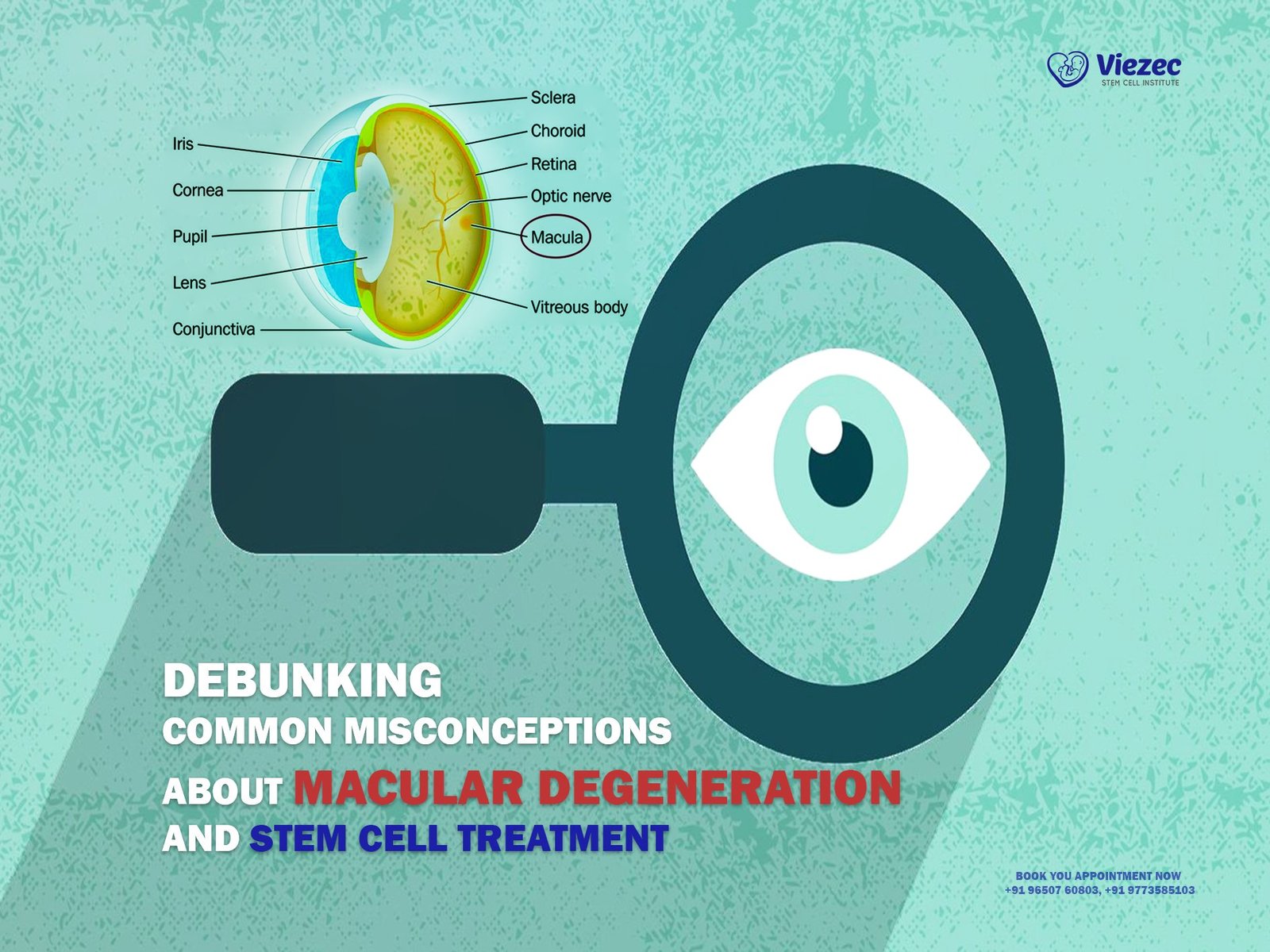
Macular degeneration is a medical condition that affects the central part of the retina, known as the macula, leading to vision loss. It primarily impacts central vision, which is crucial for activities such as reading, driving, and recognizing faces. There are two main types of macular degeneration: dry (atrophic) and wet (neovascular or exudative). Dry macular degeneration is more common and progresses slowly, characterized by the thinning of the macula. Wet macular degeneration, though less common, is more severe and rapid, caused by abnormal blood vessels growing under the retina and leaking fluid or blood. Understanding these distinctions is vital for diagnosis and treatment.
