Parkinson’s Disease (PD) and Multiple Sclerosis (MS) are both chronic neurological disorders that affect the central nervous system but in markedly different ways. Parkinson’s Disease primarily impacts movement, causing symptoms like tremors, stiffness, and bradykinesia due to the loss of dopamine-producing neurons in the brain. It is classified as a neurodegenerative disorder, meaning it progressively worsens over time. On the other hand, Multiple Sclerosis is an autoimmune disease where the immune system mistakenly attacks the myelin sheath, the protective covering of nerve fibers in the central nervous system. This leads to communication problems between the brain and the rest of the body, resulting in a wide range of symptoms including motor, sensory, and cognitive impairments.
Prevalence and Demographics
The prevalence of Parkinson’s Disease and Multiple Sclerosis varies geographically and demographically. Parkinson’s Disease affects about 1% of the population over 60, making it one of the most common neurodegenerative disorders among the elderly. It is slightly more prevalent in men than women. In contrast, Multiple Sclerosis typically affects younger adults, with most diagnoses occurring between the ages of 20 and 50. Women are approximately two to three times more likely to develop MS than men. The prevalence of MS also varies by location, being more common in regions farther from the equator, suggesting potential environmental or genetic factors influencing its distribution.
Importance of Understanding Differences
Understanding the differences between Parkinson’s Disease and Multiple Sclerosis is crucial for several reasons. Accurate diagnosis is essential for effective treatment, as the management strategies for each condition differ significantly. Additionally, awareness of these differences can aid in patient education, helping individuals and their families understand their condition and what to expect. Misdiagnosis or delayed diagnosis can lead to inappropriate treatments, exacerbation of symptoms, and unnecessary stress for patients. Moreover, research into these diseases often overlaps, and distinguishing their unique characteristics can lead to more targeted and effective therapeutic approaches.
Causes and Risk Factors
Genetic Factors
Parkinson’s Disease
Genetic factors play a notable role in the development of Parkinson’s Disease, particularly in early-onset cases. Mutations in specific genes such as SNCA, LRRK2, and PARK2 have been linked to an increased risk of PD. These genetic mutations can influence the production and accumulation of alpha-synuclein, a protein that aggregates in the brains of individuals with PD, leading to neuronal damage. While familial cases of PD are relatively rare, accounting for about 10-15% of all cases, the presence of these genetic markers can significantly increase an individual’s risk of developing the disease.
Multiple Sclerosis
Multiple Sclerosis also has a genetic component, although it is less direct than in Parkinson’s Disease. Certain genes associated with the immune system, such as the HLA-DRB1 gene, have been identified as risk factors for MS. These genetic factors influence the immune system’s ability to distinguish between the body’s own tissues and foreign invaders, leading to the autoimmune response that characterizes MS. While having a family member with MS increases an individual’s risk, the likelihood of inheriting the disease is still relatively low, indicating that other factors, including environmental triggers, also play a significant role.
Environmental Factors
Parkinson’s Disease
Environmental factors are believed to contribute to the development of Parkinson’s Disease. Exposure to pesticides and herbicides has been linked to an increased risk, as these chemicals can cause oxidative stress and neuronal damage. Additionally, rural living and drinking well water, which may contain contaminants, have been associated with a higher incidence of PD. Head injuries are another environmental risk factor; repeated trauma to the brain can lead to chronic inflammation and the degeneration of dopamine-producing neurons.
Multiple Sclerosis
For Multiple Sclerosis, environmental factors are also significant. Geographic location is one of the most well-documented factors, with higher prevalence rates in temperate regions. This has led to hypotheses about the role of vitamin D, as people living farther from the equator have less exposure to sunlight, which is necessary for vitamin D production. Low levels of vitamin D have been associated with an increased risk of MS. Viral infections, particularly Epstein-Barr virus (EBV), have also been implicated in triggering the autoimmune response that leads to MS. Smoking is another risk factor, as it can contribute to the inflammatory processes involved in the disease.
Other Risk Factors
Age and Gender
Age and gender play important roles in the risk profiles of both diseases. Parkinson’s Disease is predominantly a condition of older adults, with the risk increasing significantly after the age of 60. Men are more likely to develop PD than women, though the reasons for this gender disparity are not fully understood. In contrast, Multiple Sclerosis typically affects younger individuals, with the majority of cases diagnosed between ages 20 and 50. Women are at a higher risk of developing MS compared to men, which is thought to be related to hormonal differences and immune system functioning.
