Neurological disorders encompass a wide array of conditions that affect the brain, spinal cord, and nerves throughout the body. These disorders can significantly impact an individual’s quality of life, leading to challenges in movement, speech, cognition, and overall functionality. Neurological disorders are broadly classified based on their symptoms, causes, and affected regions. Common examples include Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS), and various forms of neuropathy. The burden of these disorders is substantial, with millions of people affected worldwide, underscoring the urgency for effective treatments.
Definition and Types of Stem Cells
Stem cells are unique cells with the remarkable potential to develop into various cell types in the body. They serve as a repair system, replenishing other cells as long as the organism is alive. There are several types of stem cells, each with distinct capabilities and potential uses in medical research and treatment. The primary types include embryonic stem cells, adult stem cells, and induced pluripotent stem cells (iPSCs). Embryonic stem cells are derived from early-stage embryos and can differentiate into almost any cell type. Adult stem cells, found in various tissues, are more specialized. iPSCs are genetically reprogrammed adult cells that behave like embryonic stem cells.
Importance of Stem Cell Research in Neurology
Stem cell research holds immense promise for neurology, offering potential cures and treatments for various neurological disorders that currently have limited options. The ability of stem cells to differentiate into specialized cells opens avenues for regenerating damaged tissues, replacing lost neurons, and modulating immune responses. Research in this field aims to develop innovative therapies that can slow disease progression, alleviate symptoms, and ultimately restore neurological function. The advances in stem cell technology are gradually translating into clinical applications, bringing hope to millions of patients suffering from debilitating neurological conditions.
Understanding Neurological Disorders
Common Neurological Disorders
Alzheimer’s Disease
