Secondary-Progressive Multiple Sclerosis (SPMS) is a stage of multiple sclerosis (MS) characterized by a gradual worsening of neurological function over time. Unlike the initial relapsing-remitting phase, where patients experience periods of relapse and remission, SPMS involves a more steady progression of disability. This phase can occur with or without occasional relapses, minor remissions, or plateaus. The transition to SPMS typically marks a significant shift in the disease’s trajectory, often necessitating adjustments in treatment and management strategies. Understanding SPMS is crucial for both patients and healthcare providers as it informs the approach to care and expectations for disease progression.
Transition from Relapsing-Remitting MS to SPMS
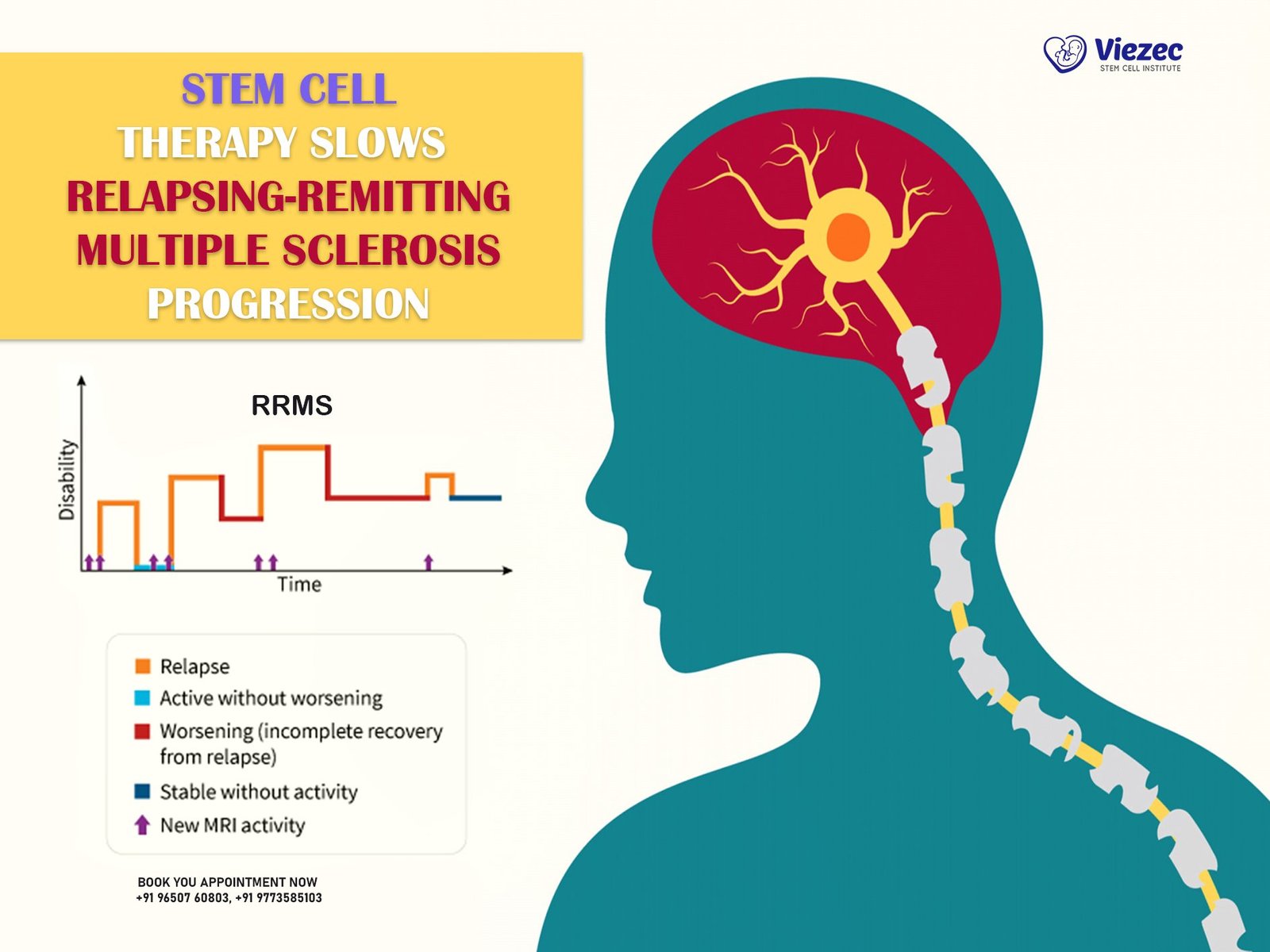
The transition from Relapsing-Remitting MS (RRMS) to SPMS is a critical phase in the disease course. This shift generally occurs after a period of relapses and remissions, where the disease begins to progress more steadily without significant recovery between episodes. The time frame for this transition varies widely among individuals, ranging from a few years to several decades after the initial diagnosis of RRMS. Early identification of this transition is essential for adapting treatment plans to manage symptoms effectively and to slow the progression of disability. Monitoring and regular assessments by healthcare professionals play a pivotal role in detecting this change early.