Family History
A family history of Parkinson’s Disease or Multiple Sclerosis can increase an individual’s risk of developing the respective condition. For Parkinson’s Disease, having a first-degree relative with the disease can double or even triple the risk, especially if there are known genetic mutations present. Similarly, a family history of Multiple Sclerosis increases the risk, although the inheritance pattern is less straightforward than in PD. Siblings or children of individuals with MS have a higher likelihood of developing the disease compared to the general population, suggesting a combination of genetic predisposition and shared environmental factors.
Symptoms and Clinical Features
Motor Symptoms
Parkinson’s Disease
Motor symptoms are the hallmark of Parkinson’s Disease and are often the first indicators of the condition. These include resting tremors, typically starting in one hand, and progressing to other parts of the body. Bradykinesia, or slowness of movement, is another key symptom, making everyday activities increasingly difficult. Rigidity, or muscle stiffness, can also occur, leading to a decreased range of motion. Postural instability, resulting in balance issues and frequent falls, is a common symptom in later stages of the disease. These motor symptoms are primarily due to the loss of dopamine-producing neurons in the substantia nigra, a region of the brain that regulates movement.
Multiple Sclerosis
Multiple Sclerosis can also present with motor symptoms, although they are often more varied than those seen in Parkinson’s Disease. Muscle weakness and spasticity are common, affecting mobility and coordination. Patients may experience tremors, although these are typically intention tremors (occurring during purposeful movement) rather than resting tremors. Gait problems, such as difficulty walking or maintaining balance, are frequent, and some individuals may require mobility aids. MS can also cause muscle spasms and cramps, adding to the physical discomfort and impairing motor function. These symptoms result from the demyelination of nerve fibers, which disrupts the transmission of signals between the brain and muscles.
Non-Motor Symptoms
Parkinson’s Disease
In addition to motor symptoms, Parkinson’s Disease is associated with a range of non-motor symptoms that can significantly impact quality of life. Cognitive impairment, including problems with memory, attention, and executive function, is common. Depression and anxiety are also prevalent, often exacerbated by the chronic nature of the disease. Autonomic dysfunction can lead to symptoms such as constipation, orthostatic hypotension (a drop in blood pressure when standing up), and bladder issues. Sleep disturbances, including REM sleep behavior disorder and insomnia, are frequent. These non-motor symptoms can sometimes precede the onset of motor symptoms, complicating the diagnostic process.
Multiple Sclerosis
Multiple Sclerosis also presents with a variety of non-motor symptoms. Cognitive issues, such as difficulties with memory, attention, and problem-solving, are common and can impact daily functioning. Fatigue is one of the most pervasive symptoms, affecting up to 90% of individuals with MS and significantly impairing their ability to perform daily activities. Sensory disturbances, such as numbness, tingling, and pain, are frequent and can affect different parts of the body. Vision problems, including optic neuritis (inflammation of the optic nerve) and double vision, are also typical. Additionally, MS can cause bladder and bowel dysfunction, sexual dysfunction, and mood disorders like depression and anxiety.
Progression and Variability
The progression and variability of Parkinson’s Disease and Multiple Sclerosis differ considerably. Parkinson’s Disease is generally a slowly progressive disorder, with symptoms worsening gradually over years or even decades. However, the rate of progression can vary among individuals. Some may experience a relatively stable course with manageable symptoms, while others may have a more rapid decline in motor and cognitive functions. The introduction of medications can alleviate symptoms and improve quality of life but does not halt the disease’s progression.
