Crohn’s Disease, a chronic inflammatory disorder of the gastrointestinal tract, affects millions worldwide, causing debilitating symptoms and impacting the quality of life of those afflicted. Traditional treatment approaches, including medications and surgery, have limitations in efficacy and safety. However, recent advancements in medical science have shed light on novel therapeutic avenues, one of which is bone marrow transplantation (BMT). This article explores the potential of BMT as a treatment for Crohn’s Disease, delving into its mechanisms, current research findings, challenges, and future prospects.
Understanding Crohn’s Disease
Before delving into the intricacies of bone marrow transplantation, it’s crucial to understand the nature of Crohn’s Disease. This condition, categorized under inflammatory bowel diseases (IBD), involves chronic inflammation of the gastrointestinal tract, typically affecting the small intestine and colon. The exact cause of Crohn’s Disease remains elusive, although it is believed to involve a complex interplay of genetic, environmental, and immunological factors.
Symptoms and Impact
Crohn’s Disease manifests through various symptoms, including abdominal pain, diarrhea, rectal bleeding, fatigue, and weight loss. These symptoms can range from mild to severe, significantly impairing an individual’s daily functioning and overall well-being. Furthermore, Crohn’s Disease is associated with complications such as bowel strictures, fistulas, and increased risk of colorectal cancer, further exacerbating its clinical burden.
Current Treatment Landscape
Managing Crohn’s Disease involves a multidisciplinary approach aimed at inducing and maintaining remission while alleviating symptoms and improving quality of life. Conventional treatment modalities include:
- Medications: Anti-inflammatory drugs, immunosuppressants, antibiotics, and biologic agents are commonly prescribed to reduce inflammation and modulate the immune response.
- Nutritional Therapy: Exclusive enteral nutrition (EEN) and dietary modifications may be employed to alleviate symptoms and promote mucosal healing.
- Surgery: In cases of severe complications or refractory disease, surgical intervention such as bowel resection or ostomy placement may be necessary to alleviate symptoms and improve quality of life.
Despite these treatment options, many patients experience disease relapse, medication intolerance, or inadequate response, underscoring the need for alternative therapeutic strategies.
Role of Bone Marrow Transplantation
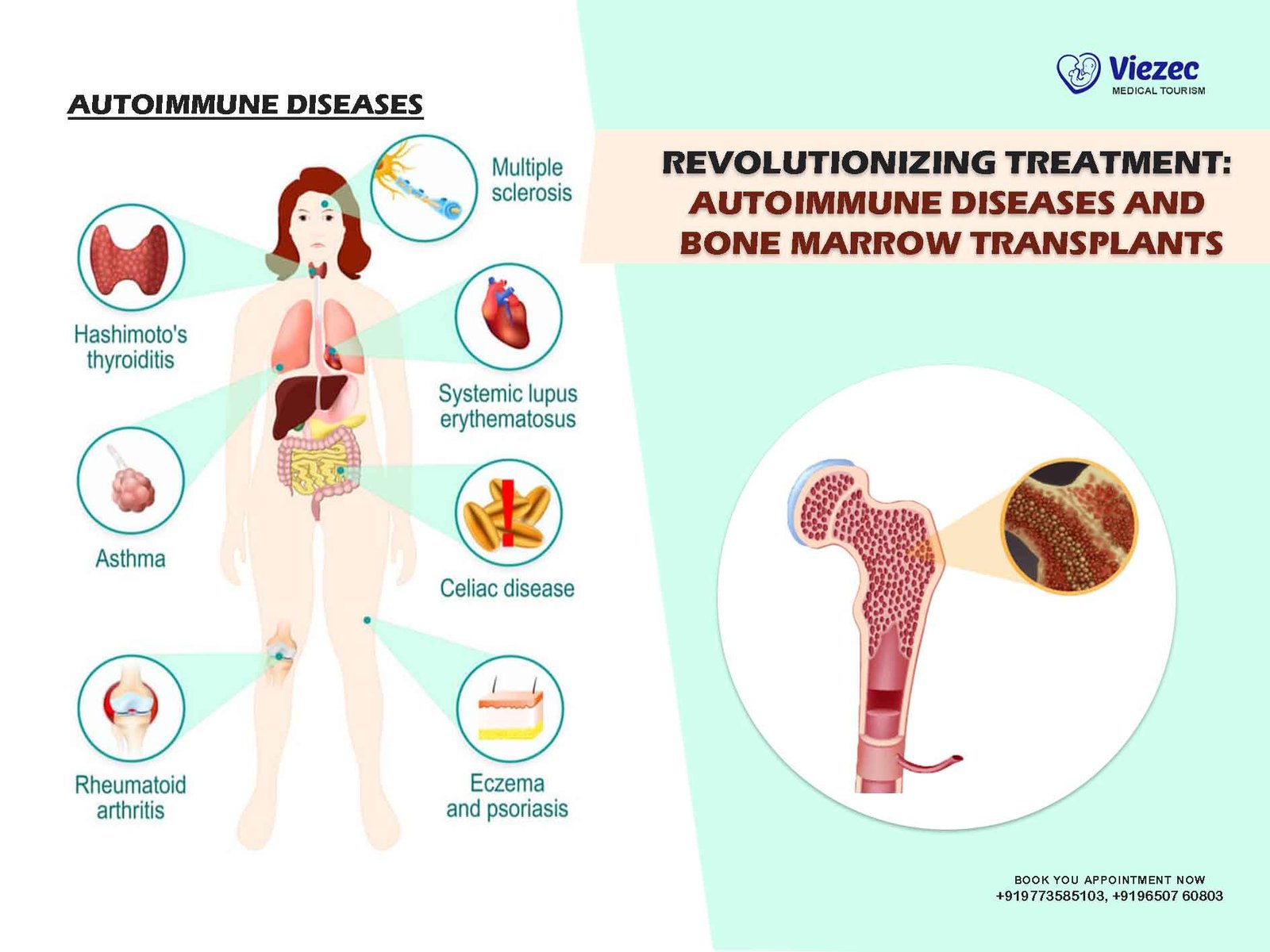
Bone marrow transplantation (BMT), long established as a curative therapy for hematologic malignancies and certain autoimmune disorders, has emerged as a potential therapeutic option for Crohn’s Disease. The rationale behind BMT in Crohn’s Disease lies in its ability to reset the immune system, thereby interrupting the pathological inflammatory cascade characteristic of the condition.