Alzheimer’s disease is a progressive neurodegenerative disorder characterized by memory loss, cognitive decline, and behavioral changes. It primarily affects older adults and is the most common cause of dementia. The disease involves the accumulation of amyloid plaques and neurofibrillary tangles in the brain, leading to neuronal damage and loss. Currently, there is no cure for Alzheimer’s, and available treatments only provide symptomatic relief, highlighting the need for new therapeutic strategies.
Parkinson’s Disease
Parkinson’s disease is a chronic, progressive movement disorder resulting from the degeneration of dopamine-producing neurons in the brain. Symptoms include tremors, rigidity, bradykinesia (slowness of movement), and postural instability. The exact cause of Parkinson’s disease remains unknown, though genetic and environmental factors are believed to play a role. Treatments primarily focus on managing symptoms through medication and, in some cases, surgical interventions like deep brain stimulation.
Multiple Sclerosis
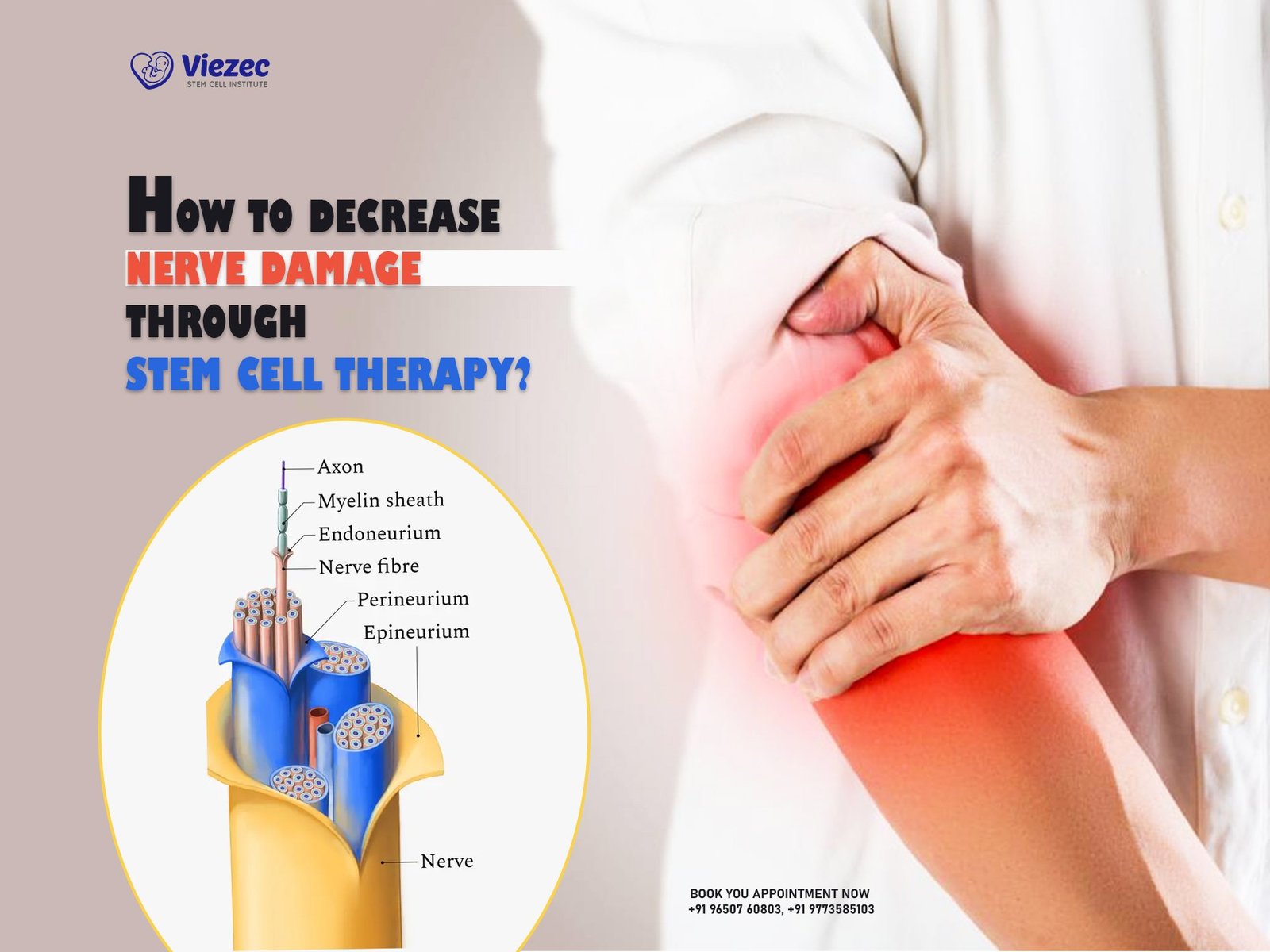
Multiple sclerosis (MS) is an autoimmune disorder where the immune system attacks the protective myelin sheath covering nerve fibers, causing communication problems between the brain and the rest of the body. Symptoms can vary widely and include fatigue, difficulty walking, numbness, and cognitive issues. MS can be relapsing-remitting or progressive, and while several treatments exist to manage symptoms and modify disease progression, a cure remains elusive.
Causes and Symptoms
Neurological disorders can arise from a variety of causes, including genetic mutations, environmental factors, infections, traumatic injuries, and autoimmune reactions. Symptoms vary depending on the specific disorder and the affected regions of the nervous system. Common symptoms include memory loss, muscle weakness, coordination problems, pain, seizures, and cognitive deficits. Understanding the underlying causes and symptomatology is crucial for developing targeted treatments and improving patient outcomes.
Current Treatment Limitations
Despite advances in medical research, current treatments for many neurological disorders are limited in their efficacy. Most therapies focus on managing symptoms rather than addressing the root causes of the diseases. For conditions like Alzheimer’s and Parkinson’s, available treatments can only temporarily alleviate symptoms and do not halt disease progression. This highlights the urgent need for innovative approaches, such as stem cell therapy, which hold the potential to offer more effective and long-lasting solutions.