Prevalence and Demographics
SPMS affects a substantial portion of the MS population, with estimates suggesting that approximately 50-60% of individuals with RRMS will transition to SPMS within 10-20 years of their initial diagnosis. The prevalence of SPMS varies geographically and demographically, with certain populations exhibiting higher rates of progression. Factors such as age, gender, and the severity of initial relapses can influence the likelihood of developing SPMS. Typically, SPMS is more common in older individuals and slightly more prevalent in women, reflecting the overall gender distribution seen in MS. Understanding these demographics helps in anticipating and planning for the needs of those at risk.
Symptoms of Secondary-Progressive Multiple Sclerosis
Motor Symptoms
Weakness and Fatigue
One of the hallmark symptoms of SPMS is persistent weakness and fatigue. Unlike the intermittent fatigue experienced during the RRMS phase, SPMS-related fatigue is often more constant and debilitating. Patients may find it challenging to complete daily tasks and activities due to muscle weakness and a pervasive sense of tiredness. This can significantly impact quality of life, leading to increased dependency on others for assistance with routine activities. Addressing fatigue through a combination of medication, physical therapy, and lifestyle modifications is crucial in managing SPMS.
Spasticity and Muscle Stiffness
Spasticity and muscle stiffness are common motor symptoms in SPMS, often contributing to discomfort and difficulty with movement. Spasticity involves involuntary muscle contractions, leading to stiffness and tightness, which can affect mobility and coordination. This symptom can vary in severity, from mild stiffness to severe, painful contractions that hinder movement. Managing spasticity typically involves a combination of pharmacological treatments, such as muscle relaxants, and non-pharmacological approaches like physical therapy and stretching exercises to maintain muscle flexibility and reduce discomfort.
Sensory Symptoms
Numbness and Tingling
Sensory disturbances such as numbness and tingling are frequently reported by individuals with SPMS. These sensations can occur in various parts of the body and may fluctuate in intensity. Numbness often leads to a loss of sensation, making it difficult to perceive touch or temperature changes, which can increase the risk of injury. Tingling, often described as a “pins and needles” sensation, can be uncomfortable and distracting. These symptoms can affect daily functioning and quality of life, necessitating strategies to manage and mitigate their impact, including medications and physical therapy.
Pain and Discomfort
Pain is a significant symptom in SPMS, manifesting in various forms such as neuropathic pain, musculoskeletal pain, and spasticity-related pain. Neuropathic pain, resulting from nerve damage, can cause burning, shooting, or stabbing sensations. Musculoskeletal pain often arises from muscle strain and joint stress due to changes in mobility and posture. Effective pain management is crucial and may involve medications like anticonvulsants or antidepressants for neuropathic pain, along with physical therapy, massage, and other non-pharmacological interventions to alleviate discomfort and improve quality of life.
