Hypothyroidism—where the thyroid gland produces insufficient hormones—affects millions of people globally and in India. Conventional treatments (such as hormone replacement) help manage it, but many patients seek therapies that go beyond symptom-control to address underlying thyroid tissue damage.
In this context, regenerative medicine and stem cell-based therapies are gaining interest. This article explores the science, current status, benefits & risks, and how patients in India should approach the possibility of stem cell treatment for hypothyroidism.
Understanding Hypothyroidism & Its Challenges
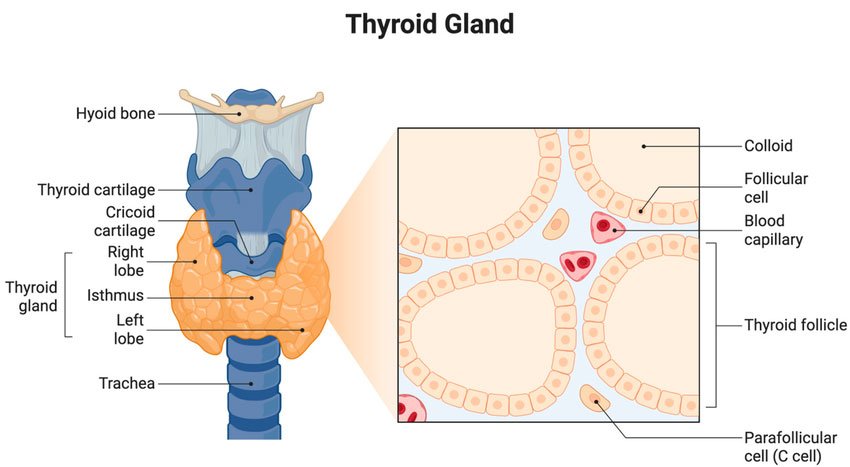
The thyroid gland regulates metabolism, energy, temperature and many bodily functions through hormones (T₃ and T₄). When under-active, symptoms may include fatigue, weight gain, cold sensitivity, hair loss and slowed metabolism.
In India, autoimmune thyroiditis (such as Hashimoto’s thyroiditis) is a common cause, along with post-surgical removal of thyroid, radioactive iodine therapy, or congenital/iodine deficiency reasons.
Current standard of care: typically Levothyroxine (T₄ replacement) and in some cases combination therapy. Clinical reviews show that while hormonal levels can be normalized, some patients remain symptomatic. PMC+2PMC+2
Key challenge: Conventional therapy manages hormone levels—it does not regenerate lost thyroid tissue or always fully restore normal thyroid architecture or immune regulation.
What is Stem Cell Therapy & How Might It Apply to the Thyroid
Stem cell therapy is a form of regenerative medicine that uses special cells capable of developing into different cell types to repair or replace damaged tissues in the body. These cells—such as mesenchymal stem cells (MSCs) or induced pluripotent stem cells (iPSCs)—can self-renew and transform into specialized cells like thyroid follicular cells, which are responsible for producing thyroid hormones.
Stem cell therapy focuses on repairing and regenerating damaged tissues rather than only compensating for lost function through external hormones.
Possible Therapeutic Actions:
-
Regeneration of Thyroid Follicular Cells
– Stem cells (particularly mesenchymal or induced pluripotent stem cells) may differentiate into thyroid-like cells capable of producing T3 and T4 hormones naturally.
– This could, in theory, reduce or even replace the need for lifelong hormone replacement. -
Immune Modulation in Hashimoto’s Disease
– In autoimmune hypothyroidism, the body’s immune system attacks its own thyroid tissue.
– Stem cells may modulate immune response and reduce chronic inflammation, helping preserve any remaining healthy thyroid cells. -
Microenvironment Restoration
– Stem cells can promote better blood supply, repair damaged tissue architecture, and reduce oxidative stress within the thyroid gland—creating a healthier environment for recovery. -
Reduction in Fibrosis and Inflammation
– Studies in animal models show that stem cells can reduce tissue fibrosis (hardening/scarring), allowing thyroid tissue to recover partial function.
