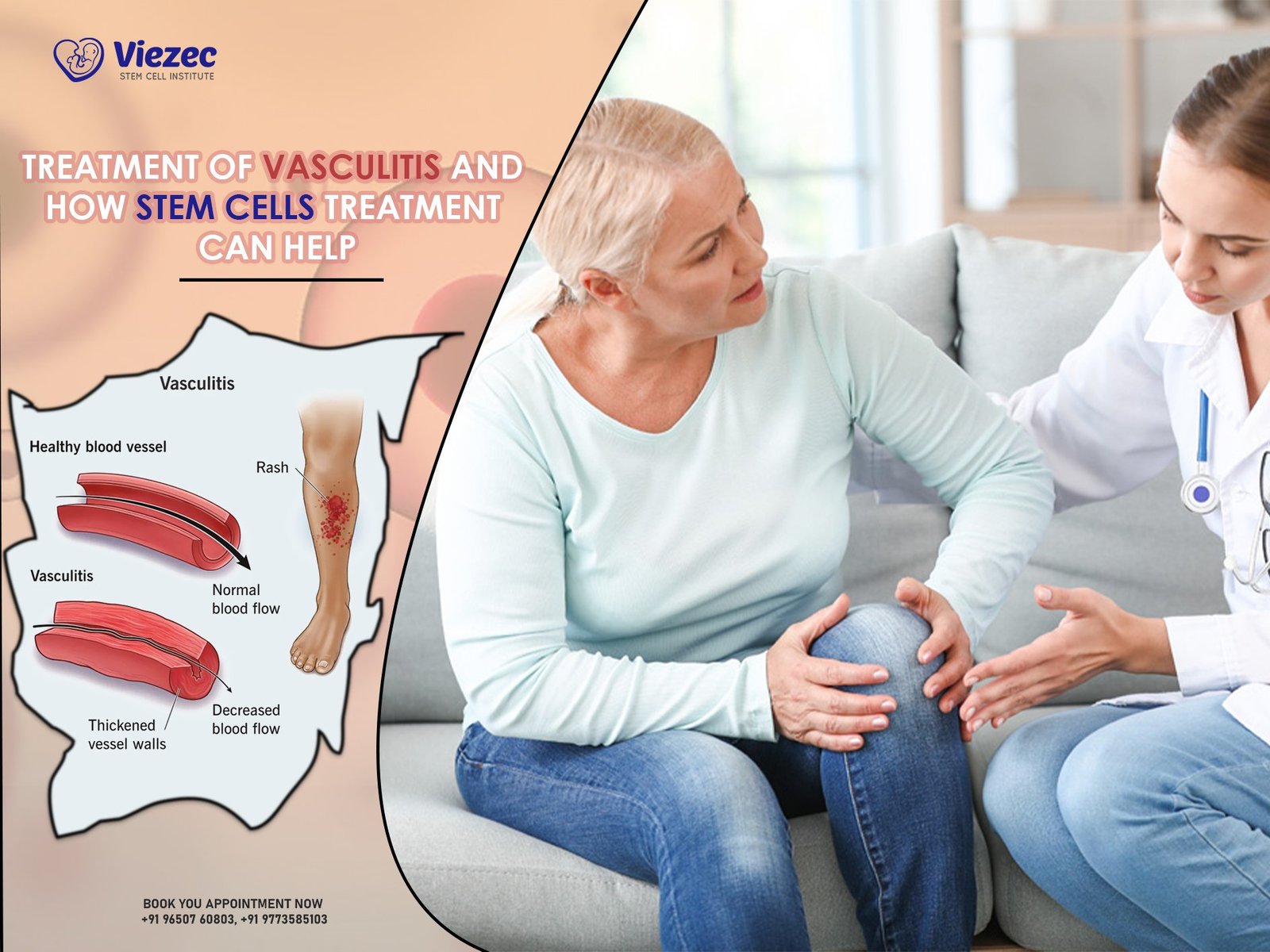
Vasculitis is a group of disorders characterized by inflammation of blood vessels, leading to various clinical manifestations. This condition can affect blood vessels of any size, type, or location within the body, including arteries, veins, and capillaries. The inflammatory process in vasculitis can result in tissue damage, organ dysfunction, and potentially life-threatening complications. While the exact cause of vasculitis remains unclear in many cases, it is believed to involve a dysregulated immune response, genetic predisposition, and environmental factors.
Overview of Vasculitis
Vasculitis encompasses a diverse array of diseases, each with its own distinct clinical features, underlying mechanisms, and prognostic implications. These disorders can be classified based on the size of the affected blood vessels (small, medium, or large) and the specific organs involved. Common types of vasculitis include:
Types of Vasculitis
- Small Vessel Vasculitis: Examples include granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
- Medium Vessel Vasculitis: Conditions like polyarteritis nodosa (PAN) and Kawasaki disease fall into this category.
