Stem cell therapy has emerged as a groundbreaking approach in the treatment of various diseases, including cancer. Stem cells are unique in their ability to differentiate into various cell types and self-renew, making them a promising tool for regenerative medicine. In cancer therapy, stem cells can potentially replace damaged tissues, improve immune responses, and even target cancer cells directly. This innovative treatment approach has gained considerable attention from researchers and clinicians worldwide, aiming to offer new hope to cancer patients who have exhausted traditional treatment options.
Importance of Evaluating Effectiveness in Cancer Treatment
Evaluating the effectiveness of stem cell therapy in cancer treatment is crucial for several reasons. First, it helps determine the therapeutic potential and safety of stem cell-based interventions, ensuring that patients receive the most effective care. Second, it provides valuable insights into the mechanisms by which stem cells interact with cancer cells and the host environment, informing the development of more targeted therapies. Lastly, rigorous evaluation allows for the identification of potential risks and complications, which is essential for refining treatment protocols and ensuring patient safety.
Scope and Objectives of the Study
The scope of this study encompasses a comprehensive analysis of stem cell therapy’s effectiveness in treating various types of cancer. The primary objectives are to assess the clinical outcomes of stem cell treatments, compare them with conventional therapies, and explore the underlying mechanisms of action. Additionally, the study aims to evaluate the safety and ethical considerations associated with stem cell therapy, providing a balanced perspective on its potential benefits and limitations. By achieving these objectives, the study seeks to contribute to the growing body of knowledge on stem cell therapy and its role in cancer treatment.
Background
History of Stem Cell Research
The history of stem cell research dates back to the early 20th century when scientists first discovered that certain cells had the potential to regenerate damaged tissues. Over the decades, significant milestones have been achieved, including the identification of embryonic stem cells in the 1980s and the development of induced pluripotent stem cells (iPSCs) in the early 2000s. These breakthroughs have paved the way for exploring stem cells’ therapeutic potential in various medical fields, including oncology. The evolution of stem cell research has been marked by numerous scientific, ethical, and regulatory challenges, which have shaped the current landscape of stem cell therapy.
Types of Stem Cells Used in Therapy
Stem cells used in therapy can be broadly categorized into three types: embryonic stem cells, adult stem cells, and induced pluripotent stem cells (iPSCs). Each type has distinct characteristics and potential applications in cancer treatment.
Embryonic Stem Cells
Embryonic stem cells (ESCs) are derived from early-stage embryos and have the ability to differentiate into any cell type in the body. This pluripotency makes them highly versatile for regenerative medicine. However, the use of ESCs in therapy raises significant ethical concerns due to the destruction of embryos, limiting their widespread application in clinical settings. Despite these challenges, ESCs remain a valuable resource for understanding cellular differentiation and developing new treatment strategies.
Adult Stem Cells
Adult stem cells, also known as somatic stem cells, are found in various tissues throughout the body. They are multipotent, meaning they can differentiate into a limited range of cell types related to their tissue of origin. Hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs) are the most commonly used adult stem cells in cancer therapy. HSCs are primarily used in bone marrow transplants for blood cancers, while MSCs have shown potential in treating solid tumors and modulating immune responses.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are created by reprogramming adult cells to revert to a pluripotent state, similar to that of embryonic stem cells. This innovative technology, developed by Shinya Yamanaka and colleagues, has revolutionized stem cell research by providing a source of pluripotent cells without the ethical issues associated with ESCs. iPSCs have significant potential in personalized medicine, allowing for the development of patient-specific therapies that can improve treatment outcomes and reduce the risk of immune rejection.
Mechanisms of Action in Cancer Treatment
The mechanisms by which stem cells exert their therapeutic effects in cancer treatment are diverse and complex. One primary mechanism is the replacement of damaged or diseased tissues with healthy cells, promoting tissue regeneration and repair. Additionally, stem cells can modulate the immune system, enhancing the body’s ability to recognize and attack cancer cells. Some stem cells have been engineered to deliver therapeutic agents directly to tumors, providing targeted treatment with minimal side effects. Understanding these mechanisms is essential for optimizing stem cell therapies and maximizing their effectiveness in cancer treatment.
Methodology
Research Design
The research design for evaluating the effectiveness of stem cell therapy in cancer treatment involves a combination of clinical trials, patient surveys, and medical records review. This mixed-methods approach allows for a comprehensive assessment of clinical outcomes, patient experiences, and long-term effects of stem cell therapies. Randomized controlled trials (RCTs) are considered the gold standard for evaluating treatment efficacy, providing robust evidence on the benefits and risks of stem cell interventions compared to standard treatments.
