Skin ulcers are more than just surface wounds—they’re often signs of deeper health issues such as poor circulation, diabetes, or prolonged immobility. This article explores the different types of skin ulcers—venous, arterial, diabetic, and pressure-related—along with their root causes, early warning signs, and complications. You’ll discover how timely diagnosis, effective wound care, and modern treatments like PRP, stem cells, and exosome therapy can support faster healing and prevent recurrence. Whether you’re managing a chronic ulcer or looking to understand risk factors, this guide offers expert insight and practical solutions for long-term skin health.
Introduction to Skin Ulcers
What Are Skin Ulcers?
Skin ulcers are open wounds that refuse to heal on their own within the expected time frame—usually a few weeks. These persistent sores develop when blood flow to an area is disrupted, leading to tissue breakdown. While ulcers can appear almost anywhere on the body, they’re most commonly seen on the legs, feet, buttocks, and lower back—especially in individuals with limited mobility or underlying health issues.
These aren’t just superficial skin issues; they’re often signals that something deeper in the body, like the vascular or immune system, isn’t functioning as it should.
Why They Shouldn’t Be Ignored
Skin ulcers are far more than just painful lesions. If neglected, they can lead to serious complications, including deep tissue infections, bone exposure, and even amputation in severe cases. Beyond the physical toll, they can drastically affect a person’s quality of life—disrupting sleep, mobility, and emotional well-being.
More importantly, ulcers often point to chronic systemic conditions such as diabetes or poor circulation that need urgent attention. Treating the ulcer alone isn’t enough—you need to address the root cause to truly heal.
Main Types of Skin Ulcers
Skin ulcers aren’t one-size-fits-all. Understanding the type of ulcer you’re dealing with is essential for effective treatment and long-term healing. Each type has unique causes, characteristics, and care needs.
Venous Ulcers
Venous ulcers are the most common type of leg ulcers. They typically form around the ankles when veins fail to return blood efficiently to the heart—a condition known as venous insufficiency. The excess pressure causes blood to pool in the lower legs, leading to swelling, skin damage, and eventually open sores.
These ulcers are often shallow but painful, with irregular borders and oozing fluid. Without proper compression therapy and care, they can recur frequently.
Arterial Ulcers
Unlike venous ulcers, arterial ulcers occur when there’s insufficient blood flow through the arteries. They typically develop on the feet, heels, or toes, where circulation is weakest. The sores have a punched-out appearance, tend to be dry, and are often extremely painful—especially at night or when legs are elevated.
Arterial ulcers are a red flag for peripheral artery disease (PAD) and should be evaluated promptly. Revascularization or improved blood flow is usually necessary before these wounds can heal.
Diabetic (Neuropathic) Ulcers
People with diabetes are at high risk for neuropathic ulcers due to two factors: nerve damage (neuropathy) and poor circulation. Neuropathy makes it difficult to feel pressure points or minor injuries on the feet, which can quickly evolve into serious ulcers without the person even realizing it.
These ulcers typically form on the soles of the feet or under pressure points, and often go unnoticed until infection sets in. Strict blood sugar control, daily foot checks, and protective footwear are critical for prevention and management.
Pressure Ulcers (Bedsores)
Pressure ulcers, or bedsores, develop when the skin is constantly compressed against a surface, cutting off blood supply. This is common in elderly, paralyzed, or bedridden patients, especially over bony areas like the hips, tailbone, and heels.
Early stages may appear as red or discolored skin, but without intervention, they can progress to deep wounds involving muscle and bone. Regular repositioning, pressure-relieving devices, and attentive nursing care are vital in preventing these life-threatening ulcers.
Root Causes of Skin Ulcers
Understanding the underlying causes of skin ulcers is crucial—not just for healing, but for preventing them from returning. Many ulcers are symptoms of deeper health conditions rather than isolated skin issues.
Poor Circulation
When blood doesn’t flow properly—especially in the legs and feet—it starves tissues of oxygen and nutrients. Over time, this weakens the skin and underlying tissue, making them more vulnerable to breakdown. Conditions like chronic venous insufficiency or peripheral artery disease (PAD) are major culprits. Without circulation, even minor scrapes can escalate into full-blown ulcers.
Diabetes and Neuropathy
Diabetes does double damage. High blood sugar levels impair both nerve function and blood vessels, especially in the lower limbs. Neuropathy dulls pain sensitivity, so a person might not even notice an injury. Meanwhile, reduced circulation means the body can’t heal the wound efficiently. That’s why diabetic foot ulcers are among the most serious—and common—types of chronic wounds.
Prolonged Pressure or Immobility
When someone is bedridden or has limited mobility, sustained pressure on one area of the body compresses blood vessels and deprives tissue of oxygen. Over time, this leads to pressure ulcers. Individuals with spinal cord injuries, elderly patients, and those in long-term care facilities are at especially high risk.