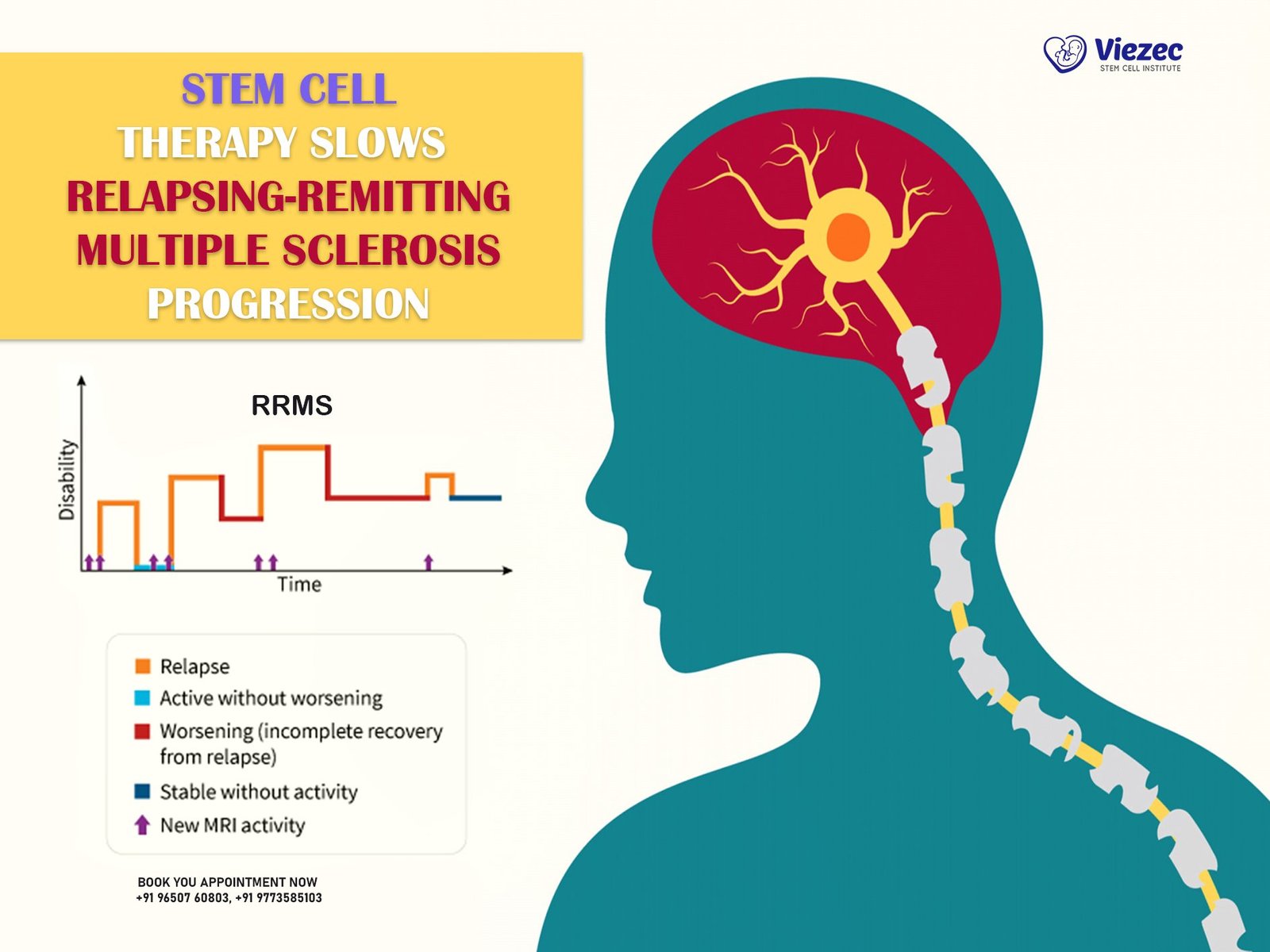
Multiple Sclerosis, on the other hand, has several distinct patterns of progression. The most common form is relapsing-remitting MS (RRMS), characterized by episodes of acute symptoms (relapses) followed by periods of partial or complete recovery (remissions). Over time, many individuals with RRMS transition to secondary progressive MS (SPMS), where the disease steadily worsens without clear relapses and remissions. Primary progressive MS (PPMS), affecting about 10-15% of individuals, involves a gradual worsening of symptoms from the onset without relapses or remissions. The variability in MS progression makes it challenging to predict the disease course for any given individual.
Diagnosis and Diagnostic Criteria
Initial Assessment
Medical History
The initial assessment for both Parkinson’s Disease and Multiple Sclerosis involves a thorough medical history to understand the patient’s symptoms, their onset, and their progression. For Parkinson’s Disease, the presence of motor symptoms such as tremors, bradykinesia, and rigidity are key indicators. A detailed history of these symptoms, including their duration and any factors that alleviate or exacerbate them, is essential. For Multiple Sclerosis, the focus is on identifying episodes of neurological symptoms that may indicate relapses. These can include visual disturbances, motor and sensory deficits, and cognitive changes. The pattern of these episodes, including their frequency and recovery, helps in differentiating MS from other neurological conditions.