Prevalence and Risk Factors
Macular degeneration is a leading cause of vision loss, particularly in individuals over 50. Its prevalence increases with age, affecting millions worldwide. Risk factors include age, genetics, smoking, hypertension, and prolonged exposure to ultraviolet light. Caucasians are more prone to develop this condition compared to other ethnic groups. Family history also plays a significant role; individuals with immediate family members who have macular degeneration are at higher risk. Additionally, poor diet, obesity, and sedentary lifestyle can contribute to the development of this disease. Recognizing these risk factors helps in preventive strategies and early intervention.
Importance of Early Detection
Symptoms and Warning Signs
Early detection of macular degeneration is crucial for effective management. Symptoms include blurred vision, difficulty reading, seeing straight lines as wavy or distorted, and dark or empty areas in the center of vision. Patients may also experience a decrease in the intensity or brightness of colors. These warning signs often start subtly and may be mistaken for regular aging vision issues, which underscores the importance of regular eye examinations, particularly for individuals over 50 or those with a family history of the disease.
Diagnostic Tools and Tests
Diagnosing macular degeneration involves a comprehensive eye examination by an ophthalmologist. Key diagnostic tools include optical coherence tomography (OCT), which provides detailed images of the retina, and fluorescein angiography, which highlights blood vessels in the retina. Amsler grid tests can also detect visual distortions indicative of macular degeneration. Early detection through these tests allows for timely intervention, potentially slowing the progression of the disease and preserving vision for longer periods.
Goals of the Program
Prevention Strategies
The primary goal of The Ultimate Macular Degeneration Program is to prevent the onset and progression of the disease. This includes promoting a healthy lifestyle with a balanced diet rich in essential nutrients for eye health, encouraging regular physical activity, and advocating for smoking cessation. Public education on the importance of UV protection and routine eye check-ups is also emphasized. By addressing modifiable risk factors, the program aims to reduce the incidence of macular degeneration and improve the quality of life for those at risk.
Treatment and Management Options
For individuals already diagnosed with macular degeneration, the program offers comprehensive treatment and management strategies. This includes pharmaceutical interventions, such as anti-VEGF injections, and surgical options like laser therapy and photodynamic therapy. Emerging treatments, including gene therapy and stem cell research, are also explored. Additionally, the program provides guidance on vision aids and rehabilitation services to help patients maintain independence and improve their daily functioning despite vision loss.
Nutrition and Diet for Eye Health
Essential Nutrients for Vision
Vitamins and Minerals
Proper nutrition plays a pivotal role in maintaining eye health and preventing macular degeneration. Essential vitamins such as A, C, and E, along with minerals like zinc and copper, are crucial for maintaining healthy retinal function. Vitamin A helps in the formation of rhodopsin, a pigment essential for vision in low-light conditions. Vitamin C and E act as antioxidants, protecting the eyes from oxidative stress. Zinc supports the immune system and is vital for the functioning of over 300 enzymes, including those involved in eye health. Including these nutrients in the diet can significantly reduce the risk of developing macular degeneration.
Antioxidants and Omega-3 Fatty Acids
Antioxidants and omega-3 fatty acids are vital in combating inflammation and oxidative stress, which contribute to macular degeneration. Lutein and zeaxanthin are antioxidants found in high concentrations in the macula and help filter harmful blue light. Omega-3 fatty acids, particularly DHA and EPA found in fish oil, support retinal health and reduce the risk of progression from dry to wet macular degeneration. Incorporating foods rich in these nutrients can aid in preserving vision and slowing disease progression.