Scientific Note: Current findings mostly come from preclinical (animal) and in vitro (lab-based) research. Human clinical data are limited but growing gradually through global trials.
What Does This Mean for Patients with Hypothyroidism?
Stem cell therapy for hypothyroidism is an emerging area in regenerative medicine. For patients, this means a potential future pathway that goes beyond just managing thyroid hormone levels—it aims to restore the thyroid gland’s ability to function naturally. However, it’s equally important to understand that this therapy is still under study, and its clinical use is in the experimental or investigational stage.
Below is a comprehensive, transparent breakdown for patients exploring this innovative treatment option.
Who Might Be a Candidate for Stem Cell Therapy?
While stem cell therapy for hypothyroidism is not yet a mainstream medical procedure, certain patients might be considered for future trials or compassionate use, depending on their medical condition and response to conventional treatment. Possible candidates may include:
-
Patients with persistent symptoms (fatigue, hair loss, weight gain, sluggish metabolism) despite taking thyroid hormone replacement regularly.
-
Individuals with autoimmune thyroiditis (Hashimoto’s Disease) where the immune system attacks the thyroid, leading to tissue destruction.
-
Post-surgical hypothyroidism cases (after thyroidectomy) or those who received radioactive iodine therapy.
-
Patients with thyroid tissue damage due to chronic inflammation or fibrosis, where regeneration could be beneficial.
-
People seeking advanced, regenerative options after standard endocrinology treatment has plateaued in its effectiveness.
Important: Every patient must first undergo a detailed endocrinology consultation, thyroid function test (TSH, T3, T4), ultrasound evaluation, and autoimmune antibody tests to determine eligibility and baseline health.
What Patients Should Expect — Setting Realistic Goals
It’s essential to maintain balanced expectations about what stem cell therapy can and cannot do right now.
| Expectation | What It Means in Reality |
|---|---|
| 🧩 “Stem cells will cure my hypothyroidism.” | The therapy is experimental. It may offer improvement or partial restoration, but no guaranteed cure yet exists. |
| ⚖️ “I might be able to reduce my thyroid medication.” | Possible in future studies or specific cases, but you must continue your prescribed medication unless advised by a qualified endocrinologist. |
| ⏳ “Results happen quickly.” | Regeneration takes time — any improvements, if they occur, may take months to evaluate via lab tests and imaging. |
| 💰 “The treatment is affordable.” | Costs can vary widely depending on cell source, protocol complexity, and follow-up needs. Always request transparent pricing and avoid unverified claims. |
Tip: Choose clinics that offer written protocols, informed consent documents, and post-treatment follow-up schedules. Transparency equals trust.
Questions Every Patient Should Ask Before Considering Treatment
Before moving ahead with any stem cell program for hypothyroidism—especially in India or abroad—ask the following critical questions:
-
What is the scientific evidence supporting this treatment?
→ Are there published peer-reviewed studies or ongoing clinical trials? -
What kind of stem cells are used?
→ Autologous (from your own body) or allogeneic (from a donor)? MSCs or iPSCs? -
Is the procedure approved or under regulatory supervision?
→ Check if it’s compliant with ICMR (Indian Council of Medical Research) or other ethical guidelines. -
Who are the treating specialists?
→ The team should include endocrinologists, regenerative medicine specialists, and lab scientists. -
What are the potential risks and side effects?
→ Understand both short-term (infection, inflammation) and long-term (cell misdifferentiation) risks. -
What follow-up plan is provided?
→ A credible centre should monitor hormone levels, thyroid imaging, and general wellness for several months after therapy.
Potential Benefits — What Some Early Evidence Suggests
Though the therapy is still in development, early experimental research shows several encouraging findings:
-
Stem cells have shown potential to regenerate thyroid tissue in animal models with hypothyroidism.
-
Inflammatory markers decreased in studies where mesenchymal stem cells were used to treat autoimmune thyroiditis.
-
Stem cell–derived thyroid organoids were able to produce T3 and T4 hormones under lab conditions.
-
Improved thyroid function and reduced fibrosis have been noted in pre-clinical reports.
These outcomes are not yet proven in large-scale human clinical trials, but they lay the scientific groundwork for future therapies.