Sample Selection
Selecting an appropriate sample is crucial for the validity and reliability of the study. The sample should include a diverse group of cancer patients who have undergone stem cell therapy, representing various cancer types, stages, and demographic characteristics. This diversity ensures that the findings are generalizable and applicable to a broad patient population.
Inclusion Criteria
Inclusion criteria define the characteristics that patients must have to participate in the study. These criteria may include a confirmed diagnosis of cancer, eligibility for stem cell therapy based on clinical guidelines, and informed consent to participate in the study. Additional criteria may be set based on specific research objectives, such as focusing on particular cancer types or stages.
Exclusion Criteria
Exclusion criteria outline the conditions or characteristics that disqualify patients from participating in the study. These may include contraindications to stem cell therapy, severe comorbidities that could confound the results, and previous participation in similar studies. Establishing clear exclusion criteria helps ensure the safety of participants and the integrity of the study findings.
Data Collection Methods
Data collection methods for this study include clinical trials, patient surveys, and medical records review. Each method provides unique insights into the effectiveness of stem cell therapy and contributes to a comprehensive understanding of its impact on cancer treatment.
Clinical Trials
Clinical trials are essential for evaluating the safety and efficacy of new treatments. In the context of stem cell therapy, clinical trials involve administering stem cell-based interventions to cancer patients and monitoring their clinical outcomes over time. These trials are typically conducted in multiple phases, starting with small-scale studies to assess safety and progressing to larger trials to evaluate efficacy and long-term effects.
Patient Surveys
Patient surveys provide valuable information on the subjective experiences of individuals undergoing stem cell therapy. These surveys may include questions on quality of life, symptom management, and overall satisfaction with the treatment. Gathering patient-reported outcomes helps capture the holistic impact of stem cell therapy beyond clinical measures, providing a more comprehensive evaluation of its effectiveness.
Medical Records Review
Reviewing medical records allows researchers to collect detailed information on patients’ medical histories, treatment protocols, and clinical outcomes. This method provides a retrospective analysis of real-world data, complementing the findings from clinical trials and patient surveys. Medical records review is particularly useful for identifying long-term effects and potential complications of stem cell therapy.
Data Analysis Techniques
Data analysis techniques for this study include statistical analysis and comparative analysis. These techniques help interpret the collected data and draw meaningful conclusions about the effectiveness of stem cell therapy in cancer treatment.
Statistical Analysis
Statistical analysis involves applying mathematical methods to summarize and interpret the data. This may include calculating descriptive statistics, such as means and standard deviations, as well as conducting inferential tests, such as t-tests or chi-square tests, to determine the significance of the findings. Advanced statistical techniques, such as regression analysis or survival analysis, may also be used to explore relationships between variables and predict outcomes.