Infections and Autoimmune Diseases
Persistent infections can damage tissue and block the healing process, especially in immune-compromised individuals. Bacterial or fungal infections, if not treated early, can worsen ulcers or even cause them to develop.
Lupus and Vasculitis as Triggers
Autoimmune conditions such as lupus and vasculitis create internal inflammation that can damage blood vessels. When this happens, blood supply to the skin becomes compromised, leading to spontaneous ulcers—often on the legs or ankles. These ulcers can be particularly stubborn and may require systemic treatment beyond typical wound care.
Ready to Explore Stem Cell Therapy?
Book a personalized consultation with our medical experts today.
Symptoms and Early Signs
Catching a skin ulcer early can make all the difference in how quickly and effectively it heals. Unfortunately, many ulcers start subtly and worsen before they get proper attention.
Pain, Discoloration, and Swelling
One of the first signs of a developing ulcer is localized pain or discomfort, often accompanied by redness, swelling, or skin discoloration. The area may feel warm to the touch and appear shiny or tight. In some cases, especially with diabetic ulcers, pain may be minimal or absent due to nerve damage—even if the ulcer is already advanced.
Signs of Infection to Watch For
Infection is a serious complication and should never be overlooked. Watch for symptoms such as:
-
Pus or foul-smelling discharge
-
Increased redness or warmth around the wound
-
Fever or chills
-
Sudden increase in pain
-
Red streaks radiating from the ulcer
If any of these signs appear, it’s important to seek medical care immediately. Infections can spread rapidly, especially in those with weakened immune systems.
How Ulcers Change Over Time
Untreated ulcers worsen in both depth and severity. What starts as a small break in the skin can deepen to expose underlying fat, muscle, or even bone. Chronic ulcers may develop thickened edges, dark necrotic tissue, or slough (dead material) that hinders healing.
Without intervention, ulcers can become a gateway to serious infections like cellulitis or sepsis. In diabetic patients, this progression can lead to limb-threatening complications and amputation.
Diagnosis and Medical Evaluation
Accurate diagnosis is the first step toward effective healing. Treating a skin ulcer without understanding its cause is like putting a bandage on a warning light—it might cover the problem temporarily, but the danger remains.
Clinical Examination and History
A comprehensive physical examination is essential. Your healthcare provider will:
-
Inspect the ulcer’s location, size, depth, and appearance
-
Check for signs of infection or tissue necrosis
-
Evaluate the surrounding skin and nearby blood vessels
-
Ask about medical history, including conditions like diabetes, vascular disease, immobility, or autoimmune disorders
They’ll also want to know how long the ulcer has been present, whether it has changed recently, and what treatments (if any) have been attempted.
Imaging and Laboratory Tests
To gain deeper insight and rule out complications, your provider may order:
-
Doppler Ultrasound – to assess blood flow and identify arterial or venous insufficiency
-
X-rays or MRI – to detect bone involvement or hidden infections such as osteomyelitis
-
Blood tests – to check for infection, inflammation, or underlying systemic disease
-
Wound culture – to identify specific bacteria or fungi responsible for any infection
These tests help create a personalized treatment plan that targets not just the ulcer, but its underlying cause.
Questions About Skin Ulcer Treatments?
Connect with our team to learn how stem cells can help your condition.
Effective Treatment Options for Skin Ulcers
Healing a skin ulcer takes more than just a surface solution. It requires a combination of wound care, infection control, and attention to the underlying cause. With the right approach, even chronic ulcers can begin to recover.
Wound Cleaning and Debridement
The first step in treating any ulcer is keeping it clean and free of dead tissue. This helps prevent infection and stimulates the body’s natural healing response.
-
Cleansing is typically done with saline or antiseptic solutions.
-
Debridement involves removing dead or infected tissue using surgical tools, enzymes, or dressings designed to soften and lift damaged areas.
Debridement is crucial—it jumpstarts the healing process and creates a healthy environment for new tissue to grow.
Topical and Oral Medications
Medication plays a vital role in managing infections and promoting healing:
-
Topical antibiotics or antimicrobial dressings (like silver or iodine-based products) help control local infection.
-
Oral antibiotics are often prescribed when there’s evidence of spreading infection or systemic involvement.
-
Anti-inflammatory creams may be used for ulcers linked to autoimmune conditions.
Moist wound healing is a key principle, so advanced dressings are often used to maintain the right balance—not too wet, not too dry.
Advanced Care Techniques
When standard care isn’t enough, modern wound management offers next-level options.
Negative Pressure Wound Therapy (NPWT)
Also known as vacuum-assisted closure (VAC), this technique uses a sealed dressing connected to a suction pump. It helps:
-
Remove excess fluid
-
Improve circulation
-
Promote faster tissue growth
NPWT is especially effective for deep, chronic, or post-surgical ulcers.