Cognitive Symptoms
Memory and Concentration Issues
Cognitive impairment is a significant concern in SPMS, affecting memory and concentration. Patients may experience difficulties with short-term memory, attention span, and the ability to process information quickly. These cognitive challenges can interfere with daily activities, work, and social interactions, leading to frustration and decreased independence. Cognitive rehabilitation strategies, including memory aids, structured routines, and cognitive exercises, can help manage these symptoms. Additionally, medications and lifestyle modifications, such as regular physical exercise and mental stimulation, may contribute to cognitive health.
Executive Function Difficulties
Executive function, which includes skills such as planning, organizing, and problem-solving, is often impaired in SPMS. Patients may struggle with tasks that require these cognitive processes, such as managing finances, organizing their day, or adapting to new situations. These difficulties can significantly impact daily life and increase reliance on caregivers. Cognitive rehabilitation, occupational therapy, and assistive technologies can provide support in managing executive function challenges. Encouraging patients to engage in activities that stimulate cognitive function can also be beneficial in maintaining these skills.
Emotional and Psychological Symptoms
Depression and Anxiety
Depression and anxiety are prevalent among individuals with SPMS, influenced by both the disease’s physical impact and the emotional burden of living with a chronic condition. Depression can manifest as persistent sadness, loss of interest in activities, and feelings of hopelessness. Anxiety may present as excessive worry, restlessness, and difficulty sleeping. Addressing these psychological symptoms is essential for overall well-being. Treatment options include psychotherapy, medications such as antidepressants and anxiolytics, and supportive interventions like support groups and stress management techniques to enhance emotional resilience.
Mood Swings and Irritability
Mood swings and irritability are common in SPMS, often resulting from the neurological changes associated with the disease and the stress of managing chronic symptoms. Patients may experience rapid shifts in mood, leading to frustration and strained relationships with family and caregivers. Identifying and addressing these mood disturbances is crucial for maintaining emotional stability. Treatment may involve a combination of pharmacological approaches, such as mood stabilizers, and non-pharmacological strategies like counseling, stress reduction techniques, and lifestyle modifications to promote emotional balance.
Diagnosis of Secondary-Progressive Multiple Sclerosis
Diagnostic Criteria
Diagnosing SPMS involves a comprehensive evaluation of clinical history, symptoms, and progression patterns. The diagnosis is primarily clinical, based on the observation of a gradual increase in disability independent of relapses over a period of time. Criteria for SPMS typically include a history of RRMS, a progressive worsening of neurological function, and the exclusion of other potential causes for the observed decline. Early and accurate diagnosis is critical for implementing appropriate treatment strategies and for differentiating SPMS from other forms of MS and neurological conditions.
MRI and Other Imaging Techniques
Magnetic Resonance Imaging (MRI) plays a pivotal role in diagnosing and monitoring SPMS. MRI can reveal changes in the brain and spinal cord associated with MS, such as the presence of new or enlarging lesions and atrophy. These imaging findings, combined with clinical assessments, help confirm the diagnosis and assess disease progression. Other imaging techniques, such as optical coherence tomography (OCT) and positron emission tomography (PET), may also be used to provide additional information about the extent of neurological damage and the involvement of other structures in the central nervous system.
Neurological Examination
A thorough neurological examination is essential in diagnosing SPMS. This examination evaluates various aspects of neurological function, including motor strength, coordination, reflexes, sensory perception, and cognitive abilities. Neurologists look for signs of disease progression, such as increased spasticity, weakness, and changes in gait or balance. Regular neurological assessments help track the progression of SPMS and guide treatment decisions. Detailed documentation of clinical findings over time is crucial for distinguishing SPMS from other neurological disorders and for optimizing patient management.
Differentiating SPMS from Other MS Types
Differentiating SPMS from other types of MS, such as primary-progressive MS (PPMS) and RRMS, is vital for appropriate management. SPMS is characterized by an initial relapsing-remitting phase followed by a progressive decline, while PPMS involves a steady progression from onset without relapses. Identifying this transition requires careful monitoring of symptom patterns, progression rates, and response to treatments. Clinicians utilize clinical history, imaging studies, and neurological examinations to distinguish SPMS from other forms of MS, ensuring that patients receive the most effective and tailored treatment approaches.
