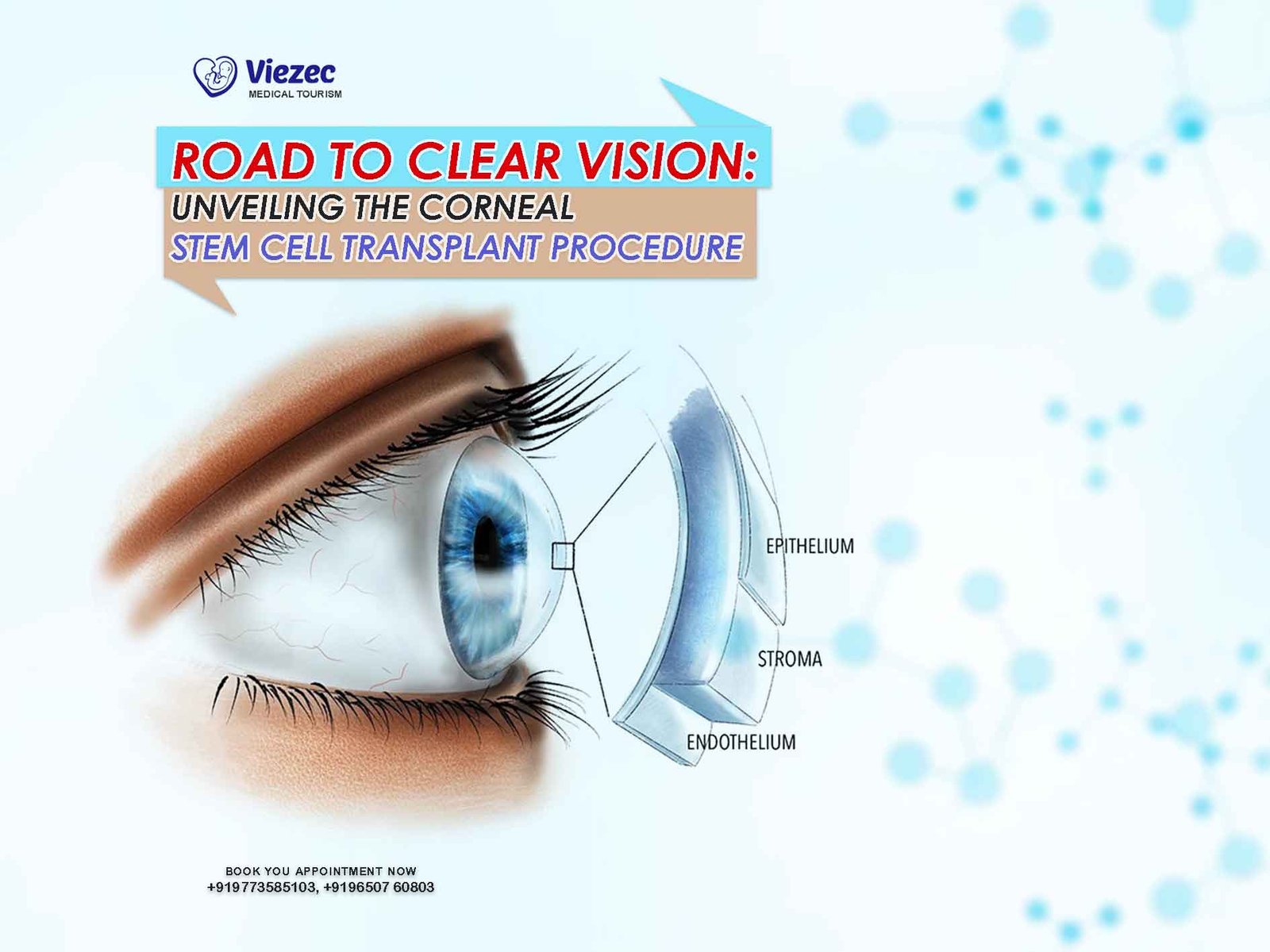
The quest for clear vision has been a driving force behind medical advancements throughout history. Vision, being one of the most crucial senses, significantly impacts our daily lives. Unfortunately, various conditions can compromise visual acuity, with corneal diseases being among the most prevalent. The cornea, the transparent outer layer of the eye, is vital for focusing light onto the retina, enabling clear vision. When the cornea is damaged or diseased, it can severely impair vision, leading to blindness if left untreated. Traditional treatment methods have often fallen short in providing adequate solutions, but recent advancements in medical science have opened up new avenues for restoring vision. One such breakthrough is the corneal stem cell transplant procedure, offering hope to countless individuals struggling with corneal diseases.
Understanding Corneal Diseases
Before delving into the intricacies of corneal stem cell transplant, it’s essential to grasp the nature of corneal diseases and their impact on vision. The cornea serves as a protective barrier against dust, germs, and other harmful particles while also contributing to the eye’s focusing power. However, various factors, including infections, injuries, genetic disorders, and aging, can lead to corneal damage or disease.