Skin Grafting and Biological Dressings
For large or non-healing wounds, skin grafts (from the patient or a donor) can be applied to encourage healing. Newer options like bioengineered skin substitutes mimic the properties of natural tissue and support regeneration.
These advanced therapies are typically performed in specialized wound care centers under medical supervision.
Regenerative and Alternative Therapies
Modern science is pushing the boundaries of how we treat skin ulcers. Regenerative therapies go beyond traditional care by stimulating the body’s natural healing abilities at a cellular level. These options are particularly promising for chronic, hard-to-heal, or diabetic ulcers.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy uses the patient’s own blood to accelerate healing:
-
A small blood sample is drawn.
-
The platelets—rich in growth factors—are separated and concentrated.
-
The PRP is injected around or applied directly to the ulcer.
These growth factors promote cell repair, angiogenesis (new blood vessel formation), and collagen production, creating an optimal environment for healing. PRP has shown encouraging results in non-healing diabetic foot ulcers and post-surgical wound care.
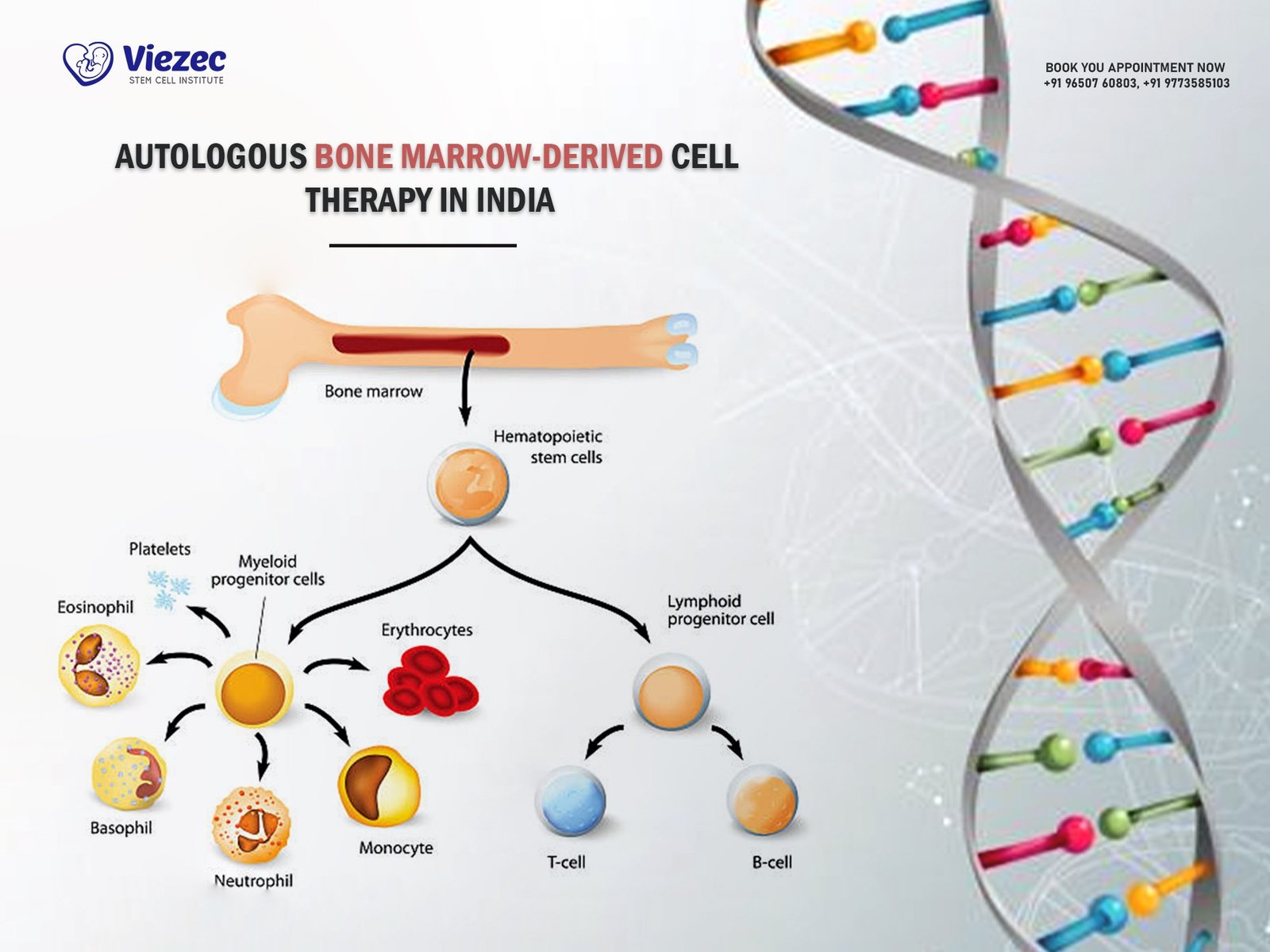
Stem Cell-Based Treatments
Stem cells are the master cells of the body—capable of transforming into various tissue types and secreting healing signals. In ulcer treatment, mesenchymal stem cells (MSCs) derived from bone marrow or fat tissue are used for their anti-inflammatory, pro-healing properties.