Comparative Analysis
Comparative analysis involves comparing the outcomes of stem cell therapy with those of conventional treatments, such as chemotherapy or radiation therapy. This analysis helps determine the relative effectiveness of different treatment modalities and identifies potential advantages or limitations of stem cell therapy. Comparative analysis may also include subgroup analyses to evaluate the effectiveness of stem cell therapy in specific patient populations or cancer types.
Clinical Applications of Stem Cell Therapy in Cancer
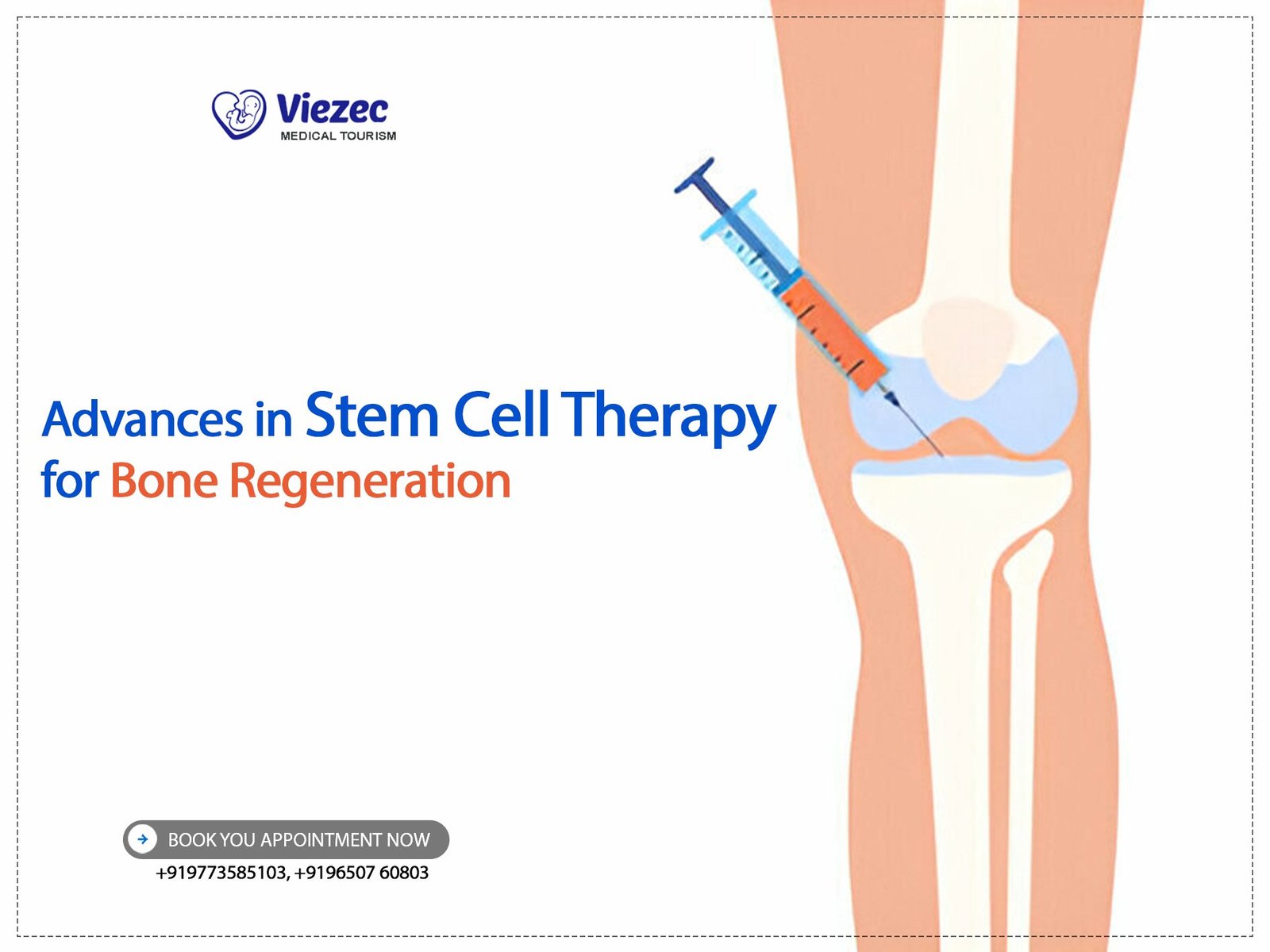
Hematopoietic Stem Cell Transplantation (HSCT)
Hematopoietic stem cell transplantation (HSCT) is one of the most established applications of stem cell therapy in cancer treatment. HSCT involves the transplantation of hematopoietic stem cells, which can differentiate into various blood cell types, to replace damaged or diseased bone marrow. This procedure is commonly used to treat blood cancers, such as leukemia and lymphoma, and has shown significant success in achieving remission and improving survival rates. HSCT can be performed using stem cells from the patient (autologous transplant) or a donor (allogeneic transplant), with each approach having distinct advantages and challenges.
Mesenchymal Stem Cells (MSCs) in Solid Tumors
Mesenchymal stem cells (MSCs) are another promising tool in cancer therapy, particularly for treating solid tumors. MSCs have the ability to migrate to tumor sites and modulate the tumor microenvironment, potentially inhibiting tumor growth and enhancing the effectiveness of other treatments. Additionally, MSCs can be engineered to deliver therapeutic agents directly to tumors, providing targeted treatment with reduced side effects. Although the clinical application of MSCs in solid tumors is still in the early stages, preliminary studies have shown encouraging results, highlighting their potential as a novel cancer treatment modality.
iPSCs and Personalized Cancer Treatment
Induced pluripotent stem cells (iPSCs) have opened new avenues for personalized cancer treatment. By reprogramming a patient’s cells into iPSCs, researchers can generate patient-specific cell lines for studying cancer biology, testing drug responses, and developing customized treatment strategies. This approach allows for the identification of the most effective therapies for individual patients, improving treatment outcomes and minimizing adverse effects. iPSCs also hold promise for developing cancer vaccines and immunotherapies tailored to the unique characteristics of a patient’s tumor.
Combination Therapies Involving Stem Cells
Combination therapies involving stem cells and other treatment modalities, such as chemotherapy, radiation therapy, or immunotherapy, are gaining traction in cancer treatment. Stem cells can enhance the effectiveness of conventional therapies by promoting tissue repair, modulating immune responses, and delivering targeted treatments. Combining stem cell therapy with other treatments may also help overcome resistance to single-agent therapies and improve overall treatment outcomes. Ongoing research is focused on identifying the most effective combinations and optimizing treatment protocols to maximize the benefits of this approach.
