiratory failure within three to five years of diagnosis.
Progressive Bulbar Palsy (PBP)
Progressive Bulbar Palsy primarily affects the bulbar muscles, which control speech, chewing, and swallowing. PBP is often considered a variant of ALS, as many individuals with PBP eventually develop ALS symptoms. Early signs of PBP include slurred speech, difficulty swallowing, and weakness in the facial and throat muscles. As the disease progresses, it can lead to significant communication and nutritional challenges, severely impacting daily life.
Primary Lateral Sclerosis (PLS)
Primary Lateral Sclerosis is a rare form of MND that affects only the upper motor neurons, leading to progressive muscle stiffness, spasticity, and weakness. Unlike ALS, PLS does not involve the lower motor neurons, and the progression is generally slower. PLS primarily affects the muscles in the lower limbs, but it can also impact the upper limbs and bulbar muscles. While PLS can significantly affect mobility and quality of life, it is not typically fatal.
Progressive Muscular Atrophy (PMA)
Progressive Muscular Atrophy primarily affects the lower motor neurons, leading to muscle weakness, wasting, and fasciculations (involuntary muscle twitches). PMA has a slower progression compared to ALS and does not usually involve the upper motor neurons. Symptoms often begin in the hands or lower limbs and gradually spread to other parts of the body. While PMA can lead to significant disability, individuals with PMA generally have a longer survival compared to those with ALS.
Causes and Risk Factors
The causes of Motor Neuron Disease are not fully understood, but a combination of genetic and environmental factors is believed to play a role. Genetic mutations are responsible for familial cases of MND, accounting for about 10% of all cases. Sporadic cases, which occur without a family history, are thought to result from a complex interplay of genetic predisposition and environmental triggers. Potential risk factors for MND include age, gender (males are more commonly affected), and exposure to certain toxins or chemicals. Ongoing research aims to identify specific genetic and environmental factors that contribute to the development of MND.
Pathophysiology and Mechanisms
Pathophysiology of MS
Demyelination Process
The hallmark of Multiple Sclerosis is the demyelination process, where the immune system attacks and damages the myelin sheath that surrounds nerve fibers in the central nervous system. Myelin is essential for the efficient transmission of electrical impulses along nerves. In MS, this damage disrupts the normal communication between the brain and the rest of the body, leading to the wide range of symptoms experienced by individuals with the disease. The demyelination process is often accompanied by the formation of scar tissue (sclerosis) in the affected areas.
Immune System Involvement
MS is considered an autoimmune disease, where the body’s immune system mistakenly targets its own tissues. In MS, immune cells, particularly T-cells and B-cells, play a crucial role in the inflammatory process that leads to demyelination. These immune cells cross the blood-brain barrier and initiate an attack on myelin, causing inflammation and damage to nerve fibers. The exact triggers for this autoimmune response are not fully understood, but it is believed to involve a combination of genetic predisposition and environmental factors.
Pathophysiology of MND
Motor Neuron Degeneration
Motor Neuron Disease is characterized by the progressive degeneration and death of motor neurons, the nerve cells responsible for controlling voluntary muscles. Motor neurons are divided into upper motor neurons (located in the brain) and lower motor neurons (located in the spinal cord and brainstem). In MND, both types of motor neurons can be affected, leading to muscle weakness, atrophy, and loss of function. The exact mechanisms behind motor neuron degeneration are not fully understood, but several factors, including genetic mutations and abnormal protein aggregation, are believed to play a role.
Genetic and Environmental Factors
Genetic mutations are a significant factor in the development of familial MND cases. Mutations in genes such as SOD1, C9orf72, and TDP-43 have been linked to both familial and sporadic forms of MND. These genetic mutations can lead to the production of abnormal proteins that accumulate and cause damage to motor neurons. Environmental factors, such as exposure to toxins, heavy metals, or viral infections, may also
contribute to the development of sporadic MND cases. The interaction between genetic susceptibility and environmental triggers is a focus of ongoing research in understanding MND pathogenesis.