Neurological Examination
A comprehensive neurological examination is crucial for diagnosing both conditions. For Parkinson’s Disease, the examination focuses on assessing motor function, including evaluating tremors, muscle tone, reflexes, and coordination. The presence of bradykinesia and rigidity, along with resting tremors, strongly suggests PD. Additionally, postural stability tests and gait analysis are performed. For Multiple Sclerosis, the neurological examination aims to identify signs of central nervous system involvement. This includes testing visual acuity and eye movements, assessing muscle strength and tone, checking reflexes, and evaluating coordination and balance. Sensory testing is also conducted to detect areas of numbness or tingling.
Diagnostic Tests
MRI and Imaging Techniques
Magnetic Resonance Imaging (MRI) is a pivotal tool in the diagnosis of both Parkinson’s Disease and Multiple Sclerosis, though its role and findings differ. In Parkinson’s Disease, MRI is used primarily to rule out other conditions that could mimic PD symptoms, such as strokes or brain tumors. While MRI cannot definitively diagnose PD, advanced imaging techniques like DaTscan, which assesses dopamine transporter levels, can support the diagnosis. For Multiple Sclerosis, MRI is a cornerstone diagnostic tool, revealing characteristic lesions or plaques in the brain and spinal cord. These lesions, caused by demyelination, are often located in specific areas such as the periventricular region, cerebellum, and spinal cord.
Blood Tests and Biomarkers
Blood tests are more commonly used to exclude other conditions rather than to diagnose Parkinson’s Disease or Multiple Sclerosis directly. In Parkinson’s Disease, routine blood tests can help rule out metabolic and systemic diseases that might present with similar symptoms. Emerging research is exploring specific biomarkers, such as alpha-synuclein levels, that could aid in PD diagnosis in the future. In Multiple Sclerosis, blood tests are used to exclude infections and other inflammatory conditions that can mimic MS. Additionally, cerebrospinal fluid (CSF) analysis, obtained through a lumbar puncture, can reveal oligoclonal bands, which are indicative of an immune response within the central nervous system and support an MS diagnosis.
Differential Diagnosis
Differential diagnosis is crucial in distinguishing Parkinson’s Disease and Multiple Sclerosis from other neurological conditions with similar presentations. For Parkinson’s Disease, differentiating it from other parkinsonian syndromes, such as multiple system atrophy (MSA) and progressive supranuclear palsy (PSP), is essential. These conditions share some symptoms with PD but have distinct clinical features and progression patterns. For Multiple Sclerosis, conditions like neuromyelitis optica spectrum disorder (NMOSD), which also involves demyelination but follows a different course and treatment response, must be considered. Other autoimmune and inflammatory diseases, such as lupus or sarcoidosis, can also present with neurological symptoms similar to MS and need to be ruled out through comprehensive diagnostic evaluations.
Pathophysiology and Disease Mechanisms
Neurodegeneration in Parkinson’s Disease
The pathophysiology of Parkinson’s Disease centers on the progressive degeneration of dopamine-producing neurons in the substantia nigra, a region of the midbrain. Dopamine is a crucial neurotransmitter involved in regulating movement, and its depletion leads to the motor symptoms characteristic of PD. The exact cause of this neurodegeneration remains unclear, but it is believed to involve a combination of genetic susceptibility, environmental exposures, and cellular processes such as oxidative stress and mitochondrial dysfunction. The accumulation of alpha-synuclein protein into Lewy bodies within neurons is a hallmark of PD, contributing to neuronal death and the spread of pathology throughout the brain.