Benefits of stem cell therapy include:
-
Tissue regeneration
-
Improved blood flow
-
Reduced inflammation
-
Faster closure of chronic wounds
Stem cells can be injected near the wound or applied using scaffolds or dressings. Studies have shown that MSCs are especially effective in diabetic foot ulcers, where traditional therapies often fail.
Exosome Therapy
Exosomes are tiny extracellular vesicles secreted by stem cells. Think of them as molecular messengers that carry proteins, RNAs, and growth factors critical for tissue repair.
Exosome therapy works by:
-
Enhancing cellular communication
-
Reducing inflammation
-
Stimulating angiogenesis and fibroblast activity
-
Accelerating re-epithelialization (skin regeneration)
Unlike stem cells, exosomes do not replicate, making them safer and easier to store and transport. Their small size also allows them to penetrate tissues more efficiently, making them ideal for topical use or microinjections in chronic ulcers.
This approach is gaining ground in clinical research and may soon become a mainstream option for non-healing wounds, especially in patients with vascular or autoimmune challenges.
Discover Regenerative Healing with Stem Cells
Take the first step toward recovery with expert care tailored for you.
Prevention and Home Care
When it comes to skin ulcers, prevention is always better than cure. For people at risk—such as those with diabetes, poor circulation, or limited mobility—daily habits and proactive care can dramatically reduce the chances of ulcers forming or recurring.
Daily Skincare and Hygiene Tips
Healthy skin starts with consistent care:
-
Clean affected areas gently using mild soap and lukewarm water.
-
Avoid scrubbing or over-drying the skin, which can cause microtears.
-
Apply fragrance-free moisturizers to keep the skin supple and hydrated.
-
Check daily for cracks, redness, or signs of pressure, especially around ankles, heels, and toes.
Even minor cuts or abrasions should be treated immediately to prevent them from evolving into ulcers.
Mobility Exercises and Pressure Relief
For those with limited mobility or at risk of pressure ulcers:
-
Change positions every 1–2 hours if lying down, and every 15–30 minutes if seated.
-
Use pressure-relieving cushions or mattresses to reduce skin stress points.
-
Incorporate gentle stretching or range-of-motion exercises to improve blood flow.
-
Consider consulting a physical therapist for a customized mobility plan.
Maintaining circulation and reducing pressure are key to protecting the skin’s integrity.
Managing Chronic Conditions to Prevent Recurrence
Most skin ulcers are symptoms of deeper medical issues. To prevent recurrence:
-
Keep blood sugar levels in check if you have diabetes.
-
Manage blood pressure and cholesterol to support vascular health.
-
Follow medical advice for autoimmune conditions like lupus or vasculitis.
-
Stay hydrated and maintain a balanced, nutrient-rich diet to support skin and immune health.
When ulcers do heal, continue monitoring the area for signs of breakdown and stay on top of follow-up care. Healing isn’t the end—it’s the beginning of ongoing prevention.
Living With Chronic Ulcers
For many individuals, skin ulcers are not just a temporary condition—they’re an ongoing challenge that affects both physical health and emotional well-being. But with the right mindset, support system, and medical strategy, it’s possible to reclaim comfort, confidence, and control.
Coping Emotionally and Physically
Living with a chronic ulcer can take a toll on every aspect of life:
-
Physical discomfort may limit movement, sleep, and independence.
-
Frequent dressing changes and medical visits can feel exhausting.
-
Emotional effects like anxiety, frustration, or depression are common—especially when healing is slow.
It’s important to acknowledge these struggles and seek support. Counseling, support groups, or talking to a mental health professional can make a meaningful difference. Don’t underestimate the power of community—connecting with others facing similar challenges can help ease the burden.
Also, celebrate progress—no matter how small. Healing happens in phases, and every improvement is a step forward.
When to Consult a Wound Specialist
If you’re dealing with a wound that:
-
Hasn’t improved in two weeks
-
Shows signs of infection
-
Keeps recurring
-
Involves underlying conditions like diabetes or vascular disease
—it’s time to see a wound care specialist.
These experts can offer advanced diagnostics, tailored treatment plans, and access to cutting-edge therapies like stem cell applications, PRP, or bioengineered skin. In some cases, collaboration with endocrinologists, vascular surgeons, or rheumatologists may be necessary for comprehensive care.
Remember: chronic ulcers are complex, but they’re not unbeatable. With persistence, expert care, and emerging regenerative options, healing is more achievable than ever before.