Symptoms and Clinical Manifestations
Symptoms of Multiple Sclerosis
Sensory Symptoms
Sensory symptoms are common in individuals with Multiple Sclerosis and can include numbness, tingling, and a “pins and needles” sensation. These symptoms often affect the limbs and can vary in intensity and duration. Some individuals may also experience altered sensations, such as burning or itching, which can be bothersome and impact daily activities. Sensory symptoms in MS are usually the result of demyelination and subsequent disruption of nerve signal transmission.
Motor Symptoms
Motor symptoms in MS can include muscle weakness, spasticity, and difficulty with coordination and balance. These symptoms can affect any part of the body and may lead to difficulties with walking, writing, or performing other fine motor tasks. Spasticity, or increased muscle tone, can cause stiffness and painful muscle contractions. Motor symptoms can fluctuate, with periods of improvement and worsening, depending on the disease activity and progression.
Cognitive Symptoms
Cognitive symptoms are often present in individuals with MS and can include difficulties with memory, attention, and executive function. Cognitive impairment can impact daily functioning, work performance, and overall quality of life. Some individuals with MS may also experience mood changes, such as depression or anxiety, which can further complicate the management of the disease. Cognitive symptoms are thought to result from both direct damage to the brain and the overall burden of the disease on the central nervous system.
Symptoms of Motor Neuron Disease
Muscle Weakness and Atrophy
Muscle weakness and atrophy are hallmark symptoms of Motor Neuron Disease. As motor neurons degenerate and die, the muscles they control become progressively weaker and eventually waste away. This can lead to difficulties with movements such as walking, lifting, and gripping objects. Muscle atrophy can affect various parts of the body, depending on which motor neurons are affected, and can result in significant disability.
Speech and Swallowing Difficulties
Speech and swallowing difficulties are common in individuals with MND, particularly in those with bulbar involvement. As the muscles responsible for speech and swallowing weaken, individuals may experience slurred speech, difficulty articulating words, and challenges with chewing and swallowing food. These symptoms can lead to communication barriers, nutritional challenges, and an increased risk of aspiration and respiratory complications.
Respiratory Issues
Respiratory issues are a significant concern in individuals with MND, especially as the disease progresses. The muscles involved in breathing, including the diaphragm and intercostal muscles, can weaken, leading to respiratory insufficiency. This can result in shortness of breath, difficulty breathing, and an increased risk of respiratory infections. Respiratory failure is often the leading cause of death in individuals with advanced MND, highlighting the importance of respiratory support and management in these patients.
Diagnostic Approaches
Diagnosing Multiple Sclerosis
MRI and Imaging Techniques
Magnetic Resonance Imaging (MRI) is a critical tool in the diagnosis of Multiple Sclerosis. MRI can detect lesions or plaques in the brain and spinal cord that are indicative of demyelination. These lesions often appear as bright spots on MRI scans and can provide evidence of disease activity and progression. MRI is also used to monitor the effectiveness of treatment and detect any new or worsening lesions over time.
Lumbar Puncture and CSF Analysis
A lumbar puncture, or spinal tap, is a procedure used to collect cerebrospinal fluid (CSF) from the spinal canal. Analysis of CSF can provide valuable information for the diagnosis of MS. The presence of oligoclonal bands, which are abnormal proteins produced by the immune system, in the CSF is a common finding in individuals with MS. CSF analysis can help confirm the diagnosis and rule out other conditions that may mimic MS.
Evoked Potentials Tests
Evoked potentials tests measure the electrical activity in the brain in response to specific stimuli. These tests can help identify abnormalities in nerve signal transmission, which are common in MS. Visual evoked potentials (VEP) test the response to visual stimuli, while somatosensory evoked potentials (SSEP) test the response to sensory stimuli. Abnormal evoked potentials can provide additional evidence of demyelination and support the diagnosis of MS.