Dietary Recommendations
Foods to Include
A diet rich in leafy greens, colorful fruits, and vegetables, nuts, seeds, and fish can provide the necessary nutrients to support eye health. Foods like spinach, kale, and collard greens are high in lutein and zeaxanthin. Berries, citrus fruits, and bell peppers are excellent sources of vitamin C. Nuts and seeds provide vitamin E, while seafood, especially fatty fish like salmon and mackerel, are abundant in omega-3 fatty acids. Incorporating these foods into daily meals can significantly benefit those at risk for or managing macular degeneration.
Foods to Avoid
Certain foods can exacerbate macular degeneration and should be avoided or consumed in moderation. These include highly processed foods, foods high in trans fats, and sugary snacks, which can contribute to inflammation and oxidative stress. Reducing the intake of fried foods, fatty meats, and refined carbohydrates can help maintain better overall eye health. It is also advisable to limit excessive salt intake, which can lead to hypertension, a risk factor for macular degeneration.
Supplements and Their Role
Evaluating Efficacy
While a balanced diet is ideal, supplements can help fill nutritional gaps. The Age-Related Eye Disease Study (AREDS) formula, which includes vitamins C and E, zinc, copper, lutein, and zeaxanthin, has been shown to reduce the risk of progression in intermediate and advanced stages of macular degeneration. It is important to evaluate the efficacy of supplements through clinical evidence and consult with healthcare providers before starting any new supplement regimen to ensure safety and appropriateness for individual health needs.
Choosing the Right Supplements
Choosing the right supplements involves understanding the specific needs of eye health and the quality of the products available. Look for supplements that contain the AREDS or AREDS2 formula and are manufactured by reputable companies. Checking for third-party testing and certifications can also ensure product quality and efficacy. Consulting with an ophthalmologist or nutritionist can provide personalized recommendations based on individual health profiles and nutritional needs.
Lifestyle Changes and Habits
Smoking and Alcohol Consumption
Impact on Eye Health
Smoking is a major risk factor for macular degeneration, significantly increasing the likelihood of developing the condition. The harmful chemicals in cigarettes can damage the retina and reduce the blood flow to the eyes. Similarly, excessive alcohol consumption can lead to nutritional deficiencies and oxidative stress, further exacerbating eye health issues. Addressing these habits is crucial for preventing and managing macular degeneration.
Strategies to Quit Smoking
Quitting smoking is one of the most effective steps to protect eye health. Strategies to quit smoking include nicotine replacement therapies, prescription medications, counseling, and support groups. Behavioral therapies and mindfulness techniques can also aid in managing withdrawal symptoms and preventing relapse. Seeking support from healthcare providers and engaging in a structured quit plan can significantly increase the chances of success.
Physical Activity
Benefits of Exercise
Regular physical activity benefits overall health and can specifically aid in preventing macular degeneration. Exercise improves cardiovascular health, which enhances blood flow to the retina, delivering essential nutrients and oxygen. It also helps in maintaining a healthy weight, reducing the risk of hypertension and diabetes, which are linked to eye diseases. Incorporating aerobic exercises, strength training, and flexibility exercises can provide comprehensive health benefits.
Recommended Exercises for Eye Health
Exercises that promote cardiovascular health, such as walking, jogging, swimming, and cycling, are particularly beneficial for eye health. Activities like yoga and tai chi can also improve circulation and reduce stress, contributing to overall well-being. Including eye-specific exercises, such as focusing on near and distant objects, can help in maintaining eye flexibility and strength. A balanced exercise routine tailored to individual fitness levels and health conditions can optimize benefits for eye health.
Managing Stress
Stress and Eye Health
Chronic stress can negatively impact eye health by increasing inflammation and oxidative stress in the body. It can also lead to unhealthy behaviors like poor diet, smoking, and reduced physical activity, which are risk factors for macular degeneration. Managing stress is essential for maintaining overall health and preventing the progression of eye diseases.