Stem Cell Basics
Types of Stem Cells
Embryonic Stem Cells
Embryonic stem cells (ESCs) are derived from early-stage embryos and possess the ability to develop into nearly any cell type in the body. This pluripotency makes them incredibly valuable for research and potential therapeutic applications. However, the use of ESCs raises ethical concerns due to the destruction of embryos, prompting the exploration of alternative stem cell sources.
Adult Stem Cells
Adult stem cells, also known as somatic or tissue-specific stem cells, are found in various tissues throughout the body. Unlike ESCs, they are multipotent, meaning they can differentiate into a limited range of cell types related to their tissue of origin. Adult stem cells are crucial for tissue repair and regeneration and are less controversial than embryonic stem cells.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs) are adult cells that have been genetically reprogrammed to an embryonic stem cell-like state. They offer a promising alternative to ESCs, as they do not involve the destruction of embryos and can be derived from a patient’s own cells, reducing the risk of immune rejection. iPSCs hold significant potential for personalized medicine and regenerative therapies.
Properties of Stem Cells
Stem cells are characterized by their unique properties, including self-renewal and the ability to differentiate into specialized cell types. Self-renewal allows stem cells to divide and produce more stem cells, maintaining their population over time. Differentiation enables them to develop into specific cell types, such as neurons, muscle cells, or blood cells, under certain conditions. These properties make stem cells invaluable for regenerative medicine and tissue engineering.
Stem Cell Differentiation
Stem cell differentiation is the process by which unspecialized stem cells develop into specialized cells with distinct functions. This process is regulated by various signals and factors within the cellular environment, including growth factors, cytokines, and extracellular matrix components. Understanding the mechanisms of differentiation is crucial for directing stem cells to form specific cell types needed for therapeutic applications, such as replacing damaged neurons in neurological disorders.
Mechanisms of Stem Cell Therapy
How Stem Cells Work
Stem cell therapy aims to harness the regenerative potential of stem cells to repair or replace damaged tissues. In neurological disorders, this involves differentiating stem cells into specific neuronal types and transplanting them into the affected areas of the brain or spinal cord. Stem cells can promote tissue repair by replacing lost or damaged cells, secreting neuroprotective factors, and modulating the immune response to reduce inflammation.
Stem Cell Delivery Methods
Intravenous Injection
Intravenous injection is a non-invasive method of delivering stem cells into the bloodstream. This approach allows stem cells to migrate to the site of injury or disease through the circulatory system. However, the efficiency of homing to specific tissues can be limited, and there is a risk of cells being trapped in other organs, such as the lungs or liver.
Direct Neural Injection
Direct neural injection involves delivering stem cells directly into the brain or spinal cord. This method ensures that a high concentration of cells reaches the targeted area, potentially enhancing therapeutic efficacy. However, it is more invasive and carries risks associated with surgical procedures, such as infection or damage to surrounding tissues.
Scaffold-based Delivery
Scaffold-based delivery uses biocompatible materials to create a supportive structure for stem cells, enhancing their survival, integration, and function in the host tissue. Scaffolds can provide physical support, promote cell adhesion, and deliver bioactive molecules that guide stem cell differentiation and tissue regeneration. This method is particularly useful for repairing large or complex tissue defects.
Challenges in Stem Cell Therapy
Stem cell therapy faces several challenges, including ensuring the survival, integration, and functional differentiation of transplanted cells. There are also risks of immune rejection, tumor formation, and ethical concerns, particularly with the use of embryonic stem cells. Additionally, scaling up production and ensuring the consistency and quality of stem cell preparations for clinical use are significant hurdles. Addressing these challenges is essential for the successful translation of stem cell therapies from the laboratory to clinical practice.
Stem Cell Research and Alzheimer’s Disease
Pathophysiology of Alzheimer’s Disease
Alzheimer’s disease is characterized by the accumulation of amyloid-beta plaques and tau tangles in the brain, leading to neuronal death and brain atrophy. The exact mechanisms underlying these pathological changes remain unclear, but they involve a combination of genetic, environmental, and lifestyle factors. The progressive loss of neurons and synapses impairs cognitive function, memory, and behavior, ultimately resulting in severe dementia.