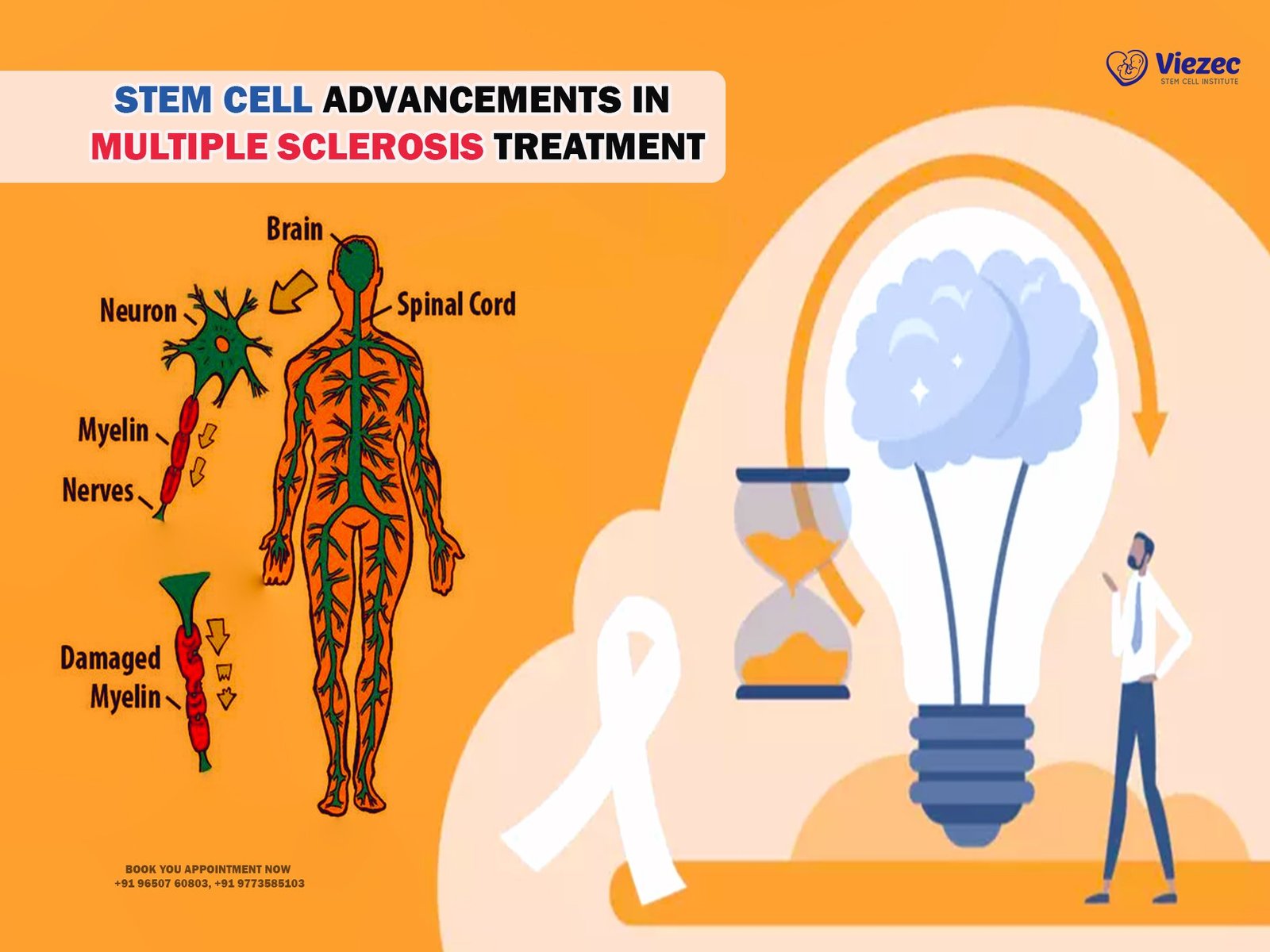
Demyelination in Multiple Sclerosis
Multiple Sclerosis is characterized by the immune system’s attack on the myelin sheath, the protective covering of nerve fibers in the central nervous system. This demyelination disrupts the efficient transmission of electrical impulses along the nerves, leading to the diverse neurological symptoms of MS. The immune attack also causes inflammation and subsequent damage to the underlying nerve fibers, resulting in permanent neurological deficits over time. The exact trigger for this autoimmune response is not fully understood, but it likely involves a combination of genetic predisposition, environmental factors such as viral infections, and possibly a breakdown in the blood-brain barrier that allows immune cells to enter the central nervous system.
Common Pathological Features
While Parkinson’s Disease and Multiple Sclerosis have distinct pathophysiological mechanisms, they share some common features related to neurodegeneration and inflammation. Both diseases involve a progressive loss of neuronal function, leading to chronic disability. Inflammation plays a role in both conditions, though it is more central to MS pathogenesis. Oxidative stress and mitochondrial dysfunction are also implicated in the neuronal damage observed in both diseases. Additionally, protein misfolding and aggregation, such as alpha-synuclein in PD and possibly other proteins in MS, contribute to the disease processes. Understanding these shared and distinct mechanisms can help in developing targeted therapies and improving disease management.