Treatment Options for Secondary-Progressive Multiple Sclerosis
Disease-Modifying Therapies (DMTs)
Immunomodulatory Drugs
Immunomodulatory drugs are a cornerstone in the treatment of SPMS. These medications work by modulating the immune system to reduce inflammation and slow disease progression. Examples include interferons and glatiramer acetate, which have been shown to decrease the frequency of relapses and delay the accumulation of disability. While these drugs are more commonly used in the RRMS phase, some evidence suggests they may still benefit individuals with SPMS, particularly those with ongoing relapses. Regular monitoring for side effects and effectiveness is crucial in managing these therapies.
Immunosuppressive Treatments
Immunosuppressive treatments, such as mitoxantrone, cyclophosphamide, and newer agents like ocrelizumab, are used to control the immune system’s overactivity in SPMS. These drugs aim to reduce the rate of progression and limit neurological damage. Due to their potent effects and potential for significant side effects, immunosuppressive treatments are
4o
often reserved for individuals with aggressive disease courses or inadequate responses to other therapies. Close monitoring by healthcare providers is essential to optimize treatment benefits while minimizing risks.
Symptomatic Treatments
Medications for Spasticity and Pain
Managing symptoms such as spasticity and pain is crucial in improving quality of life for individuals with SPMS. Medications such as baclofen and tizanidine are commonly prescribed to reduce muscle stiffness and spasms associated with spasticity. Neuropathic pain may be treated with anticonvulsants like gabapentin or pregabalin, which help alleviate nerve-related discomfort. Non-steroidal anti-inflammatory drugs (NSAIDs) and opioid analgesics may be used cautiously for musculoskeletal pain, taking into account their potential for side effects and addiction. Individualized treatment plans aim to balance symptom relief with safety and efficacy.
Cognitive and Emotional Management
Cognitive and emotional symptoms in SPMS may benefit from pharmacological interventions and supportive therapies. Medications such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) can alleviate depression and anxiety, improving overall well-being. Cognitive rehabilitation programs, including memory training and compensatory strategies, help maintain cognitive function and manage executive challenges. Psychotherapy, counseling, and participation in support groups provide emotional support, coping skills, and strategies to navigate the psychological impact of living with SPMS.
Physical and Occupational Therapy
Exercise and Rehabilitation Programs
Physical therapy and exercise programs play a crucial role in managing mobility and functional abilities in SPMS. These programs focus on strengthening muscles, improving flexibility, and maintaining balance and coordination. Aerobic exercises, such as swimming or stationary cycling, promote cardiovascular health and overall well-being. Rehabilitation strategies may also include gait training, assistive devices, and adaptive equipment to enhance independence and quality of life. Regular participation in these programs can help individuals with SPMS manage symptoms and optimize physical function.
Assistive Devices and Mobility Aids
Assistive devices and mobility aids are essential in supporting daily activities and promoting independence for individuals with SPMS. Devices such as canes, walkers, and wheelchairs provide stability and support during mobility. Adaptive equipment, such as grab bars, raised toilet seats, and specialized utensils, help facilitate self-care tasks and improve safety in the home environment. Occupational therapists assess individual needs and recommend appropriate assistive devices to enhance functional abilities and quality of life. Education and training in device use are essential for maximizing benefits and ensuring safe and effective implementation.
Lifestyle Modifications
Diet and Nutrition
Maintaining a balanced diet and adequate nutrition is essential for overall health and well-being in SPMS. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports immune function, reduces inflammation, and promotes energy levels. Some individuals may benefit from dietary supplements, such as vitamin D and omega-3 fatty acids, which have been studied for their potential neuroprotective effects in MS. Consulting with a registered dietitian or nutritionist can help develop personalized dietary strategies to meet individual nutritional needs and support disease management.