- Large Vessel Vasculitis: Giant cell arteritis (GCA) and Takayasu arteritis are prominent examples of large vessel vasculitis.
Causes and Symptoms
The etiology of vasculitis is multifactorial, involving complex interactions between genetic susceptibility, environmental triggers, and dysregulated immune responses. While the precise triggers may vary depending on the subtype of vasculitis, common factors implicated in its pathogenesis include infections, autoimmune phenomena, drug reactions, and environmental toxins.
Clinical manifestations of vasculitis can vary widely depending on the size and location of the affected blood vessels and the organs involved. However, common symptoms may include:
- Fatigue
- Fever
- Weight loss
- Skin rashes or ulcers
- Joint pain or swelling
- Nerve pain or numbness
- Shortness of breath
- Visual disturbances
Conventional Treatments for Vasculitis
The management of vasculitis typically involves a combination of pharmacotherapy, lifestyle modifications, and supportive care aimed at controlling inflammation, preserving organ function, and preventing disease complications. Commonly used treatments include:
Corticosteroids and Immunosuppressive Drugs
Corticosteroids, such as prednisone, are often used as first-line agents to suppress inflammation and modulate the immune response in vasculitis. In more severe cases or when corticosteroids alone are insufficient, additional immunosuppressive medications, such as methotrexate, azathioprine, or cyclophosphamide, may be prescribed to achieve disease remission.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are commonly used to alleviate pain, reduce fever, and relieve inflammation in vasculitis. While they may provide symptomatic relief, NSAIDs do not address the underlying immune-mediated pathology of the disease and are typically used in conjunction with other therapies.
Biologic Therapies
Biologic agents, such as rituximab and tocilizumab, target specific components of the immune system involved in the pathogenesis of vasculitis. These medications may be used in refractory cases or as adjunctive therapy to conventional immunosuppressants, offering a more targeted and tailored approach to treatment.
Limitations of Conventional Treatments
Despite the efficacy of conventional treatments in many cases, they are associated with several limitations and challenges, including:
- Side Effects and Long-term Risks: Prolonged use of corticosteroids and immunosuppressive drugs can lead to significant adverse effects, such as osteoporosis, diabetes, hypertension, and increased susceptibility to infections.
- Inefficacy in Some Cases: Not all patients with vasculitis respond adequately to conventional therapies, leading to persistent disease activity, relapses, and progressive organ damage.
- Relapse Rates: Even among responders, vasculitis often follows a relapsing-remitting course, with periods of disease quiescence alternating with flare-ups, necessitating ongoing monitoring and adjustments to treatment regimens.
Emerging Role of Stem Cell Therapy
In recent years, stem cell therapy has emerged as a promising and innovative approach for the treatment of vasculitis, offering the potential for disease modification, tissue repair, and long-term remission. Stem cells possess unique regenerative and immunomodulatory properties that make them attractive candidates for therapeutic intervention in autoimmune and inflammatory disorders.
Understanding Stem Cell Therapy
Stem cell therapy involves the administration of exogenous stem cells, either from the patient’s own body (autologous) or from a donor (allogeneic), to modulate immune responses, promote tissue repair, and restore homeostasis. These cells can differentiate into various cell types and exert paracrine effects through the release of bioactive factors, thereby exerting pleiotropic effects on the immune system and the microenvironment of inflamed tissues.
Mechanisms of Action in Vasculitis Treatment
The therapeutic effects of stem cell therapy in vasculitis are mediated through multiple mechanisms, including:
- Immune Modulation and Regulation: Stem cells have the ability to suppress aberrant immune responses, inhibit pro-inflammatory cytokine production, and promote the expansion of regulatory T cells, thereby restoring immune tolerance and attenuating autoimmunity.
- Tissue Repair and Regeneration: Stem cells possess regenerative potential and can differentiate into endothelial cells, smooth muscle cells, and other cell types involved in vascular repair and angiogenesis, promoting tissue healing and functional recovery.
- Reduced Relapse Rates: By targeting the underlying pathophysiology of vasculitis and inducing durable immunomodulatory effects, stem cell therapy may reduce the frequency and severity of disease flares, leading to sustained remission and improved long-term outcomes.
Clinical Trials and Research Findings
A growing body of preclinical and clinical evidence supports the efficacy and safety of stem cell therapy in the treatment of vasculitis. Several small-scale studies and pilot trials have demonstrated promising results, with improvements in disease activity scores, reduction in relapse rates, and enhanced quality of life observed in treated patients.