Treatment Approaches
Medications
Parkinson’s Disease
Medications for Parkinson’s Disease primarily aim to replenish dopamine levels or mimic its effects in the brain. Levodopa is the most effective treatment, often combined with carbidopa to prevent its breakdown before reaching the brain. Dopamine agonists, such as pramipexole and ropinirole, directly stimulate dopamine receptors. Monoamine oxidase-B (MAO-B) inhibitors, like selegiline and rasagiline, prevent the breakdown of dopamine. Catechol-O-methyltransferase (COMT) inhibitors, such as entacapone, extend the duration of levodopa’s effects. These medications can significantly improve motor symptoms but may have side effects such as dyskinesias, hallucinations, and orthostatic hypotension, requiring careful management and adjustment.
Multiple Sclerosis
Multiple Sclerosis treatment focuses on modifying the disease course, managing relapses, and alleviating symptoms. Disease-modifying therapies (DMTs) aim to reduce the frequency and severity of relapses and slow disease progression. These include injectable medications like interferon-beta and glatiramer acetate, oral medications such as fingolimod, dimethyl fumarate, and teriflunomide, and intravenous treatments like natalizumab and ocrelizumab. Corticosteroids, such as methylprednisolone, are used to manage acute relapses. Symptomatic treatments, including muscle relaxants, pain relievers, and medications for fatigue, bladder dysfunction, and cognitive issues, are also essential in improving the quality of life for individuals with MS.
Physical and Occupational Therapy
Physical and occupational therapy play crucial roles in managing Parkinson’s Disease and Multiple Sclerosis, helping to maintain mobility, function, and independence. For Parkinson’s Disease, physical therapy focuses on improving gait, balance, and flexibility through exercises and techniques that enhance movement. Occupational therapy helps patients adapt daily activities to their changing abilities, recommending assistive devices and modifications to the home environment. For Multiple Sclerosis, physical therapy aims to address muscle weakness, spasticity, and coordination issues, incorporating exercises to maintain strength and mobility. Occupational therapy helps manage fatigue, suggesting energy conservation strategies and adaptive equipment to facilitate daily tasks.
Surgical Interventions
Deep Brain Stimulation (DBS) for Parkinson’s
Deep Brain Stimulation (DBS) is a surgical treatment option for Parkinson’s Disease, particularly for patients with advanced disease or those who do not respond well to medications. DBS involves implanting electrodes in specific brain regions, such as the subthalamic nucleus or globus pallidus internus. These electrodes deliver electrical impulses that help regulate abnormal neural activity, improving motor symptoms such as tremors, rigidity, and bradykinesia. DBS can significantly enhance the quality of life for patients with PD, allowing them to reduce their medication doses and manage symptoms more effectively. However, it is a complex procedure with potential risks, including infection, bleeding, and cognitive or mood changes.
Plasmapheresis for Multiple Sclerosis
Plasmapheresis, or plasma exchange, is a procedure used in severe cases of Multiple Sclerosis, particularly during acute relapses that do not respond to corticosteroids. It involves removing the patient’s blood, separating the plasma (which contains antibodies and other immune components), and replacing it with a substitute, such as albumin or donor plasma. This process helps to remove the harmful antibodies that contribute to the autoimmune attack on the myelin sheath. Plasmapheresis can provide temporary relief from severe symptoms and is typically reserved for cases of aggressive relapses or certain types of MS, such as neuromyelitis optica spectrum disorder (NMOSD).
Stem Cell Research and Therapies
Current Research Status
Parkinson’s Disease
Stem cell research for Parkinson’s Disease is a rapidly evolving field, with ongoing studies exploring the potential of stem cells to replace the lost dopamine-producing neurons and restore normal brain function. Researchers are investigating various types of stem cells, including embryonic stem cells, induced pluripotent stem cells (iPSCs), and mesenchymal stem cells, to determine their efficacy and safety in treating PD. Preclinical studies have shown promising results, and several clinical trials are underway to assess the feasibility of stem cell transplantation in humans. These trials aim to determine the optimal type of stem cells, delivery methods, and potential long-term benefits and risks.