Stress Management Techniques
Managing stress is crucial for individuals with SPMS, as stress can exacerbate symptoms and impact overall health. Techniques such as mindfulness meditation, deep breathing exercises, progressive muscle relaxation, and yoga promote relaxation and reduce stress levels. Engaging in enjoyable activities, hobbies, and social connections also contributes to emotional well-being and resilience. Identifying and minimizing sources of stress, establishing realistic goals, and practicing self-care are integral components of stress management in SPMS. Healthcare providers and support networks can provide guidance and resources to implement effective stress reduction strategies.
Stem Cell Treatments for Secondary-Progressive Multiple Sclerosis
Overview of Stem Cell Therapy
Stem cell therapy is a promising area of research and treatment for SPMS, aiming to repair damaged nerve tissue and modulate the immune response. Stem cells have the potential to differentiate into various cell types and promote tissue regeneration, offering a novel approach to disease modification. While still considered experimental, stem cell therapies hold significant promise for individuals with aggressive or refractory SPMS who have not responded adequately to conventional treatments. Ongoing clinical trials and research initiatives seek to elucidate the safety, efficacy, and long-term outcomes of stem cell therapies in MS.
Types of Stem Cells Used
Hematopoietic Stem Cells
Hematopoietic stem cells, derived from bone marrow or peripheral blood, are commonly used in stem cell transplantation for MS. These multipotent cells have the ability to differentiate into immune cells, which may reset the immune system and reduce autoimmune activity in SPMS. High-dose chemotherapy is typically administered to deplete existing immune cells before transplanting hematopoietic stem cells to promote immune system reconstitution. This approach aims to halt disease progression and induce prolonged periods of remission in select individuals with aggressive forms of SPMS.
Mesenchymal Stem Cells
Mesenchymal stem cells, found in various tissues such as bone marrow, adipose tissue, and umbilical cord blood, exhibit immunomodulatory and regenerative properties. These cells secrete factors that suppress inflammatory responses and promote tissue repair, making them attractive candidates for MS therapy. Mesenchymal stem cell transplantation has shown promising results in preclinical studies and early-phase clinical trials, suggesting potential benefits for reducing inflammation and preserving neurological function in SPMS. Further research is needed to optimize protocols, assess long-term safety, and establish efficacy in larger patient populations.
Mechanisms of Action
Stem cells exert their therapeutic effects through multiple mechanisms in SPMS. These include immunomodulation, promoting tissue repair and regeneration, and reducing neuroinflammation. Hematopoietic stem cell transplantation aims to reset the immune system and prevent further autoimmune-mediated damage to the central nervous system. Mesenchymal stem cells contribute to tissue repair by releasing growth factors, cytokines, and extracellular vesicles that modulate the local immune response and support neuronal survival. Understanding these mechanisms is essential for refining stem cell therapies and maximizing their therapeutic potential in treating SPMS.
Clinical Trials and Research Findings
Clinical trials investigating stem cell therapies for SPMS have demonstrated varying degrees of efficacy and safety. Early-phase trials have reported improvements in neurological function, reduction in disease activity, and stabilization of disability progression in some participants. However, challenges remain, including the need for standardized protocols, optimization of patient selection criteria, and long-term monitoring of outcomes. Ongoing research initiatives aim to address these challenges and expand our understanding of stem cell therapies’ role in MS treatment. Collaborative efforts among researchers, clinicians, and patients are essential for advancing this promising field.
Risks and Benefits
Stem cell therapies for SPMS carry inherent risks and benefits that require careful consideration and informed decision-making. Potential benefits may include disease stabilization, improved quality of life, and reduced reliance on conventional treatments. However, risks such as infection, immune reactions, and long-term adverse effects necessitate thorough risk assessment and patient counseling. The decision to pursue stem cell therapy should involve comprehensive discussions with healthcare providers, weighing potential benefits against risks based on individual disease characteristics and treatment goals. Continued research and clinical trials are essential for establishing safety, efficacy, and long-term outcomes of stem cell therapies in SPMS.
