Bone cancer is a rare but potentially devastating disease that affects the skeletal system. It originates in the bones and can spread to other parts of the body if left untreated. Traditional treatments for bone cancer include surgery, chemotherapy, and radiation therapy. However, in cases where the cancer has metastasized or is resistant to conventional treatments, bone marrow transplants offer a promising alternative.
Understanding Bone Cancer
Bone cancer, medically known as primary bone cancer, begins when normal cells in the bone undergo a series of genetic mutations, causing them to grow uncontrollably. These abnormal cells form a mass of tissue called a tumor, which can weaken the bone and lead to pain, fractures, and other complications.
There are several types of primary bone cancer, including osteosarcoma, chondrosarcoma, and Ewing sarcoma. Each type has its own distinct characteristics and requires tailored treatment approaches.
Bone Marrow Transplantation: An Overview
Bone marrow transplantation, also known as hematopoietic stem cell transplantation (HSCT), involves the replacement of diseased or damaged bone marrow with healthy stem cells. These stem cells can be obtained from a donor (allogeneic transplant) or from the patient themselves (autologous transplant).
Types of Bone Marrow Transplants
- Autologous Transplant: In an autologous transplant, the patient’s own stem cells are harvested prior to undergoing high-dose chemotherapy or radiation therapy. After the treatment, the harvested stem cells are reinfused into the patient’s bloodstream, where they migrate to the bone marrow and begin producing healthy blood cells.
- Allogeneic Transplant: An allogeneic transplant involves the use of stem cells from a genetically matched donor, typically a sibling or unrelated donor. Before the transplant, the patient undergoes conditioning therapy to suppress their immune system and make room for the donor cells. The donor cells are then infused into the patient’s bloodstream, where they engraft in the bone marrow and begin producing healthy blood cells.
Mechanism of Action
Bone marrow transplantation works by replenishing the patient’s bone marrow with healthy stem cells, which can differentiate into various blood cell types, including red blood cells, white blood cells, and platelets. This process helps restore the patient’s immune system and ability to produce healthy blood cells, which may have been compromised by cancer treatments.
Role of Bone Marrow Transplants in Bone Cancer Treatment
Addressing Treatment Resistance
One of the main challenges in treating bone cancer is the development of resistance to conventional therapies such as chemotherapy and radiation. Cancer cells can acquire mutations that render them less responsive to treatment, leading to disease progression and poor outcomes. In such cases, bone marrow transplantation offers a novel approach by providing a new source of healthy stem cells that are not affected by the resistance mechanisms.
Targeting Metastatic Disease
Metastasis, the spread of cancer from its primary site to other parts of the body, is a common feature of advanced bone cancer. Traditional treatments may be ineffective against metastatic disease, as the cancer cells have already infiltrated distant organs and tissues. By replacing the patient’s bone marrow with healthy donor cells, bone marrow transplantation can potentially target and eliminate metastatic cancer cells circulating in the bloodstream, leading to improved disease control and survival rates.
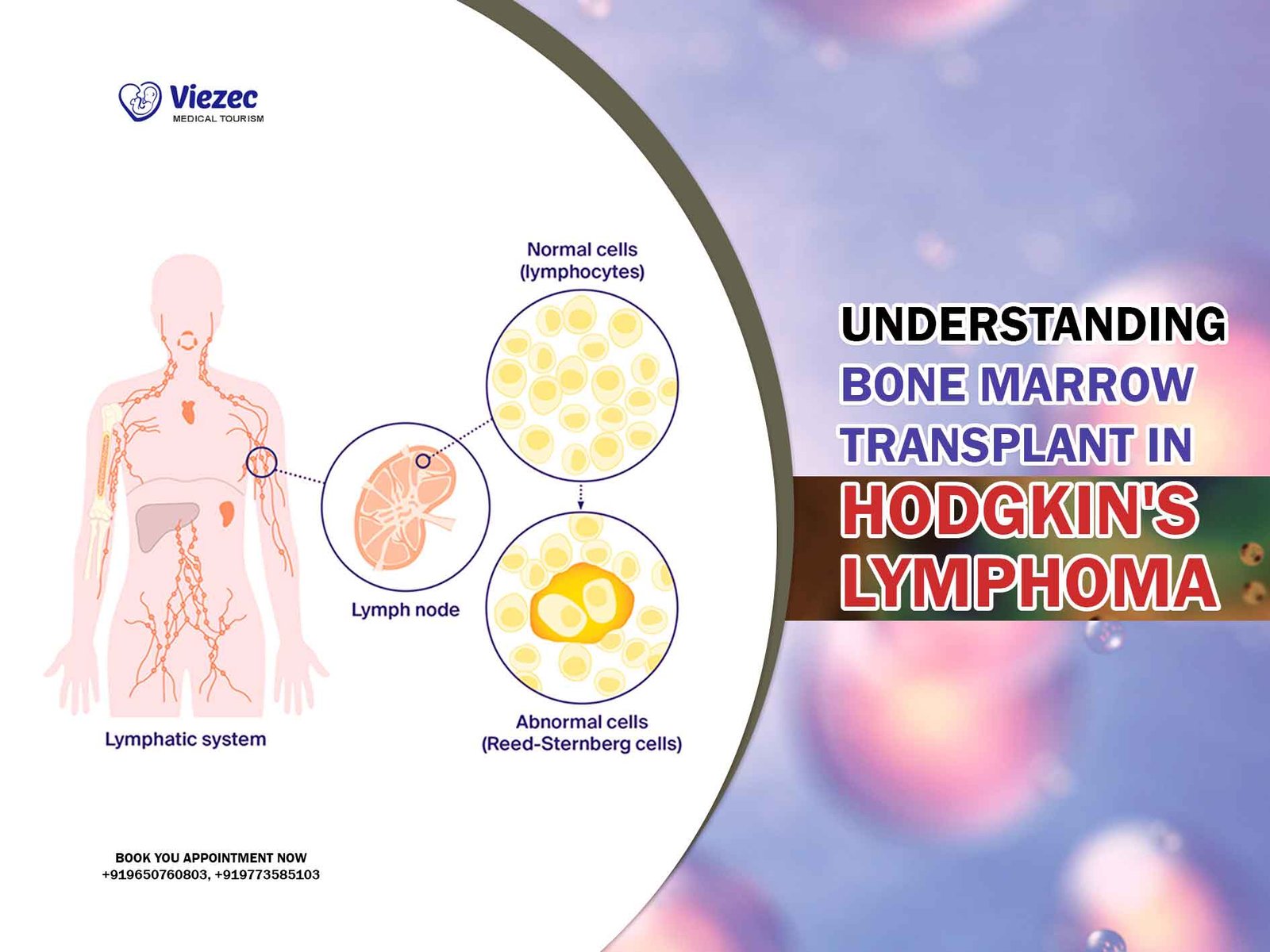
Enhancing Immune Surveillance