Diagnosing Motor Neuron Disease
Electromyography (EMG)
Electromyography is a diagnostic test used to assess the health of muscles and the motor neurons that control them. EMG involves inserting a thin needle electrode into the muscle to record electrical activity during muscle contraction and rest. Abnormal EMG findings, such as spontaneous muscle activity or reduced motor unit recruitment, can indicate motor neuron damage and support the diagnosis of MND.
Nerve Conduction Studies (NCS)
Nerve Conduction Studies measure the speed and strength of electrical signals as they travel along nerves. NCS can help differentiate between disorders affecting the nerves, muscles, and neuromuscular junction. In individuals with MND, NCS may show reduced nerve conduction velocity and amplitude, indicating motor neuron damage. NCS is often performed in conjunction with EMG to provide a comprehensive assessment of nerve and muscle function.
Genetic Testing
Genetic testing can identify specific mutations associated with familial forms of MND. Mutations in genes such as SOD1, C9orf72, and TARDBP can be detected through blood tests or other genetic analysis methods. Identifying these genetic mutations can provide valuable information for diagnosis, prognosis, and potential participation in clinical trials. Genetic testing is particularly important for individuals with a family history of MND or those presenting with early-onset disease.
Treatment Options and Management
Treatment for Multiple Sclerosis
Disease-Modifying Therapies (DMTs)
Disease-Modifying Therapies are the cornerstone of MS treatment and aim to reduce the frequency and severity of relapses, slow disease progression, and prevent new lesions from forming. DMTs include injectable medications, oral treatments, and intravenous infusions. Commonly used DMTs include interferon beta, glatiramer acetate, and newer agents such as fingolimod, dimethyl fumarate, and ocrelizumab. The choice of DMT depends on the individual’s disease course, tolerance, and overall health.
Symptomatic Treatments
In addition to DMTs, symptomatic treatments are used to manage specific symptoms of MS, such as muscle spasticity, pain, fatigue, and bladder dysfunction. Medications such as muscle relaxants, pain relievers, and antidepressants can help alleviate symptoms and improve quality of life. Physical therapy, occupational therapy, and speech therapy can also provide valuable support in managing MS-related symptoms and maintaining function.
Lifestyle and Supportive Care
Lifestyle modifications and supportive care are essential components of MS management. Regular exercise, a balanced diet, and adequate rest can help individuals maintain overall health and well-being. Supportive care, including counseling and support groups, can provide emotional and psychological support for individuals with MS and their families. Access to rehabilitation services, assistive devices, and adaptive technologies can also enhance independence and quality of life.
Treatment for Motor Neuron Disease
Riluzole and Other Medications
Riluzole is the only FDA-approved medication for ALS and has been shown to prolong survival by a few months. Riluzole works by reducing the release of glutamate, a neurotransmitter that can be toxic to motor neurons. Other medications, such as edaravone, have also been approved for ALS and may provide additional benefits. Symptomatic treatments, such as muscle relaxants, antispasmodics, and pain relievers, can help manage specific symptoms of MND.
Physical and Occupational Therapy
Physical and occupational therapy play a crucial role in managing MND by helping individuals maintain strength, mobility, and independence. Physical therapy focuses on exercises to improve muscle strength, flexibility, and balance, while occupational therapy addresses daily living activities and the use of assistive devices. Regular therapy sessions can help slow the progression of disability and improve overall quality of life.
Respiratory Support
As MND progresses, respiratory muscles weaken, leading to breathing difficulties. Respiratory support, such as non-invasive ventilation (NIV) and mechanical ventilation, can help manage respiratory insufficiency and improve survival. NIV involves using a mask or nasal device to provide positive pressure ventilation, while mechanical ventilation requires a more invasive approach with a tracheostomy. Early intervention with respiratory support can significantly enhance quality of life for individuals with advanced MND.
Emerging Therapies and Research
Stem Cell Therapy in MS
Types of Stem Cell Approaches
Stem cell therapy is a promising area of research for the treatment of MS. Various types of stem cells, including hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs), are being investigated for their potential to repair damaged myelin and modulate the immune response. HSCs, derived from bone marrow or blood, can regenerate immune cells and reset the immune system. MSCs, found in various tissues, have anti-inflammatory and regenerative properties that may help repair myelin and promote nerve function.