Efficacy and Outcomes
Success Rates in Various Cancer Types
The success rates of stem cell therapy in cancer treatment vary depending on the type and stage of cancer, as well as the specific stem cell intervention used. For example, hematopoietic stem cell transplantation (HSCT) has shown high success rates in treating blood cancers, such as leukemia and lymphoma, with many patients achieving long-term remission. In contrast, the application of stem cell therapy in solid tumors is still in the early stages, and more research is needed to determine its effectiveness.
Leukemia and Lymphoma
HSCT has been particularly successful in treating leukemia and lymphoma, with many patients achieving long-term remission and improved survival rates. Allogeneic HSCT, which involves using stem cells from a donor, has shown the highest success rates in these cancers, as it provides a new immune system capable of targeting residual cancer cells. However, autologous HSCT, which uses the patient’s own stem cells, is also effective in certain cases and may have fewer complications.
Breast Cancer
The use of stem cell therapy in breast cancer treatment is still experimental, with ongoing research exploring its potential benefits. Preliminary studies have shown that mesenchymal stem cells (MSCs) can inhibit tumor growth and enhance the effectiveness of chemotherapy, but more research is needed to confirm these findings and determine the optimal treatment protocols.
Lung Cancer
Lung cancer is another area where stem cell therapy is being investigated. Early studies have shown that MSCs can target lung tumors and deliver therapeutic agents directly to the tumor site, potentially improving treatment outcomes. However, clinical trials are needed to evaluate the safety and efficacy of this approach and determine its potential role in lung cancer treatment.
Short-term vs. Long-term Outcomes
Evaluating both short-term and long-term outcomes is essential for assessing the overall effectiveness of stem cell therapy in cancer treatment. Short-term outcomes may include immediate responses to treatment, such as tumor shrinkage or remission, while long-term outcomes focus on survival rates, disease-free intervals, and quality of life improvements. By examining both types of outcomes, researchers can gain a comprehensive understanding of the benefits and limitations of stem cell therapy and identify areas for further improvement.
Quality of Life Improvements
One of the key goals of cancer treatment is to improve patients’ quality of life. Stem cell therapy has the potential to enhance quality of life by promoting tissue repair, reducing treatment-related side effects, and improving overall health. Patient-reported outcomes, such as physical functioning, emotional well-being, and symptom management, provide valuable insights into the impact of stem cell therapy on quality of life and help guide future treatment strategies.
Safety and Ethical Considerations
Potential Risks and Complications
Like all medical treatments, stem cell therapy carries potential risks and complications. It is essential to carefully evaluate these risks to ensure patient safety and optimize treatment protocols.
Graft-Versus-Host Disease (GVHD)
One of the most significant risks associated with allogeneic stem cell transplantation is graft-versus-host disease (GVHD), a condition where the donor’s immune cells attack the recipient’s tissues. GVHD can cause severe and potentially life-threatening complications, affecting the skin, liver, gastrointestinal tract, and other organs. Strategies to prevent and manage GVHD, such as immunosuppressive therapies and donor matching, are critical for improving the safety of allogeneic HSCT.
Tumorigenicity Risks
Another concern with stem cell therapy is the potential for tumorigenicity, or the formation of tumors from transplanted stem cells. This risk is particularly relevant for embryonic stem cells and induced pluripotent stem cells (iPSCs), which have a high proliferative capacity. Ensuring the safety of stem cell therapies requires rigorous screening and quality control measures to minimize the risk of tumor formation and other adverse effects.
Ethical Issues in Stem Cell Research and Therapy
Ethical considerations play a significant role in the development and application of stem cell therapies. Addressing these issues is essential for ensuring the responsible and ethical conduct of research and clinical practice.
Consent and Autonomy
Informed consent is a cornerstone of ethical medical practice, ensuring that patients are fully aware of the potential benefits, risks, and alternatives to stem cell therapy. Respecting patient autonomy involves providing clear and comprehensive information, allowing patients to make informed decisions about their treatment options.
Use of Embryonic Stem Cells
The use of embryonic stem cells (ESCs) in research and therapy raises ethical concerns due to the destruction of embryos. Balancing the potential benefits of ESC-based therapies with ethical considerations requires careful deliberation and adherence to regulatory guidelines. Alternative approaches, such as the use of induced pluripotent stem cells (iPSCs), offer a promising solution by providing pluripotent cells without the ethical issues associated with ESCs.