Types of Corneal Diseases
Corneal diseases encompass a broad spectrum of conditions, each with its own set of symptoms and causes. Some common corneal diseases include:
Keratoconus
Keratoconus is a progressive condition characterized by the thinning and bulging of the cornea into a cone shape. This irregularity disrupts the cornea’s ability to refract light properly, resulting in distorted vision, increased sensitivity to light, and astigmatism.
Corneal Dystrophies
Corneal dystrophies refer to a group of inherited conditions wherein abnormal material accumulates in the cornea, leading to clouding, distortion, and eventual vision loss. Examples include Fuchs’ dystrophy and lattice dystrophy.
Corneal Scarring
Corneal scarring can result from injuries, infections, or previous surgeries. Scars on the cornea can obstruct the passage of light, causing blurred or distorted vision.
Impact on Quality of Life
Corneal diseases can significantly impact an individual’s quality of life, affecting their ability to perform daily tasks, drive safely, and engage in activities they enjoy. Moreover, severe corneal conditions can lead to chronic pain, discomfort, and ultimately, vision loss.
Role of Stem Cells in Corneal Regeneration
Stem cells hold immense potential in regenerative medicine due to their unique ability to differentiate into various cell types and proliferate indefinitely. In the context of corneal regeneration, limbal stem cells play a pivotal role. The limbus, located at the junction between the cornea and the sclera, harbors a niche of stem cells responsible for maintaining the integrity and transparency of the cornea.
Limbal Stem Cell Deficiency (LSCD)
Limbal stem cell deficiency (LSCD) occurs when there is a depletion or dysfunction of limbal stem cells, leading to impaired corneal epithelial regeneration. LSCD can result from chemical burns, ocular trauma, autoimmune diseases, or congenital disorders. Without proper limbal stem cell function, the cornea loses its regenerative capacity, leading to persistent epithelial defects, corneal neovascularization, and scarring.
Importance of Corneal Epithelial Regeneration
The corneal epithelium serves as a protective barrier against pathogens and maintains the smooth optical surface necessary for clear vision. Therefore, restoring corneal epithelial integrity is essential in treating conditions associated with LSCD.
Corneal Stem Cell Transplant Procedure: A Step-by-Step Guide
The corneal stem cell transplant procedure, also known as limbal stem cell transplantation (LSCT), aims to replenish the limbal stem cell population and restore corneal epithelial function. The procedure typically involves the following steps:
Patient Evaluation
Before proceeding with LSCT, a comprehensive eye examination is conducted to assess the extent of corneal damage and determine the suitability of the patient for the procedure. This evaluation may include visual acuity tests, corneal imaging, and assessment of ocular surface health.
Donor Selection
In allogeneic LSCT, where donor tissue is used, careful donor selection is crucial to minimize the risk of graft rejection and transmission of infectious diseases. Donor tissue is obtained from cadaveric or living donors, with stringent screening protocols in place to ensure donor suitability.
Harvesting of Limbal Stem Cells
Limbal stem cells can be harvested from either the patient’s healthy eye (autologous transplantation) or a donor eye (allogeneic transplantation). Various techniques, such as limbal biopsy or tissue grafting, may be employed to obtain limbal stem cells while preserving their regenerative capacity.
Preparation of Recipient Bed
The recipient cornea is prepared to receive the transplanted limbal stem cells. This may involve the removal of scar tissue, epithelial debridement, or creation of a niche conducive to stem cell engraftment.
Transplantation of Limbal Stem Cells
The harvested limbal stem cells are then transplanted onto the recipient cornea using delicate surgical techniques. The cells are carefully positioned to ensure optimal integration and survival within the ocular microenvironment.
Postoperative Care
Following LSCT, meticulous postoperative care is essential to promote graft survival and corneal epithelialization. This may include the use of topical medications, such as antibiotics and corticosteroids, to prevent infection and inflammation, as well as regular follow-up visits to monitor progress.
Advancements and Innovations in LSCT
Over the years, significant advancements and innovations have enhanced the efficacy and safety of LSCT, paving the way for improved outcomes and broader applicability. Some notable developments include:
Cultivated Limbal Epithelial Transplantation (CLET)
Cultivated limbal epithelial transplantation (CLET) involves ex vivo expansion of limbal stem cells obtained from a small biopsy of healthy limbal tissue. This allows for the generation of a sufficient number of cells for transplantation, reducing the need for large donor grafts and minimizing the risk of immune rejection.
Tissue Engineering Approaches
Tissue engineering approaches aim to create bioengineered corneal substitutes using biocompatible scaffolds seeded with limbal stem cells. These constructs mimic the native corneal microenvironment and hold promise for providing long-term functional restoration in cases of extensive corneal damage.
Novel Therapeutic Agents
Advances in regenerative medicine have led to the development of novel therapeutic agents, such as growth factors, cytokines, and small molecules, that can enhance the survival and functionality of transplanted stem cells. These adjunctive treatments may improve graft integration and accelerate corneal epithelial healing.