Innovative Stem Cell Delivery Methods
Viezec uses advanced and minimally invasive delivery methods to ensure stem cells reach the targeted area safely and effectively. Our techniques are designed to maximize therapeutic benefits while prioritizing patient safety.
Learn About Our Techniques
Trusted by hundreds of patients worldwide for safe and effective stem cell therapy.
Why Delivery Method Matters
The way stem cells are delivered to the body directly affects treatment outcomes. At Viezec, we use advanced, minimally invasive delivery techniques that precisely target affected areas, maximize therapeutic benefits, and minimize risk for every patient.
Maximized Effectiveness
Proper delivery ensures stem cells reach the precise area of need, increasing the chances of optimal tissue regeneration and therapeutic success.
Enhanced Safety
Minimally invasive techniques reduce complications, prevent unwanted side effects, and allow patients to recover faster and more comfortably.
Targeted Precision
By delivering stem cells directly to the affected tissues or organs, we ensure targeted regeneration and better overall outcomes.
Stem Cell Delivery Methods

Intravenous (IV) Infusion
Stem cells are delivered through a vein for systemic distribution, ideal for conditions affecting multiple areas.

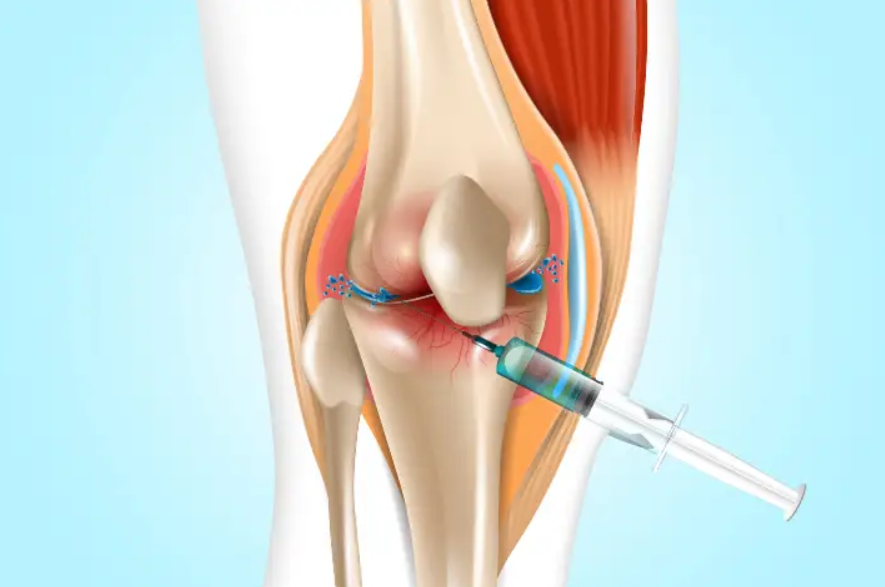
Intra-articular Injection
Direct injection into joints promotes healing and reduces inflammation for conditions like arthritis.

Intrathecal Injection
Stem cells are delivered into the spinal canal, supporting neurological conditions and CNS disorders.

Topical / Non-Invasive
Stem cells can be applied to skin wounds, eye conditions, or inhaled for respiratory benefits.

Advanced Techniques
Includes exosome therapy, cell sheets, and nanoparticle-based delivery for precise and effective treatment.
Safety and Precision
At Viezec, patient safety is our top priority. Our delivery methods are designed for precision, minimizing risks while maximizing therapeutic effectiveness. Every procedure follows strict clinical protocols and is performed by highly skilled medical professionals.
✓
Minimized Risks
Advanced protocols and minimally invasive techniques reduce complications and ensure patient safety.
✓
Precision Delivery
Stem cells are delivered exactly where needed for optimal therapeutic outcomes.
✓
Expert Medical Team
Our highly trained professionals follow strict clinical protocols for every procedure.
✓
Strict Protocols
Every procedure follows carefully monitored clinical protocols to ensure maximum safety.
Patient Experience During Treatment
At Viezec, we ensure every patient feels comfortable and informed throughout the treatment process. From pre-procedure consultation to post-treatment care, our team guides you step-by-step, prioritizing comfort, safety, and confidence in the therapy.
Step-by-Step Guidance
Our team explains each procedure stage, ensuring patients are informed and relaxed.
Comfort & Minimal Invasiveness
Our delivery methods are designed to minimize discomfort and reduce recovery time.
Post-Treatment Support
We provide continuous care and guidance to monitor progress and ensure safety.
Research-Backed Methods
Our stem cell delivery techniques are supported by extensive scientific research and clinical studies. Viezec combines cutting-edge technology with evidence-based practices to ensure the highest standards of treatment efficacy and patient safety.
Clinically Validated
Our methods are backed by peer-reviewed clinical studies demonstrating safety and efficacy.
Evidence-Based Protocols
Each delivery technique follows established protocols grounded in scientific evidence.
Continuous Innovation
We constantly refine our techniques based on the latest research to ensure optimal outcomes.
Frequently Asked Questions
What is the safest method for stem cell delivery?
Viezec uses minimally invasive and targeted delivery methods to ensure maximum safety and effectiveness for each patient.
How long does a typical procedure take?
Most delivery procedures take between 30 minutes to 2 hours depending on the technique and area being treated.
Will I experience pain during treatment?
Our methods are designed for minimal discomfort, and we provide supportive care to ensure patient comfort throughout the procedure.
How soon will I see results?
Results vary depending on the condition treated, but many patients begin noticing improvements within weeks after treatment.
Ready to Experience Safe and Effective Stem Cell Therapy?
Book a consultation with our expert medical team today and learn how our advanced delivery methods can help you achieve optimal results.
Book a Consultation
Trusted by hundreds of patients worldwide for safe and precise stem cell therapy.
This website uses cookies to improve your experience. If you continue to use this site, you agree with it.
Ok