The immune system plays a crucial role in identifying and eliminating cancer cells. However, cancer can evade immune detection by various mechanisms, allowing it to proliferate unchecked. Bone marrow transplantation can bolster the patient’s immune response by replenishing the immune cell populations that may have been depleted by cancer treatments. This enhanced immune surveillance can help prevent cancer recurrence and improve long-term outcomes for patients with bone cancer.
Considerations for Bone Marrow Transplantation in Bone Cancer
Patient Selection
Not all patients with bone cancer are candidates for bone marrow transplantation. The decision to undergo a transplant depends on several factors, including the type and stage of cancer, the patient’s overall health status, and the availability of suitable donors. A thorough evaluation by a multidisciplinary team of oncologists, hematologists, and transplant specialists is essential to determine the suitability of bone marrow transplantation for each individual patient.
Risks and Complications
Like any medical procedure, bone marrow transplantation carries risks and potential complications. These may include infection, graft-versus-host disease (GVHD) in allogeneic transplants, organ damage, and graft failure. Patients undergoing transplantation require close monitoring and supportive care to manage these potential complications and maximize the chances of a successful outcome.
Long-Term Follow-Up
Bone marrow transplantation can have long-lasting effects on the patient’s health and quality of life. Long-term follow-up is essential to monitor for late effects such as secondary cancers, infertility, and chronic graft-versus-host disease. Patients who undergo transplantation require ongoing medical surveillance and supportive care to address any late complications and optimize their long-term outcomes.
Current Research and Future Directions
Advancements in Transplantation Techniques
Recent advancements in transplantation techniques, such as reduced-intensity conditioning regimens and haploidentical transplantation, have expanded the pool of eligible candidates for bone marrow transplantation. These innovations have made transplantation safer and more accessible for patients with bone cancer, leading to improved outcomes and survival rates.
Targeted Therapies and Immunotherapy
Emerging targeted therapies and immunotherapies hold promise for improving the efficacy of bone marrow transplantation in treating bone cancer. By targeting specific molecular pathways involved in cancer growth and metastasis, these therapies can complement the effects of transplantation and enhance its anti-cancer effects. Clinical trials are underway to evaluate the safety and efficacy of combining transplantation with novel targeted agents and immunotherapies in patients with bone cancer.
Personalized Medicine Approaches
Advances in genomic profiling and precision medicine have paved the way for personalized treatment approaches in bone cancer. By analyzing the genetic makeup of individual tumors, oncologists can identify specific molecular abnormalities driving cancer growth and tailor treatment strategies accordingly. Personalized medicine approaches hold the potential to optimize the selection of candidates for bone marrow transplantation and improve outcomes for patients with bone cancer.
Bone marrow transplantation represents a promising option for the treatment of bone cancer, particularly in cases where conventional therapies have failed or are unlikely to succeed. By replenishing the patient’s bone marrow with healthy stem cells, transplantation can overcome treatment resistance, target metastatic disease, and enhance immune surveillance, leading to improved outcomes and survival rates. Ongoing research efforts aimed at refining transplantation techniques, identifying novel therapeutic targets, and implementing personalized treatment approaches are likely to further advance the field and improve outcomes for patients with bone cancer in the years to come.