Myelofibrosis is a rare and serious bone marrow disorder characterized by the abnormal production of blood cells. It falls under the category of myeloproliferative neoplasms, which involve the overproduction of blood cells in the bone marrow. Myelofibrosis disrupts the normal production of blood cells, leading to symptoms such as fatigue, weakness, anemia, and an enlarged spleen.
While there are several treatment options available for myelofibrosis, including medications and radiation therapy, bone marrow transplant (BMT) remains one of the most effective treatments for eligible patients. In this comprehensive guide, we will explore the different types of bone marrow transplant options available for myelofibrosis patients, the criteria for eligibility, the transplant process, and the potential risks and benefits involved.
Understanding Myelofibrosis
What is Myelofibrosis?
Myelofibrosis is a chronic and progressive disorder that affects the bone marrow, causing the excessive production of fibrous tissue and leading to the disruption of normal blood cell production. The condition can be primary, meaning it develops on its own, or secondary, occurring as a result of other blood disorders such as polycythemia vera or essential thrombocythemia.
Symptoms of Myelofibrosis
The symptoms of myelofibrosis can vary widely from person to person but may include:
- Fatigue and weakness
- Shortness of breath
- Easy bruising or bleeding
- Enlarged spleen (splenomegaly)
- Bone pain
- Night sweats
- Fever
- Unexplained weight loss
Treatment Options for Myelofibrosis
Medications
Several medications are available to manage the symptoms of myelofibrosis and slow down the progression of the disease. These may include:
- JAK Inhibitors: Drugs such as ruxolitinib can help reduce spleen size and alleviate symptoms.
- Androgens: These hormones may be prescribed to stimulate red blood cell production.
- Immunomodulatory Drugs: Agents like thalidomide or lenalidomide may be used to suppress the abnormal production of blood cells.
Radiation Therapy
Radiation therapy may be used to reduce the size of an enlarged spleen or alleviate bone pain associated with myelofibrosis.
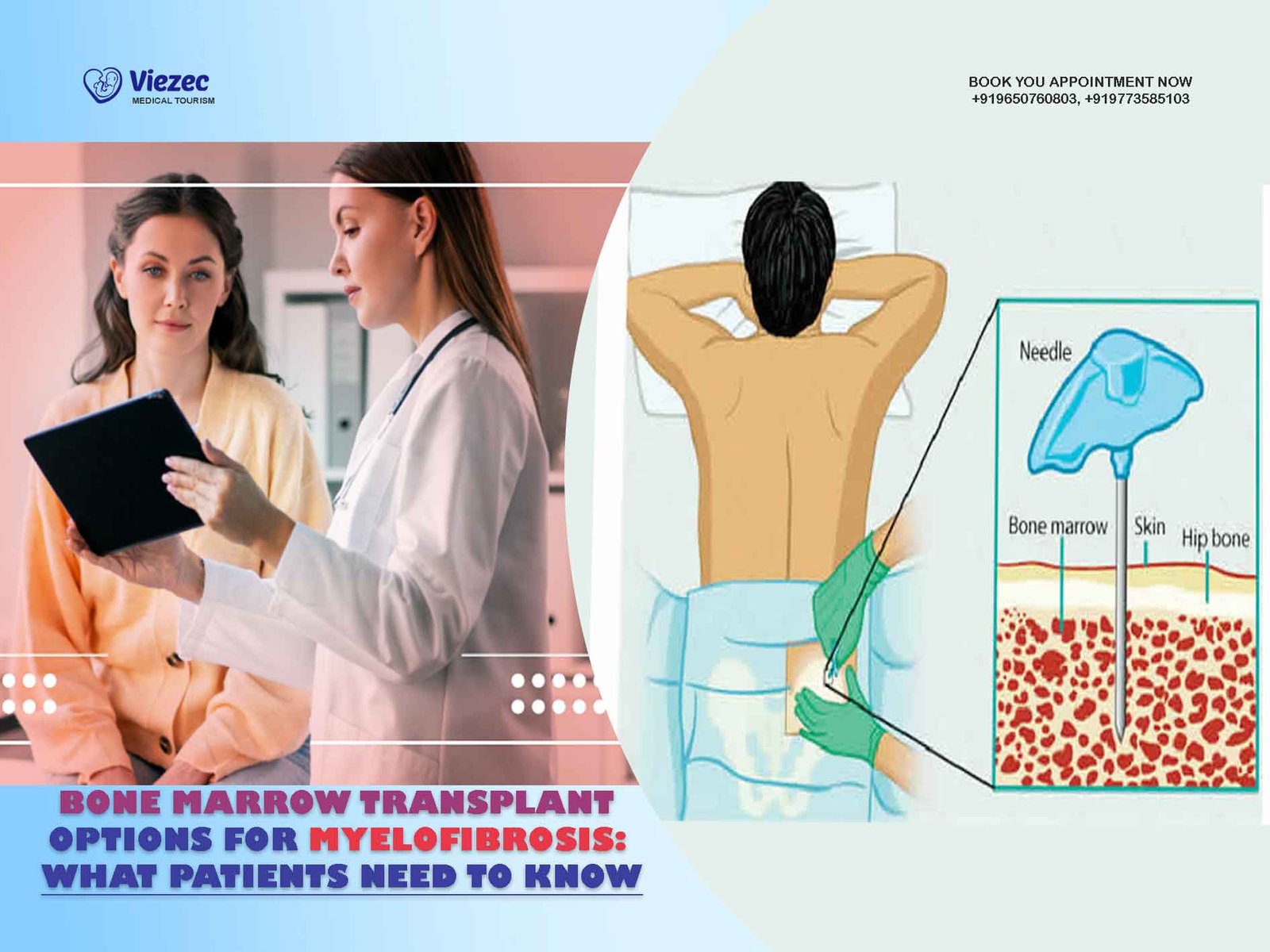
Bone Marrow Transplant (BMT)
Bone marrow transplant, also known as hematopoietic stem cell transplant (HSCT), offers a potentially curative treatment option for eligible myelofibrosis patients. BMT involves replacing diseased or damaged bone marrow with healthy stem cells from a donor.