Coping with Secondary-Progressive Multiple Sclerosis
Psychological Support
Counseling and Therapy
Psychological support is essential for individuals coping with SPMS, addressing the emotional and psychological impact of living with a chronic neurological condition. Counseling and therapy provide a safe space to explore feelings of grief, frustration, and uncertainty, while developing coping strategies and resilience. Cognitive-behavioral therapy (CBT) helps individuals manage stress, anxiety, and depression by identifying negative thought patterns and promoting adaptive behaviors. Supportive psychotherapy emphasizes emotional expression, validation, and building a supportive network of family, friends, and healthcare providers.
Support Groups and Community Resources
Engaging in support groups and community resources offers social connection, peer support, and shared experiences for individuals with SPMS and their caregivers. These groups provide opportunities to exchange practical tips, emotional support, and encouragement while navigating the challenges of living with MS. Online forums, local MS societies, and patient advocacy organizations offer educational resources, virtual support groups, and community events that promote empowerment and resilience. Peer support networks foster a sense of belonging and solidarity, reducing feelings of isolation and promoting overall well-being.
Practical Tips for Daily Living
Energy Conservation Strategies
Managing energy levels is crucial for individuals with SPMS to optimize daily functioning and reduce fatigue. Energy conservation strategies involve pacing activities, prioritizing tasks, and incorporating rest breaks throughout the day. Simplifying routines, delegating tasks, and using assistive devices can help conserve physical and cognitive energy. Planning ahead, setting realistic goals, and practicing self-care promote efficiency and minimize exhaustion. Occupational therapists provide personalized guidance and practical strategies to enhance energy conservation and improve productivity in daily activities.
Home Modifications for Accessibility
Adapting the home environment for accessibility enhances safety, independence, and quality of life for individuals with SPMS. Modifications may include installing grab bars in bathrooms, widening doorways for wheelchair accessibility, and reducing tripping hazards. Accessible furniture, such as adjustable beds and supportive seating, promotes comfort and ease of movement. Smart home technologies, such as voice-activated devices and automated lighting, offer convenience and accessibility. Occupational therapists conduct home assessments and recommend personalized modifications to address individual needs and maximize functional independence.
Family and Caregiver Support
Education and Training for Caregivers
Family and caregivers play a crucial role in supporting individuals with SPMS, offering practical assistance, emotional encouragement, and advocacy. Education and training programs provide caregivers with essential knowledge about MS, symptom management, and caregiving strategies. Understanding the impact of SPMS on physical and cognitive function enables caregivers to anticipate needs, promote independence, and provide responsive care. Effective communication, mutual respect, and shared decision-making strengthen partnerships between individuals with SPMS and their caregivers, fostering a supportive and nurturing environment.
Respite Care Options
Respite care offers temporary relief and support for caregivers, allowing them to recharge, pursue personal interests, and maintain their own health and well-being. Respite services may include in-home care, adult day programs, or short-term residential stays tailored to individual preferences and needs. Professional caregivers provide compassionate support, supervision, and assistance with daily activities, ensuring continuity of care and peace of mind for individuals with SPMS and their families. Accessing respite care resources enhances caregiver resilience, reduces stress, and promotes sustainable caregiving practices.
Research and Future Directions in SPMS Treatment
Current Research Initiatives
Ongoing research initiatives in SPMS focus on advancing understanding, improving treatment outcomes, and exploring novel therapeutic approaches. Multidisciplinary collaborations among researchers, clinicians, and advocacy organizations drive innovation and progress in MS research. Epidemiological studies investigate disease progression patterns, risk factors, and impact on quality of life to inform personalized treatment strategies. Biomarker research aims to identify biological markers that predict disease activity, treatment response, and prognosis in SPMS. Precision medicine approaches seek to tailor therapies based on individual genetic profiles and disease characteristics, optimizing therapeutic efficacy and minimizing adverse effects.