Types of Stem Cells Used in Vasculitis Treatment
Stem cells used in vasculitis treatment can be derived from various sources, each with its own unique characteristics and therapeutic potential. Common types of stem cells utilized in clinical practice include:
Hematopoietic Stem Cells
Hematopoietic stem cells are multipotent progenitor cells found in bone marrow, peripheral blood, and umbilical cord blood, capable of differentiating into various blood cell lineages, including leukocytes, erythrocytes, and platelets. Autologous hematopoietic stem cell transplantation (HSCT) has been investigated as a treatment strategy for severe refractory vasculitis, offering the potential for immune system reset and long-term disease control.
Mesenchymal Stem Cells
Mesenchymal stem cells are adult stem cells present in various tissues, such as bone marrow, adipose tissue, and umbilical cord tissue, with immunomodulatory, anti-inflammatory, and regenerative properties. These cells have been shown to suppress immune activation, promote tissue repair, and modulate the inflammatory microenvironment in vasculitis, offering a novel therapeutic approach for disease management.
Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPSCs) are generated by reprogramming adult somatic cells, such as skin fibroblasts or blood cells, into a pluripotent state, resembling embryonic stem cells. iPSC technology holds great promise for personalized medicine and disease modeling in vasculitis, allowing for the generation of patient-specific stem cell lines for drug screening, genetic analysis, and regenerative medicine applications.
Advantages of Stem Cell Therapy in Vasculitis
Stem cell therapy offers several potential advantages over conventional treatments for vasculitis, including:
- Immune Modulation and Regulation: Stem cells exert broad immunomodulatory effects, targeting multiple components of the immune system involved in the pathogenesis of vasculitis, leading to durable disease control and reduced reliance on immunosuppressive medications.
- Tissue Repair and Regeneration: Stem cells promote endothelial repair, neovascularization, and tissue remodeling in damaged blood vessels, restoring vascular integrity and function and preventing long-term complications, such as stenosis, aneurysm formation, and organ dysfunction.
- Reduced Relapse Rates: By inducing immune tolerance and promoting tissue healing, stem cell therapy may reduce the frequency and severity of disease flares, leading to prolonged remission and improved quality of life for patients with vasculitis.
Challenges and Considerations in Stem Cell Treatment
Despite the promising potential of stem cell therapy in vasculitis, several challenges and considerations must be addressed to ensure its safety, efficacy, and feasibility in clinical practice. Key issues include:
Safety Concerns
Stem cell therapy carries inherent risks, including infection, bleeding, thrombosis, and immune-mediated complications, such as graft-versus-host disease (GVHD) or autoimmune reactions. Rigorous patient selection, careful monitoring, and adherence to established protocols are essential to minimize adverse events and optimize treatment outcomes.
Ethical Considerations
The use of stem cells, especially embryonic stem cells, raises ethical concerns related to the source of cells, informed consent, and the potential for exploitation or misuse of biological materials. Transparent communication, ethical oversight, and adherence to regulatory guidelines are essential to uphold the principles of autonomy, beneficence, and justice in stem cell research and therapy.
Cost and Accessibility
Stem cell therapy may be associated with high upfront costs, including cell processing, transplantation procedures, and post-transplant care, making it prohibitively expensive for some patients and healthcare systems. Efforts to reduce costs, improve efficiency, and expand access to stem cell treatments through insurance coverage, reimbursement policies, and government funding are needed to ensure equitable access for all patients in need.
Patient Selection and Pre-Treatment Evaluation
The selection of appropriate candidates for stem cell therapy in vasculitis requires comprehensive pre-treatment evaluation, including:
- Disease Severity Assessment: Patients with severe, refractory, or relapsing vasculitis who have failed conventional therapies may be considered for stem cell transplantation as salvage therapy or disease-modifying intervention.
- Comorbidities Evaluation: The presence of comorbid medical conditions, such as cardiovascular disease, pulmonary dysfunction, or renal impairment, should be carefully assessed to mitigate perioperative risks and optimize treatment outcomes.
- Informed Consent Process: Patients should be fully informed about the potential risks, benefits, and uncertainties associated with stem cell therapy, allowing them to make informed decisions and participate in shared decision-making regarding their treatment options.
Stem Cell Treatment Procedure for Vasculitis
The stem cell treatment procedure for vasculitis typically involves the following steps:
Harvesting of Stem Cells
Stem cells can be harvested from various sources, including bone marrow, peripheral blood, adipose tissue, or umbilical cord blood, depending on the specific protocol and patient characteristics. The harvesting process may involve apheresis, bone marrow aspiration, or surgical extraction under local or general anesthesia.
Conditioning Regimen
Prior to stem cell transplantation, patients may undergo a conditioning regimen consisting of chemotherapy, radiation therapy, or immunosuppressive medications to deplete endogenous immune cells, suppress residual disease activity, and create a favorable environment for stem cell engraftment and differentiation.
Stem Cell Infusion and Follow-up
Once the conditioning phase is completed, harvested stem cells are infused into the patient’s bloodstream via intravenous injection, where they home to sites of inflammation, interact with host tissues, and exert their therapeutic effects. Patients are closely monitored during the post-transplant period for signs of engraftment, immune reconstitution, and disease response, with regular follow-up visits scheduled to assess treatment outcomes and adjust management strategies as needed.