Mesenchymal Stem Cells for Hypothyroidism
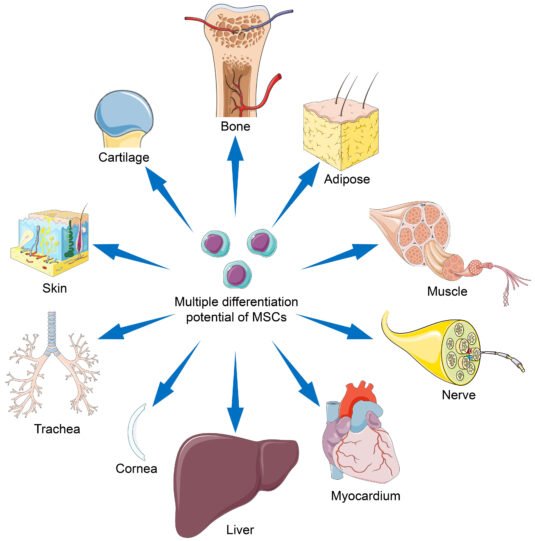
Mesenchymal stem cells (MSCs) are multipotent stromal cells capable of differentiating into a variety of tissue types and modulating immune responses. In the context of hypothyroidism, MSCs have generated significant interest because they offer a regenerative approach that goes beyond traditional hormone replacement therapy. Unlike conventional treatments that manage symptoms by supplying synthetic hormones, MSCs aim to repair or regenerate damaged thyroid tissue, addressing the root cause of the disorder.
Mechanism of Action: Regeneration and Immune Modulation
MSCs may support thyroid recovery through two main mechanisms:
-
Tissue Regeneration: MSCs can differentiate into thyroid-like cells or promote the repair of existing thyroid follicles, potentially restoring the gland’s natural hormone-producing capacity.
-
Immunomodulation: In autoimmune hypothyroidism, such as Hashimoto’s thyroiditis, MSCs have the ability to regulate immune system activity, reducing inflammation and limiting further thyroid tissue destruction. Preclinical studies suggest that this dual action may help improve thyroid function over time.
Clinical Potential and Current Research
While MSC therapy for hypothyroidism remains largely experimental, early research and animal studies are promising. Transplantation of MSCs in preclinical models has shown improvements in thyroid tissue structure, hormone levels, and inflammatory markers. Human clinical trials are still limited, but initial investigations indicate that MSC therapy could potentially reduce dependence on lifelong hormone replacement and improve overall quality of life for selected patients. In India, regulated stem cell clinics like Viezec focus on providing MSC therapy under strict ethical and safety protocols, ensuring patients benefit from advanced regenerative techniques while minimizing risks.
Comparison: Stem Cell Therapy vs Conventional Thyroid Treatment
| Aspect | Conventional Thyroid Treatment | Stem Cell Therapy (Regenerative) |
|---|---|---|
| Primary goal | Replace missing thyroid hormone to relieve symptoms and normalize labs | Repair/regenerate thyroid tissue and/or modulate immune response to reduce dependency on replacement |
| Scientific maturity | Established, guideline-driven, decades of safety data | Emerging; mostly preclinical and early-phase human studies for thyroid applications |
| Typical intervention | Daily oral levothyroxine (sometimes liothyronine) | One or more cell infusions/injections (MSCs, iPSC-derived cells, etc.) in clinical/research settings |
| Regulatory status | Widely approved, standard of care globally | Largely experimental for thyroid disease — requires clinical trial/regulated program |
| Efficacy (typical) | High for normalizing TSH and preventing complications; symptom improvement variable | Variable and not proven consistently in large human trials; potential for reduced medication needs or improved tissue function in some cases |
| Safety profile | Well-characterized; rare side effects when dosed correctly | Short-term safety in some cell therapies acceptable; long-term safety and risks (e.g., ectopic growth, immune reactions) under study |
| Monitoring needed | Routine TSH/T4 checks and clinical review | Intensive baseline and longitudinal monitoring (hormones, imaging, immune markers, safety labs) |
| Cost | Low ongoing cost (medication) | High upfront costs; multiple procedures and follow-ups possible |
| Accessibility | Globally available, including primary care | Limited to specialized/regenerative centres and clinical trials |
| Who it may suit | Most patients with primary hypothyroidism | Selected patients seeking alternatives, those with tissue loss, or participating in research with informed consent |

As a Stem Cell Service Provider in India: Our Approach & Message
At Viezec, we understand that choosing a regenerative treatment for hypothyroidism—or any chronic condition—is a deeply personal decision. Our goal is to guide patients with transparency, evidence-based information, and ethical medical care.