Emerging Therapies and Innovations
Emerging therapies in SPMS explore new treatment modalities, including targeted immunotherapies, neuroprotective agents, and regenerative medicine approaches. Monoclonal antibodies targeting specific immune cells or cytokines aim to modulate immune responses and reduce inflammatory damage in the central nervous system. Neuroprotective strategies focus on preserving neuronal integrity and function, potentially slowing disease progression and improving neurological outcomes. Regenerative medicine holds promise for repairing damaged nerve tissue and promoting recovery through stem cell therapies, tissue engineering, and gene therapy techniques. Early-phase clinical trials and translational research efforts are underway to evaluate safety, efficacy, and long-term benefits of these innovative approaches in SPMS.
The Role of Genetics and Biomarkers
Genetic studies and biomarker research provide insights into the underlying mechanisms of SPMS, guiding personalized treatment decisions and prognostic assessments. Genome-wide association studies (GWAS) identify genetic variants associated with MS susceptibility, disease progression, and response to therapy. Understanding genetic factors enables clinicians to stratify risk, predict clinical outcomes, and optimize treatment approaches tailored to individual genetic profiles. Biomarkers such as neuroimaging markers, cytokine profiles, and neurofilament light chain levels offer objective measures of disease activity, treatment response, and progression in SPMS. Integrating genetic and biomarker data into clinical practice enhances precision medicine approaches and improves patient outcomes in MS management.
Patient Involvement in Research
Active patient involvement and engagement in research empower individuals with SPMS to contribute to scientific advancements, shape research priorities, and advocate for improved treatments and healthcare services. Patient-centered research initiatives prioritize patient perspectives, values, and priorities in study design, recruitment strategies, and outcome assessments. Participatory research approaches foster collaboration, trust, and transparency between researchers, healthcare providers, and individuals with SPMS, ensuring research relevance and meaningful impact on patient care. Patient advocacy organizations play a vital role in amplifying patient voices, raising awareness, and mobilizing support for research funding and policy initiatives.
Future Challenges and Opportunities
Despite significant progress in SPMS research and treatment, several challenges and opportunities lie ahead in addressing unmet needs and improving patient outcomes. Challenges include optimizing early detection and diagnosis of SPMS, enhancing access to specialized care and multidisciplinary services, and addressing disparities in healthcare delivery. Long-term monitoring of treatment efficacy, safety, and adherence remains essential to manage disease progression and minimize complications. Innovations in telemedicine, digital health technologies, and remote monitoring offer opportunities to expand access to healthcare services, enhance patient engagement, and improve continuity of care for individuals with SPMS. Collaborative efforts across stakeholders, continued investment in research, and advocacy for policies that support MS research and healthcare delivery are critical to advancing treatment options and improving quality of life for individuals living with SPMS.
FAQs
What are the early signs of secondary-progressive multiple sclerosis (SPMS)?
Early signs of SPMS may include worsening neurological symptoms, increased disability progression, and reduced recovery periods between relapses. Symptoms such as persistent fatigue, difficulty walking, cognitive impairment, and sensory changes may indicate transition from relapsing-remitting MS to SPMS.
How is secondary-progressive multiple sclerosis (SPMS) diagnosed?
Diagnosis of SPMS involves clinical evaluation, neuroimaging with MRI, and assessment of disease progression over time. Neurological examination, including assessment of motor, sensory, cognitive, and emotional function, helps differentiate SPMS from other MS types and neurological conditions.
What treatments are available for secondary-progressive multiple sclerosis (SPMS)?
Treatments for SPMS include disease-modifying therapies (DMTs) to reduce disease activity and progression, symptomatic treatments for managing symptoms such as spasticity and pain, physical and occupational therapy to optimize function and mobility, and emerging therapies such as stem cell transplantation and targeted immunotherapies.
How can individuals with secondary-progressive multiple sclerosis (SPMS) manage daily challenges and improve quality of life?
Managing SPMS involves adopting lifestyle modifications, such as maintaining a balanced diet, managing stress, and conserving energy. Engaging in physical and occupational therapy, accessing assistive devices, and participating in support groups provide practical support and emotional resilience to navigate daily challenges and enhance quality of life.