Multiple Sclerosis
In Multiple Sclerosis, stem cell research focuses on repairing the damaged myelin sheath and modulating the immune response to prevent further attacks. Hematopoietic stem cell transplantation (HSCT), which involves harvesting and reinfusing the patient’s own stem cells after high-dose immunosuppressive therapy, has shown potential in halting disease progression and improving symptoms in some patients. Mesenchymal stem cells (MSCs) are also being studied for their immunomodulatory properties and ability to promote tissue repair. Clinical trials are ongoing to evaluate the safety and efficacy of these approaches, with some promising results suggesting that stem cell therapies could offer new hope for individuals with MS.
Potential Benefits and Challenges
The potential benefits of stem cell therapies for Parkinson’s Disease and Multiple Sclerosis include the restoration of lost functions, reduction in disease progression, and improvement in the quality of life. For Parkinson’s Disease, successful stem cell transplantation could replenish the dopamine-producing neurons, alleviating motor symptoms and reducing reliance on medications. For Multiple Sclerosis, stem cell therapies could repair damaged myelin, reduce inflammation, and restore neurological function. However, significant challenges remain, including ensuring the safety and long-term viability of transplanted cells, avoiding immune rejection, and addressing ethical concerns associated with the use of embryonic stem cells.
Clinical Trials and Future Directions
Numerous clinical trials are exploring the use of stem cell therapies for Parkinson’s Disease and Multiple Sclerosis, with researchers continually refining techniques and approaches to enhance efficacy and safety. For Parkinson’s Disease, trials are investigating the optimal source of stem cells, delivery methods, and adjunctive therapies to support the survival and integration of transplanted cells. In Multiple Sclerosis, trials are focusing on identifying the most effective stem cell types and protocols for HSCT and MSC therapies. Future directions in stem cell research aim to address current limitations, develop personalized treatment approaches, and ultimately bring these innovative therapies into clinical practice.
Living with Parkinson’s Disease and Multiple Sclerosis
Daily Life and Mobility
Living with Parkinson’s Disease and Multiple Sclerosis presents unique challenges that require adaptive strategies to maintain independence and quality of life. For individuals with Parkinson’s Disease, daily life adjustments may include incorporating regular physical exercise, following a balanced diet, and using assistive devices to manage motor symptoms. Mobility issues, such as shuffling gait and balance problems, necessitate modifications to the home environment to prevent falls and ensure safety. In Multiple Sclerosis, daily life can be impacted by fatigue, muscle weakness, and coordination difficulties. Energy conservation techniques, assistive devices, and home adaptations can help manage these challenges and enhance mobility.
Emotional and Psychological Impact
Both Parkinson’s Disease and Multiple Sclerosis can have profound emotional and psychological effects on individuals and their families. Depression, anxiety, and mood disorders are common in both conditions, often exacerbated by the chronic and progressive nature of the diseases. Individuals with Parkinson’s Disease may experience apathy, loss of motivation, and social withdrawal, while cognitive changes, such as memory impairment and executive dysfunction, can also occur. In Multiple Sclerosis, emotional lability, cognitive difficulties, and stress related to disease unpredictability are significant concerns. Psychological support, including counseling, support groups, and medication, plays a vital role in managing these emotional and psychological challenges.
Support Systems and Resources
A robust support system is essential for individuals living with Parkinson’s Disease and Multiple Sclerosis. Family, friends, healthcare providers, and patient support organizations provide crucial assistance and resources. Support groups offer a sense of community, allowing individuals to share experiences, gain knowledge, and receive emotional support. Specialized healthcare teams, including neurologists, physiotherapists, occupational therapists, and mental health professionals, collaborate to provide comprehensive care. Educational resources, such as informational materials, online forums, and workshops, help individuals and their caregivers stay informed about the latest treatments, research developments, and coping strategies.
Prognosis and Quality of Life
Disease Progression
Parkinson’s Disease
The progression of Parkinson’s Disease varies significantly among individuals, with some experiencing a slower decline in function while others face rapid deterioration. The disease typically follows a gradual course, with motor symptoms worsening over time and non-motor symptoms becoming more prominent. Early-stage PD is often managed effectively with medications, but as the disease advances, motor complications, such as dyskinesias and fluctuations, become more challenging to control. Non-motor symptoms, including cognitive impairment, autonomic dysfunction, and sleep disturbances, also impact quality of life. Research into disease-modifying treatments aims to slow or halt progression, offering hope for improved outcomes.