Types of Bone Marrow Transplants
Autologous Transplant
In an autologous transplant, the patient’s own stem cells are collected and stored before undergoing high-dose chemotherapy or radiation therapy. After treatment, the stored stem cells are returned to the patient’s body to help regenerate healthy bone marrow.
Allogeneic Transplant
In an allogeneic transplant, stem cells are obtained from a compatible donor, typically a sibling or unrelated matched donor. The donor’s stem cells are then infused into the patient’s bloodstream, where they travel to the bone marrow and begin producing healthy blood cells.
Reduced-Intensity Conditioning (RIC) Transplant
In a reduced-intensity conditioning transplant, lower doses of chemotherapy and/or radiation are used compared to traditional transplant approaches. This approach is often preferred for older patients or those with underlying health conditions who may not tolerate high-dose therapy.
Eligibility Criteria for Bone Marrow Transplant
General Health
Patients undergoing bone marrow transplant must be in relatively good overall health to tolerate the intensive treatment regimen and recovery process.
Age
While age alone is not a strict criterion for eligibility, older patients may face increased risks associated with transplant procedures. However, advancements in transplant techniques have expanded eligibility criteria for older patients.
Disease Status
The stage and progression of myelofibrosis will influence a patient’s eligibility for transplant. Patients with advanced disease or significant comorbidities may not be suitable candidates.
Donor Availability
For allogeneic transplants, the availability of a suitable donor—either related or unrelated—is crucial. Patients without a compatible donor may explore alternative transplant options or clinical trials.
Transplant Process
Pre-Transplant Evaluation
Before undergoing a bone marrow transplant, patients undergo a comprehensive evaluation to assess their overall health and suitability for the procedure. This may involve medical tests, imaging studies, and consultations with various specialists.
Stem Cell Collection
For autologous transplants, the patient’s stem cells are collected through a process called apheresis. During apheresis, blood is drawn from the patient, and the stem cells are separated and collected before the remaining blood components are returned to the patient’s body.
Conditioning Regimen
Prior to transplant, patients may undergo a conditioning regimen involving chemotherapy, radiation therapy, or a combination of both. This helps suppress the patient’s immune system and create space within the bone marrow for the donor cells to engraft successfully.
Transplantation
The transplant procedure involves infusing the donor’s stem cells into the patient’s bloodstream through a central venous catheter. The stem cells then travel to the bone marrow, where they begin to multiply and produce healthy blood cells.
Engraftment and Recovery
Following transplant, patients are closely monitored for signs of engraftment, which occurs when the donor cells establish themselves in the patient’s bone marrow and begin producing new blood cells. The recovery process typically involves a prolonged hospital stay and close follow-up care.
Risks and Complications
Graft-versus-Host Disease (GVHD)
Graft-versus-host disease is a potentially serious complication of allogeneic transplants, where the donor’s immune cells attack the recipient’s tissues. GVHD can affect the skin, liver, and gastrointestinal tract and may require immunosuppressive therapy.
Infection
The suppression of the immune system during the transplant process increases the risk of infections, which can be bacterial, viral, or fungal in nature. Patients may receive prophylactic antibiotics or antiviral medications to prevent infections.
Graft Failure
In some cases, the transplanted stem cells may fail to engraft and produce new blood cells, leading to graft failure. This may necessitate additional treatments or a second transplant.
Long-Term Side Effects
Patients who undergo bone marrow transplant may experience long-term side effects, including infertility, secondary cancers, and organ damage from chemotherapy or radiation therapy.
Make a Decision
Bone marrow transplant offers a potentially curative treatment option for eligible myelofibrosis patients. While the procedure carries risks and complications, advancements in transplant techniques and supportive care have improved outcomes and expanded eligibility criteria. Patients considering bone marrow transplant should discuss the potential risks and benefits with their healthcare team to make informed decisions about their treatment options. With careful planning and ongoing support, bone marrow transplant can provide hope for improved quality of life and long-term survival for patients with myelofibrosis.