In recent years, the field of regenerative medicine has witnessed remarkable progress, offering new hope for the treatment of various diseases. Among the promising avenues explored is the potential use of stem cells to repair damaged organs, including the lungs. The respiratory system, with its intricate structure and vulnerability to various insults, often faces challenges in terms of damage and disease. This article delves into the intricate world of stem cells and their capacity to repair damaged lungs, exploring the current state of research, the challenges faced, and the potential breakthroughs that could revolutionize respiratory medicine.
Understanding Stem Cells
Basics of Stem Cells
Stem cells are undifferentiated cells with the remarkable ability to differentiate into specialized cell types. They are characterized by two essential properties: self-renewal and pluripotency. Self-renewal allows stem cells to divide and produce identical daughter cells, maintaining an undifferentiated state. Pluripotency, on the other hand, enables them to differentiate into various cell types, making them a versatile tool for regenerative medicine.
There are two main types of stem cells: embryonic stem cells (ESCs) and adult or somatic stem cells. ESCs are derived from embryos and have the potential to differentiate into any cell type in the human body. Adult stem cells, also known as somatic or tissue-specific stem cells, are found in various tissues and are more restricted in their differentiation potential.
Types of Stem Cells Relevant to Lung Repair
Mesenchymal Stem Cells (MSCs)
Mesenchymal stem cells (MSCs) are a type of adult stem cell that holds significant promise for lung repair. These multipotent cells can differentiate into various cell types, including bone, cartilage, and adipose tissue. Moreover, MSCs possess immunomodulatory properties, making them an attractive candidate for treating inflammatory lung diseases.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are generated by reprogramming adult cells to a pluripotent state. Like embryonic stem cells, iPSCs can differentiate into any cell type. This technology provides a potential source of patient-specific stem cells, minimizing the risk of immune rejection. iPSCs have shown promise in lung regeneration, offering a personalized approach to treatment.
Lung Microenvironment
Understanding Lung Damage
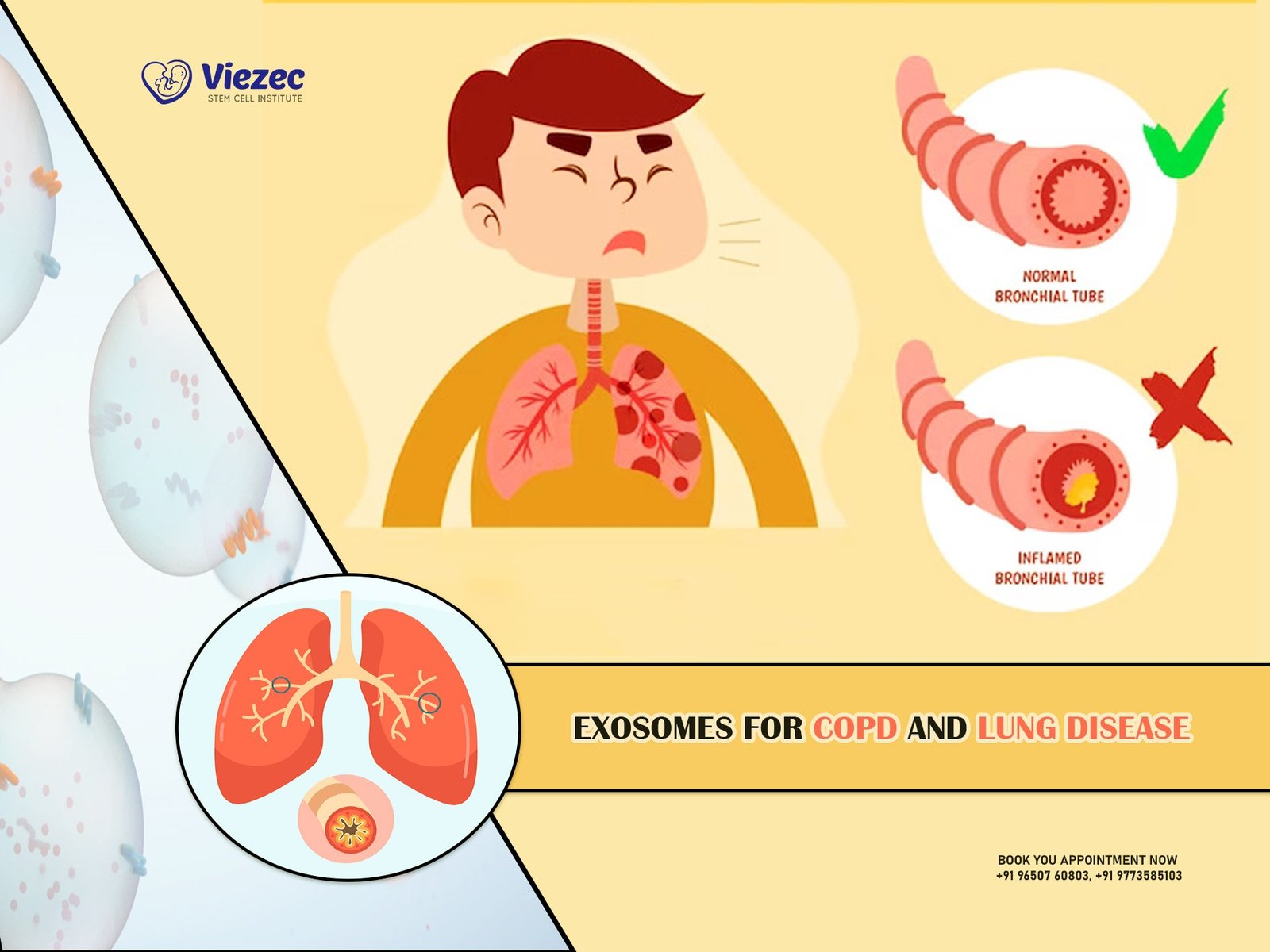
The lungs are complex organs composed of a delicate network of airways, blood vessels, and alveoli. Exposure to environmental factors, infections, or chronic diseases can lead to lung damage. Common lung conditions, such as chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), and acute respiratory distress syndrome (ARDS), highlight the need for effective therapies to repair damaged lung tissue.