Multiple Sclerosis
Multiple Sclerosis progression can be highly variable, with different disease courses and outcomes. Relapsing-remitting MS (RRMS) is characterized by episodes of neurological symptoms followed by periods of partial or complete recovery. Over time, many individuals with RRMS transition to secondary progressive MS (SPMS), marked by a gradual decline in function with fewer relapses. Primary progressive MS (PPMS) involves continuous worsening of symptoms from onset, with no distinct relapses. The rate of progression and degree of disability vary widely, influenced by factors such as early treatment initiation, disease-modifying therapy effectiveness, and individual patient characteristics.
Management of Symptoms
Long-term Medication Use
Long-term medication use is a cornerstone of managing Parkinson’s Disease and Multiple Sclerosis. For Parkinson’s Disease, adjusting medication regimens over time is necessary to balance symptom control and side effects. Regular follow-ups with healthcare providers ensure optimal dosing and address complications such as dyskinesias. In Multiple Sclerosis, adherence to disease-modifying therapies is critical in reducing relapse frequency and slowing disease progression. Symptomatic treatments, such as muscle relaxants, pain relievers, and medications for fatigue and cognitive issues, are tailored to individual needs. Regular monitoring and adjustments help manage side effects and maximize therapeutic benefits.
Lifestyle Adjustments
Lifestyle adjustments play a vital role in managing Parkinson’s Disease and Multiple Sclerosis, enhancing quality of life and overall well-being. For Parkinson’s Disease, incorporating regular physical activity, such as walking, yoga, and strength training, helps maintain mobility and flexibility. A balanced diet rich in antioxidants supports brain health. In Multiple Sclerosis, strategies to manage fatigue, such as pacing activities and prioritizing tasks, are essential. Physical exercise tailored to individual abilities, combined with a healthy diet and adequate rest, supports overall health. Stress management techniques, including mindfulness, meditation, and hobbies, contribute to emotional and psychological well-being.
Advances in Research and Hope for the Future
Ongoing research and advancements in understanding Parkinson’s Disease and Multiple Sclerosis offer hope for improved treatments and potential cures. In Parkinson’s Disease, breakthroughs in genetics, neurobiology, and neuroimaging are uncovering new targets for disease-modifying therapies. Innovative approaches, such as gene therapy, neuroprotective agents, and personalized medicine, are being explored. In Multiple Sclerosis, advances in immunology and regenerative medicine are paving the way for novel treatments, including stem cell therapies and remyelination strategies. Clinical trials and collaborative research efforts continue to drive progress, bringing new insights and potential breakthroughs that could transform the lives of individuals with these challenging conditions.
FAQs
What are the main differences between Parkinson’s Disease and Multiple Sclerosis?
Parkinson’s Disease primarily affects motor function due to the loss of dopamine-producing neurons in the brain, leading to symptoms such as tremors, rigidity, and bradykinesia. Multiple Sclerosis is an autoimmune disease that targets the myelin sheath of nerve fibers in the central nervous system, causing a wide range of neurological symptoms, including visual disturbances, muscle weakness, and coordination issues.
How are Parkinson’s Disease and Multiple Sclerosis diagnosed?
Diagnosis of Parkinson’s Disease involves a clinical assessment of motor symptoms, a neurological examination, and possibly imaging techniques like DaTscan. Multiple Sclerosis diagnosis relies on a combination of MRI findings showing characteristic brain and spinal cord lesions, cerebrospinal fluid analysis, and clinical evaluation of symptom patterns.
Can stem cell therapy cure Parkinson’s Disease and Multiple Sclerosis?
Stem cell therapy holds promise for treating both conditions, but it is not yet a cure. Ongoing research is exploring the potential of stem cells to replace damaged neurons in Parkinson’s Disease and repair myelin in Multiple Sclerosis. Clinical trials are underway to evaluate the safety and efficacy of these therapies.
What lifestyle changes can help manage Parkinson’s Disease and Multiple Sclerosis?
For Parkinson’s Disease, regular physical exercise, a balanced diet, and assistive devices can help manage symptoms and maintain mobility. In Multiple Sclerosis, energy conservation techniques, physical exercise tailored to individual abilities, and stress management strategies are essential. Both conditions benefit from psychological support and community resources.