Mechanisms of Action
BMT involves the infusion of healthy hematopoietic stem cells, derived from either the patient (autologous transplantation) or a compatible donor (allogeneic transplantation). These stem cells possess the capacity to differentiate into various blood cell lineages and exert immunomodulatory effects. In the context of Crohn’s Disease, BMT aims to achieve immune reconstitution and tolerance induction, thereby restoring immune homeostasis and ameliorating intestinal inflammation.
Research Evidence
Early clinical trials investigating the efficacy of BMT in Crohn’s Disease have shown promising results. A landmark study published in The New England Journal of Medicine demonstrated significant clinical improvement and mucosal healing in patients with refractory Crohn’s Disease who underwent autologous hematopoietic stem cell transplantation. Subsequent studies have corroborated these findings, highlighting the potential of BMT as a therapeutic intervention for severe and refractory cases of Crohn’s Disease.
Challenges and Considerations
Despite its potential benefits, BMT for Crohn’s Disease is not without challenges and considerations:
- Risk of Complications: BMT carries inherent risks, including infection, graft-versus-host disease (GVHD), and organ toxicity, which necessitate careful patient selection and comprehensive risk assessment.
- Optimal Timing and Patient Selection: Identifying the most appropriate candidates for BMT and determining the optimal timing of intervention remain areas of active investigation, as patient heterogeneity and disease dynamics pose challenges in this regard.
- Long-term Outcomes: Long-term data on the efficacy and safety of BMT in Crohn’s Disease are limited, underscoring the need for further research to elucidate its durability and potential adverse effects over time.
Future Directions and Conclusion
The exploration of bone marrow transplantat as a therapeutic avenue for Crohn’s Disease represents a paradigm shift in the management of this chronic inflammatory condition. As research efforts continue to elucidate its mechanisms, optimize treatment protocols, and assess long-term outcomes, BMT holds the promise of providing durable remission and improved quality of life for patients with refractory Crohn’s Disease.
In conclusion, bone marrow transplantation offers a novel and potentially transformative approach to addressing the unmet needs of individuals suffering from severe and refractory Crohn’s Disease. While challenges remain, ongoing research and clinical trials hold the key to harnessing the full therapeutic potential of BMT in the management of this debilitating condition. By unraveling the complexities of immune dysregulation and inflammation, BMT may pave the way for personalized and precision medicine approaches in the era of inflammatory bowel diseases.