Stem Cell Interaction with the Lung Microenvironment
Homing and Engraftment
For stem cells to effectively repair damaged lungs, they must navigate the complex lung microenvironment. Homing, the process by which stem cells migrate to the site of injury, and engraftment, the successful integration of stem cells into the damaged tissue, are crucial steps. Understanding the interactions between stem cells and the lung microenvironment is essential for developing targeted and effective therapies.
Immunomodulation
The lung is a highly immune-responsive organ, and inflammatory responses often accompany tissue damage. Stem cells, particularly MSCs, exert immunomodulatory effects by regulating the immune system’s inflammatory and anti-inflammatory responses. This property is vital for mitigating excessive inflammation and promoting a regenerative environment in the damaged lungs.
Current State of Research
Preclinical Studies
Animal Models
Preclinical studies using animal models have provided valuable insights into the potential of stem cells for lung repair. Various studies have demonstrated the ability of stem cells, particularly MSCs, to ameliorate lung injury, reduce inflammation, and enhance tissue regeneration in animal models of lung diseases. These findings form a foundation for advancing to clinical trials.
Challenges and Limitations
While preclinical studies show promise, several challenges must be addressed before stem cell therapies for lung repair can become a clinical reality. These challenges include optimizing cell delivery methods, ensuring long-term engraftment, and understanding the long-term safety of stem cell treatments.
Clinical Trials
Mesenchymal Stem Cells in Clinical Trials
The translation of stem cell therapies from the laboratory to clinical practice is underway. Clinical trials focusing on the use of MSCs for lung repair are exploring safety, efficacy, and optimal delivery methods. Preliminary results from some trials show encouraging outcomes, but the full potential of stem cells in clinical settings is yet to be realized.
Challenges in Clinical Translation
Clinical translation of stem cell therapies faces challenges related to standardization of protocols, ethical considerations, and the need for rigorous safety assessments. Addressing these challenges is crucial for establishing the safety and efficacy of stem cell treatments for lung diseases in diverse patient populations.
Future Directions
Advancements in Stem Cell Technology
CRISPR/Cas9 and Gene Editing
Advancements in gene-editing technologies, such as CRISPR/Cas9, offer exciting possibilities for enhancing the therapeutic potential of stem cells. Precise manipulation of stem cells’ genetic makeup may improve their engraftment, differentiation capacity, and immunomodulatory effects, paving the way for more effective lung repair.
3D Bioprinting and Tissue Engineering
The integration of stem cells with 3D bioprinting and tissue engineering holds promise for creating functional lung tissue ex vivo. This innovative approach may overcome challenges associated with in vivo cell delivery and provide a personalized and scalable solution for lung repair.
Overcoming Immunological Barriers
Immune-Evasive Strategies
The immune system poses a significant challenge to the success of stem cell therapies. Developing strategies to enhance the immune evasion of transplanted stem cells, such as encapsulation techniques or modification of cell surface markers, is essential for long-term engraftment and sustained therapeutic effects.
Personalized Medicine Approaches
Patient-Specific iPSCs
The use of patient-specific iPSCs opens avenues for personalized medicine in lung repair. Generating stem cells from a patient’s own cells reduces the risk of immune rejection and offers a tailored approach to treatment, taking into account the individual’s genetic and cellular characteristics.
Ethical Considerations and Regulatory Landscape
Ethical Considerations
The use of stem cells in research and therapy raises ethical questions related to their derivation, manipulation, and transplantation. Addressing these ethical concerns is crucial for ensuring responsible and transparent practices in the development and application of stem cell therapies for lung repair.
Regulatory Landscape
The regulatory framework for stem cell therapies is evolving to ensure the safety and efficacy of these innovative treatments. Regulatory agencies worldwide are actively engaged in establishing guidelines and standards for the development and approval of stem cell-based therapies, balancing the need for innovation with patient safety.
As we navigate the intricate landscape of stem cell therapy for lung repair, the potential for transformative breakthroughs is palpable. Stem cells, with their regenerative and immunomodulatory properties, offer hope for addressing the challenges posed by lung diseases. While preclinical studies and early-phase clinical trials show promise, there is much work to be done to optimize stem cell therapies, address challenges, and ensure their safe and effective integration into clinical practice. The future of respiratory medicine may well be shaped by the ongoing research and advancements in stem cell technology, ushering in a new era of personalized and regenerative treatments for damaged lungs.