Stem Cell Treatment Approaches
Neuronal Replacement
One approach to treating Alzheimer’s disease with stem cells involves replacing lost neurons. By differentiating stem cells into cholinergic neurons, which are particularly affected in Alzheimer’s, it is possible to restore neuronal populations and improve cognitive function. These cells can be transplanted into the brain to integrate with existing neural networks and compensate for lost function.
Neuroprotection
Stem cells can also provide neuroprotection by secreting growth factors, cytokines, and other molecules that support neuronal survival and function. These factors can help reduce inflammation, prevent further neuronal loss, and promote the repair of damaged tissues. This approach aims to slow disease progression and maintain cognitive function for a longer period.
Clinical Trials and Outcomes
Clinical trials investigating stem cell therapies for Alzheimer’s disease are ongoing, with some promising results. Early-phase trials have demonstrated the safety and feasibility of stem cell transplantation, with some studies showing improvements in cognitive function and brain metabolism. However, more extensive research is needed to confirm these findings and determine the long-term efficacy and safety of stem cell treatments for Alzheimer’s disease.
Stem Cell Research and Parkinson’s Disease
Pathophysiology of Parkinson’s Disease
Parkinson’s disease is characterized by the degeneration of dopaminergic neurons in the substantia nigra, a region of the brain involved in movement control. The loss of these neurons leads to a deficiency of dopamine, a neurotransmitter essential for coordinating movement. The exact cause of neuronal death is not fully understood, but it likely involves a combination of genetic mutations, environmental toxins, and cellular dysfunction.
Stem Cell Treatment Approaches
Dopaminergic Neuron Replacement
Stem cell therapy for Parkinson’s disease focuses on replacing the lost dopaminergic neurons. By differentiating stem cells into dopaminergic neurons and transplanting them into the brain, it is possible to restore dopamine levels and improve motor function. This approach aims to directly address the underlying cause of Parkinson’s and provide long-lasting relief from symptoms.
Disease-modifying Strategies
In addition to neuronal replacement, stem cells can be used to develop disease-modifying strategies that slow the progression of Parkinson’s disease. This includes using stem cells to deliver neuroprotective factors, modulate the immune response, and promote the survival and function of existing neurons. These strategies aim to preserve neural networks and maintain motor function over time.
Clinical Trials and Outcomes
Several clinical trials are exploring the potential of stem cell therapies for Parkinson’s disease. Early-phase trials have demonstrated the safety and feasibility of transplanting stem cell-derived dopaminergic neurons, with some studies reporting improvements in motor function. Ongoing research aims to optimize cell differentiation protocols, delivery methods, and patient selection to enhance therapeutic outcomes and minimize risks.
Stem Cell Research and Multiple Sclerosis
Pathophysiology of Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disorder where the immune system attacks the myelin sheath, the protective covering of nerve fibers. This leads to demyelination, inflammation, and subsequent neuronal damage, disrupting communication between the brain and the rest of the body. The exact cause of MS is unknown, but it involves a combination of genetic predisposition and environmental triggers.
Stem Cell Treatment Approaches
Remyelination Strategies
One approach to treating MS with stem cells involves promoting remyelination, the process of restoring the damaged myelin sheath. Stem cells can differentiate into oligodendrocytes, the cells responsible for producing myelin, and be transplanted into the affected areas to repair the damaged myelin and restore nerve function.
Immune Modulation
Stem cells can also modulate the immune response, reducing the autoimmune attack on myelin and preventing further damage. This involves using stem cells to reset the immune system or deliver immunomodulatory factors that suppress the inflammatory response. These strategies aim to halt disease progression and promote recovery.