As a responsible stem cell service provider in India, we follow a structured, patient-centric approach that ensures every individual receives not only advanced treatment options but also trustworthy scientific guidance.
Our Philosophy: Science, Safety & Transparency
Stem cell therapy represents the frontier of modern regenerative medicine, but not every innovation is automatically ready for widespread clinical use.
At Viezec, we firmly believe in a balanced approach—offering access to cutting-edge regenerative techniques while maintaining full compliance with Indian biomedical guidelines and international ethical standards.
Our guiding principles include:
-
Scientific integrity: We rely on peer-reviewed research, verified protocols, and evidence-based practices.
-
Transparency: Every patient receives a full explanation of the treatment protocol, expected benefits, limitations, and potential risks.
-
Patient safety first: We only use certified laboratories and adhere to ICMR and CDSCO recommendations for cell-based therapies.
-
Ethical care: We never claim “miracle cures.” Instead, we educate patients about what regenerative medicine can and cannot achieve.
Our mission is to make regenerative therapy accessible, affordable, and scientifically sound for patients in India and worldwide.
Our Expertise & Treatment Protocols
Viezec’s medical and research teams include specialists in regenerative medicine, endocrinology, and cellular biology.
For hypothyroidism and autoimmune thyroiditis cases, we employ protocols that focus on both tissue repair and immune modulation.
Our core methodology includes:
-
Personalized assessment: Each patient undergoes comprehensive medical evaluation including thyroid function tests (TSH, T3, T4), autoimmune antibody markers, and general health screening.
-
Stem cell source selection: Depending on indication and patient suitability, we use ethically sourced mesenchymal stem cells (MSCs) derived from umbilical cord, bone marrow, or adipose tissue.
-
Processing in GMP-certified labs: Cells are processed in sterile, government-registered facilities to ensure purity, viability, and safety.
-
Delivery method: Administered through intravenous infusion or targeted injections (based on the clinical need and physician’s decision).
-
Monitoring & follow-up: Hormonal levels, immune markers, and symptom tracking are done at regular intervals post-therapy.
Every treatment plan is reviewed by our internal ethics and clinical advisory board before implementation.
Patient Education and Support
We believe informed patients make safer, smarter decisions.
That’s why we make sure every individual understands both the potential and limitations of stem cell therapy before beginning treatment.
Our education process includes:
-
Free pre-treatment consultations to explain the science and process.
-
Written consent forms clearly outlining benefits, risks, and alternatives.
-
Continuous guidance from a dedicated care coordinator throughout the therapy journey.
-
Transparent cost estimates and payment options (no hidden charges).
-
Educational resources via blogs, FAQs, and one-to-one sessions to help patients understand regenerative medicine in simple terms.
Compliance, Quality & Ethical Standards
In India, stem cell therapy is regulated under the Indian Council of Medical Research (ICMR) and Central Drugs Standard Control Organization (CDSCO) guidelines.
Viezec ensures that every protocol aligns with these frameworks and international Good Manufacturing Practices (GMP).
Our ethical commitments include:
-
Using only ethically sourced, non-embryonic stem cells.
-
Following all ICMR recommendations and maintaining complete patient documentation.
-
Ensuring cell viability, sterility, and traceability through batch-wise testing.
-
Maintaining confidentiality of patient data as per HIPAA and Indian IT regulations.
-
Transparent reporting of outcomes—both positive and limited—to promote scientific honesty.
Why Choose India for Stem Cell Therapy
India has rapidly become a global destination for regenerative medicine, offering world-class expertise at a fraction of Western costs.