Clinical Outcomes and Success Rates
The clinical outcomes and success rates of stem cell therapy in vasculitis vary depending on multiple factors, including the underlying disease subtype, patient demographics, disease severity, treatment protocol, and follow-up duration. While results from clinical trials and observational studies have shown promising efficacy and safety profiles, further research is needed to elucidate the long-term benefits and optimal strategies for patient selection, treatment delivery, and outcome assessment.
Improvement in Disease Activity Scores
Stem cell therapy has been associated with significant improvements in disease activity scores, including reductions in vasculitis disease activity index (BVAS), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) levels, and other inflammatory markers, indicative of disease remission and immunomodulatory effects.
Reduction in Relapse Rates
Patients treated with stem cell therapy have demonstrated reduced rates of disease relapse, flare-ups, and hospitalizations compared to those receiving conventional treatments alone, suggesting a potential disease-modifying effect and long-term remission induction.
Quality of Life Measures
Quality of life measures, including physical functioning, pain scores, fatigue levels, and emotional well-being, have shown significant improvements following stem cell transplantation, reflecting the holistic impact of treatment on patient-reported outcomes and health-related quality of life.
Personalized Medicine Approaches
Advances in genomic medicine, biomarker discovery, and molecular profiling may enable the development of personalized treatment algorithms and targeted therapies tailored to the individual characteristics and underlying pathophysiology of each patient with vasculitis, optimizing treatment outcomes and minimizing adverse events.
Combination Therapies
Combining stem cell therapy with conventional immunosuppressive agents, biologic therapies, or targeted inhibitors may enhance treatment efficacy, reduce treatment resistance, and prolong disease remission in vasculitis, offering synergistic effects and complementary mechanisms of action.
Biomarker Development
Identification of novel biomarkers, such as genetic polymorphisms, cytokine profiles, or immune cell subsets, may facilitate early diagnosis, prognostic stratification, and treatment response prediction in vasculitis, enabling more precise patient selection, treatment monitoring, and outcome assessment in clinical practice.
Make an informed Decision
In summary, vasculitis represents a heterogeneous group of inflammatory disorders characterized by blood vessel inflammation, tissue damage, and systemic manifestations. While conventional treatments have improved outcomes for many patients, they are associated with significant limitations, including side effects, relapses, and treatment resistance.
Stem cell therapy offers a promising alternative for patients with severe, refractory, or relapsing vasculitis, harnessing the regenerative and immunomodulatory properties of stem cells to restore immune homeostasis, promote tissue repair, and induce long-term remission. Despite challenges and considerations, ongoing research and clinical trials continue to expand our understanding of stem cell therapy and its potential applications in vasculitis, highlighting the importance of continued collaboration, innovation, and investment in regenerative medicine.
In conclusion, the future of vasculitis treatment holds great promise, with stem cell therapy poised to play a transformative role in improving patient outcomes, enhancing quality of life, and advancing the field of precision medicine for autoimmune and inflammatory diseases.
Recap of Vasculitis and Treatment Challenges
Vasculitis is a complex and heterogeneous group of disorders characterized by inflammation of blood vessels, leading to tissue damage, organ dysfunction, and systemic symptoms. Despite advances in diagnosis and treatment, vasculitis remains a challenging condition to manage, with significant morbidity and mortality associated with severe, refractory, or relapsing disease.
Conventional treatments, including corticosteroids, immunosuppressive drugs, and biologic therapies, have improved outcomes for many patients; however, they are associated with several limitations, including side effects, relapses, and treatment resistance. As such, there is a critical need for novel therapeutic approaches that address the underlying pathophysiology of vasculitis and offer durable disease control and improved quality of life for affected individuals.
Potential of Stem Cell Therapy
Stem cell therapy holds great promise as a novel and innovative treatment modality for vasculitis, offering the potential for disease modification, tissue repair, and long-term remission. By harnessing the regenerative and immunomodulatory properties of stem cells, this approach aims to restore immune homeostasis, promote vascular repair, and induce durable remission in patients with refractory or relapsing disease.
Importance of Continued Research and Development
Continued research and development are essential to advance the field of stem cell therapy in vasculitis and address current limitations and challenges. Key areas of focus include optimizing treatment protocols, refining patient selection criteria, elucidating mechanisms of action, and conducting large-scale clinical trials to establish safety, efficacy, and long-term outcomes.
By fostering collaboration, innovation, and investment in regenerative medicine, we can unlock the full potential of stem cell therapy and revolutionize the management of vasculitis, ultimately improving patient outcomes, enhancing quality of life, and paving the way for personalized and precision medicine approaches in autoimmune and inflammatory diseases.