Clinical Trials and Outcomes
Clinical trials investigating stem cell therapies for MS are ongoing, with some studies showing promising results. Early-phase trials have demonstrated the safety and feasibility of using stem cells to promote remyelination and modulate the immune response. Some patients have experienced improvements in mobility, fatigue, and other symptoms, suggesting the potential of stem cell therapies to provide meaningful benefits for individuals with MS.
Emerging Stem Cell Therapies for Other Neurological Disorders
Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder that affects motor neurons, leading to muscle weakness, paralysis, and eventual respiratory failure. Stem cell therapy for ALS aims to replace lost motor neurons, provide neuroprotection, and modulate the immune response. Clinical trials are exploring various approaches, including the transplantation of neural stem cells and the use of iPSCs to generate motor neurons for transplantation.
Spinal Cord Injuries
Spinal cord injuries can result in permanent paralysis and loss of sensory and motor function. Stem cell therapy holds promise for repairing spinal cord injuries by promoting the regeneration of damaged neurons, supporting axonal growth, and creating a favorable environment for tissue repair. Various approaches, including the use of neural stem cells and scaffold-based delivery, are being investigated in clinical trials.
Stroke
Stroke is a leading cause of disability and death, resulting from the interruption of blood flow to the brain. Stem cell therapy for stroke aims to repair damaged brain tissue, enhance neurogenesis, and improve functional recovery. Clinical trials are exploring the use of various types of stem cells, including mesenchymal stem cells and iPSCs, to promote tissue repair and restore neurological function in stroke patients.
Ethical and Regulatory Considerations
Ethical Issues in Stem Cell Research
Use of Embryonic Stem Cells
The use of embryonic stem cells (ESCs) in research raises ethical concerns due to the destruction of embryos. This has led to debates about the moral status of embryos and the ethics of using ESCs for medical research and treatment. Alternatives, such as iPSCs, offer a less controversial option, but the ethical considerations surrounding ESCs continue to influence regulatory policies and public opinion.
Informed Consent
Informed consent is a critical ethical consideration in stem cell research and therapy. Patients and donors must be fully informed about the risks, benefits, and potential outcomes of participating in stem cell studies or receiving stem cell treatments. Ensuring that consent is obtained ethically and transparently is essential for protecting the rights and autonomy of participants.
Regulatory Frameworks
International Guidelines
The development and application of stem cell therapies are governed by various regulatory frameworks to ensure safety, efficacy, and ethical conduct. International guidelines, such as those established by the International Society for Stem Cell Research (ISSCR), provide standards for the ethical conduct of stem cell research, clinical trials, and the commercialization of stem cell products. These guidelines aim to promote responsible research and protect patient welfare.
FAQs
1. What are the main types of stem cells used in treating neurological disorders?
The primary types of stem cells used in treating neurological disorders are embryonic stem cells, adult stem cells, and induced pluripotent stem cells (iPSCs). Each type has unique properties and potential applications in regenerative medicine and therapy.
2. How do stem cells help in treating Alzheimer’s disease?
Stem cells can help treat Alzheimer’s disease by replacing lost neurons, providing neuroprotection through the secretion of growth factors, and modulating the immune response to reduce inflammation and prevent further neuronal damage.
3. What are the challenges in using stem cell therapy for Parkinson’s disease?
Challenges in using stem cell therapy for Parkinson’s disease include ensuring the survival and integration of transplanted cells, preventing immune rejection, and optimizing delivery methods to enhance therapeutic efficacy while minimizing risks.
4. Can stem cell therapy cure multiple sclerosis?
While stem cell therapy cannot currently cure multiple sclerosis, it holds potential to significantly modify the disease by promoting remyelination, reducing inflammation, and supporting the repair of damaged tissues, thereby improving patient outcomes.
5. What ethical issues are associated with stem cell research?
Ethical issues in stem cell research include the use of embryonic stem cells, which involves the destruction of embryos, and ensuring informed consent from participants. These concerns influence regulatory policies and public perception of stem cell research.