At Viezec, international and Indian patients alike choose us because of our:
-
Highly experienced clinical teams and biomedical scientists
-
Advanced laboratory infrastructure meeting GMP and ISO standards
-
Affordable, ethical, and transparent medical services
-
Personalized care plans adapted to Indian and global health needs
-
Seamless tele-consultation and patient coordination for overseas clients
Our location in India allows us to combine affordability with excellence—making cutting-edge regenerative solutions accessible without compromising safety or scientific integrity.
Conclusion
Stem cell therapy, particularly using mesenchymal stem cells (MSCs), represents an exciting frontier in the management of hypothyroidism. Unlike conventional hormone replacement, which primarily addresses symptoms, MSC therapy holds the potential to regenerate damaged thyroid tissue and modulate autoimmune responses, offering a more holistic approach to thyroid health. While current research is promising, it remains largely experimental, and outcomes can vary between patients.
For individuals in India seeking advanced regenerative care, partnering with a regulated, certified stem cell center like Viezec ensures that treatments are performed safely, ethically, and under expert supervision. Patients are encouraged to combine medical guidance, ongoing monitoring, and realistic expectations when exploring MSC therapy. By staying informed and consulting with qualified specialists, hypothyroid patients can make empowered decisions about integrating regenerative medicine into their long-term thyroid care plan.
FAQs
Can Hypothyroidism Be Cured with Stem Cell Treatments?
Stem cell therapy is currently considered investigational for hypothyroidism. While preclinical studies and early research show promise in regenerating thyroid tissue and reducing autoimmune inflammation, there is no guaranteed cure at this time. Patients may experience improved thyroid function or reduced dependency on hormone replacement, but outcomes vary, and long-term efficacy in humans is still under study.
How do stem cells work for hypothyroidism treatment?
Stem cells, particularly mesenchymal stem cells (MSCs), can help in two ways:
-
Regeneration: They may differentiate into thyroid-like cells or promote repair of damaged thyroid follicles.
-
Immunomodulation: They can reduce autoimmune activity, particularly in conditions like Hashimoto’s thyroiditis, protecting remaining thyroid tissue and creating a favorable environment for tissue repair.
What is Stem Cell Therapy and How Can It Help Thyroid Patients?
Stem cell therapy involves harvesting multipotent cells from sources like bone marrow, adipose tissue, or umbilical cord, processing them under controlled laboratory conditions, and delivering them to the patient. For thyroid patients, this therapy aims to support natural hormone production, repair thyroid tissue, and modulate autoimmune attacks, offering a potential complement to conventional hormone replacement.
Who is eligible for stem cell therapy for hypothyroidism?
Eligibility typically includes patients whose hypothyroidism is not fully managed by conventional treatment, those with significant thyroid tissue loss (post-surgery or radioactive therapy), or patients willing to participate in investigational and regulated protocols. Each candidate undergoes a thorough medical evaluation to determine suitability.
Are there any risks associated with stem cell therapy for hypothyroidism?
Yes, while generally considered safe under regulated conditions, potential risks include mild infusion reactions, fever, local discomfort, or immune reactions. Long-term risks, such as abnormal tissue growth, are still under study. Safety depends on the stem cell source, clinical protocol, and laboratory standards.
How long does it take to see results from stem cell therapy?
Improvement in thyroid function or symptoms is often gradual. Some patients may notice changes in 3–6 months, while full regenerative effects may take longer. Continuous monitoring of hormone levels and immune markers is essential to assess response.
How does stem cell therapy compare to conventional hormone replacement therapy?
Conventional therapy, such as levothyroxine, effectively manages symptoms and normalizes hormone levels but does not repair thyroid tissue or modulate autoimmune damage. Stem cell therapy aims to regenerate tissue and improve immune balance but remains experimental, with outcomes that vary between patients.
Is stem cell therapy for hypothyroidism available in India?
Yes, regulated stem cell centers in India, such as Viezec, offer MSC therapy under ethical and certified clinical protocols. Patients can access advanced regenerative medicine with expert supervision, strict safety standards, and comprehensive post-treatment monitoring. However, therapy is offered as investigational, not as a guaranteed cure.