Current Clinical Trials and Results
Several clinical trials are underway to evaluate the safety and efficacy of stem cell therapy in MS. Early results have shown promise, with some studies reporting improvements in disease activity, relapse rates, and disability progression. However, more research is needed to determine the long-term benefits and potential risks of stem cell therapy. Ongoing trials aim to optimize treatment protocols, identify the most effective stem cell types, and understand the mechanisms of action.
Stem Cell Therapy in MND
Types of Stem Cell Approaches
Stem cell therapy is also being explored as a potential treatment for MND. Approaches under investigation include the use of neural stem cells (NSCs) to replace damaged motor neurons and the use of MSCs to provide neuroprotective effects and modulate inflammation. NSCs can differentiate into motor neurons and integrate into the existing neural network, while MSCs can secrete factors that promote motor neuron survival and reduce inflammation.
Current Clinical Trials and Results
Clinical trials for stem cell therapy in MND are in the early stages, with some studies showing encouraging results. Initial trials have demonstrated the safety and feasibility of stem cell transplantation, with some participants experiencing stabilization or improvement in symptoms. However, larger, randomized controlled trials are needed to confirm these findings and determine the long-term efficacy and safety of stem cell therapy for MND. Ongoing research aims to refine stem cell delivery methods, optimize dosing, and identify the most suitable patient populations.
Conclusion and Future Directions
Summary of Key Differences
Multiple Sclerosis and Motor Neuron Disease are distinct neurological disorders with unique pathophysiologies, symptoms, and treatment approaches. MS is characterized by demyelination and immune system involvement, leading to a wide range of sensory, motor, and cognitive symptoms. In contrast, MND involves the degeneration of motor neurons, resulting in progressive muscle weakness, atrophy, and respiratory issues. Accurate diagnosis and differentiation between these disorders are crucial for effective management and improved patient outcomes.
Advancements in Research and Treatment
Advancements in research and treatment are continuously improving the outlook for individuals with MS and MND. The development of disease-modifying therapies and symptomatic treatments has significantly enhanced the management of MS, while ongoing research into stem cell therapy and other emerging treatments holds promise for both MS and MND. Increased understanding of the underlying mechanisms of these disorders is paving the way for more targeted and personalized treatment approaches.
Hope for the Future
While MS and MND remain challenging conditions, ongoing research, clinical trials, and advancements in medical technology offer hope for the future. Continued efforts to understand the causes and mechanisms of these disorders, coupled with the development of innovative treatments, have the potential to transform the lives of individuals affected by MS and MND. Collaborative research, increased awareness, and support from the medical community and the public are essential in driving progress and finding effective solutions for these debilitating diseases.
FAQs
1. What is the main difference between Multiple Sclerosis and Motor Neuron Disease?
The main difference between Multiple Sclerosis (MS) and Motor Neuron Disease (MND) lies in their pathophysiology. MS is an autoimmune disorder that affects the central nervous system, causing demyelination of nerve fibers. In contrast, MND involves the degeneration of motor neurons, leading to muscle weakness and atrophy.
2. Can stem cell therapy cure MS or MND?
Stem cell therapy is still in the experimental stages for both MS and MND. While early results from clinical trials are promising, more research is needed to determine the long-term efficacy and safety of stem cell therapy. Currently, there is no cure for either MS or MND.
3. What are the common symptoms of MS?
Common symptoms of MS include sensory disturbances (such as numbness and tingling), muscle weakness, spasticity, balance and coordination difficulties, cognitive impairment, and fatigue. Symptoms can vary widely among individuals and can fluctuate over time.
4. How is MND diagnosed?
MND is diagnosed through a combination of clinical evaluation, electromyography (EMG), nerve conduction studies (NCS), and genetic testing. These tests help assess muscle and nerve function and identify any genetic mutations associated with familial MND cases. For more information, visit us online.