Comparative Analysis with Conventional Therapies
Chemotherapy vs. Stem Cell Therapy
Chemotherapy is a widely used cancer treatment that involves using drugs to kill rapidly dividing cancer cells. While effective, chemotherapy often has significant side effects, such as hair loss, nausea, and immune suppression. Stem cell therapy offers a potential alternative or complement to chemotherapy by promoting tissue repair and enhancing the body’s immune response. Comparative studies are needed to evaluate the relative effectiveness and side effect profiles of these treatment modalities.
Radiation Therapy vs. Stem Cell Therapy
Radiation therapy uses high-energy radiation to destroy cancer cells, but it can also damage healthy tissues and cause long-term side effects. Stem cell therapy has the potential to mitigate some of these side effects by promoting tissue regeneration and repair. Additionally, stem cells can be engineered to deliver radiation-sensitizing agents directly to tumors, potentially improving the effectiveness of radiation therapy while reducing its harmful effects.
Immunotherapy and Stem Cell Synergy
Immunotherapy, which harnesses the body’s immune system to target cancer cells, has shown promising results in treating various cancers. Combining stem cell therapy with immunotherapy may enhance the overall effectiveness of treatment by boosting the immune response and providing targeted delivery of therapeutic agents. Research into the synergistic effects of these therapies is ongoing, with the goal of developing more effective and personalized cancer treatment strategies.
Cost-Benefit Analysis
Evaluating the cost-effectiveness of stem cell therapy compared to conventional treatments is essential for informing healthcare policy and decision-making. While stem cell therapy may have higher upfront costs, its potential to improve long-term outcomes and reduce the need for ongoing treatments could result in overall cost savings. Cost-benefit analysis considers both the economic and clinical aspects of treatment, providing a comprehensive assessment of its value.
Future Directions and Innovations
Advances in Stem Cell Engineering
Advances in stem cell engineering are driving the development of new and improved cancer therapies. Techniques such as gene editing, tissue engineering, and synthetic biology are being applied to enhance the therapeutic potential of stem cells. These innovations aim to improve the precision and effectiveness of stem cell-based treatments, offering new hope for cancer patients.
Emerging Therapies and Clinical Trials
Emerging stem cell therapies and ongoing clinical trials are exploring novel approaches to cancer treatment. These include the use of engineered stem cells to deliver targeted therapies, the development of cancer vaccines, and the application of stem cell-derived exosomes for tumor modulation. As these therapies progress through clinical trials, they have the potential to revolutionize cancer treatment and improve patient outcomes.
Potential for Personalized Medicine
The potential for personalized medicine is one of the most exciting aspects of stem cell therapy. By developing patient-specific treatments based on individual genetic and cellular profiles, personalized medicine aims to optimize treatment effectiveness and minimize adverse effects. Stem cell technologies, such as iPSCs, play a crucial role in this approach, enabling the development of customized therapies tailored to each patient’s unique needs.
Regulatory and Policy Developments
Regulatory and policy developments are essential for ensuring the safe and ethical application of stem cell therapies. As new treatments emerge, regulatory frameworks must evolve to address the unique challenges and risks associated with stem cell research and clinical practice. Policy developments should also promote equitable access to innovative therapies, ensuring that all patients can benefit from advances in stem cell medicine.
FAQs
What are stem cells and how are they used in cancer therapy?
Stem cells are unique cells capable of differentiating into various cell types and self-renewing. In cancer therapy, they are used to replace damaged tissues, enhance immune responses, and deliver targeted treatments. Hematopoietic stem cell transplantation (HSCT) is a common application, particularly for blood cancers, while mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs) are being explored for solid tumors and personalized medicine.
What are the main risks associated with stem cell therapy for cancer?
The main risks include graft-versus-host disease (GVHD) in allogeneic transplants, where donor immune cells attack the recipient’s tissues, and the potential for tumor formation from transplanted stem cells, especially embryonic stem cells and iPSCs. Ensuring patient safety involves careful screening, donor matching, and monitoring for adverse effects.
How does stem cell therapy compare to conventional cancer treatments?
Stem cell therapy offers potential advantages over conventional treatments, such as promoting tissue repair and reducing side effects. Comparative studies are needed to evaluate its relative effectiveness. Combining stem cell therapy with treatments like chemotherapy, radiation, and immunotherapy may enhance overall outcomes and reduce treatment-related complications.
What is the future of stem cell therapy in cancer treatment?
The future of stem cell therapy in cancer treatment is promising, with advances in stem cell engineering, emerging therapies, and personalized medicine approaches. Ongoing clinical trials and regulatory developments will shape the landscape of stem cell-based treatments, aiming to improve patient outcomes and offer new hope for those battling cancer.
For more information or to stay updated on the latest advancements in stem cell therapy for cancer, visit us online.