Techniques for Stress Reduction
Effective stress management techniques include mindfulness meditation, deep breathing exercises, yoga, and progressive muscle relaxation. Engaging in hobbies, spending time in nature, and maintaining social connections can also help reduce stress. Regular physical activity and a healthy diet contribute to better stress management. Incorporating these techniques into daily routines can improve mental well-being and support eye health.
Medical Treatments and Therapies
Pharmaceutical Interventions
Anti-VEGF Injections
Anti-VEGF (vascular endothelial growth factor) injections are a primary treatment for wet macular degeneration. These injections work by inhibiting the growth of abnormal blood vessels and reducing fluid leakage in the retina. Medications like Avastin, Lucentis, and Eylea are commonly used. Regular injections, typically administered monthly, can stabilize vision and, in some cases, improve it. This treatment requires ongoing monitoring and adherence to the injection schedule to achieve optimal results.
Other Medications
In addition to anti-VEGF injections, other medications may be used to manage macular degeneration. These include corticosteroids, which can reduce inflammation and swelling in the retina, and medications that address underlying conditions like hypertension or diabetes. Experimental drugs targeting different pathways of the disease are also under investigation. Combining pharmaceutical interventions with lifestyle changes can enhance treatment outcomes and slow disease progression.
Surgical Options
Laser Therapy
Laser therapy is used to treat certain cases of wet macular degeneration. It involves using a high-energy laser beam to seal leaking blood vessels and prevent further damage to the retina. While this procedure can be effective in stabilizing vision, it is less commonly used today due to the development of more targeted treatments like anti-VEGF injections. Laser therapy is typically reserved for specific cases where other treatments are not suitable or effective.
Photodynamic Therapy
Photodynamic therapy (PDT) combines a light-activated drug with a special laser to treat abnormal blood vessels in the retina. The drug, administered via injection, accumulates in the abnormal vessels, which are then activated by the laser light, causing them to close off. PDT can be used in conjunction with anti-VEGF injections for a more comprehensive approach to treating wet macular degeneration. This therapy requires careful monitoring and follow-up to assess effectiveness and manage any side effects.
Emerging Treatments
Gene Therapy
Gene therapy represents a promising frontier in the treatment of macular degeneration. This approach involves delivering genetic material directly into the cells of the retina to correct or replace defective genes responsible for the disease. Early clinical trials have shown potential in halting or even reversing vision loss. While still in the experimental stage, gene therapy could offer a long-term solution for macular degeneration, particularly for those with a genetic predisposition to the condition.
Stem Cell Research
Stem cell research is exploring the potential to regenerate damaged retinal cells in patients with macular degeneration. By transplanting stem cells into the retina, scientists hope to restore lost vision and improve retinal function. Clinical trials are ongoing, and while there are significant challenges to overcome, the potential for stem cell therapy to revolutionize the treatment of macular degeneration is substantial. Continued research and development in this field are essential for bringing these therapies to clinical practice.
Vision Aids and Rehabilitation
Optical Devices
Magnifiers and Telescopic Lenses
Magnifiers and telescopic lenses are valuable tools for individuals with macular degeneration, helping to enhance remaining vision for tasks like reading and detailed work. Handheld and stand magnifiers, along with electronic magnifiers, can provide different levels of magnification and ease of use. Telescopic lenses, which can be mounted on glasses or used as handheld devices, allow for better distance vision. These aids are customizable to meet the specific needs of each patient, improving their quality of life and independence.
Electronic Vision Aids
Advancements in technology have led to the development of sophisticated electronic vision aids, such as closed-circuit television (CCTV) systems, screen readers, and wearable devices like eSight and OrCam. These devices use cameras and digital displays to magnify and enhance images, making it easier for individuals with macular degeneration to read, recognize faces, and perform daily activities. The integration of artificial intelligence in some devices offers additional functionalities, such as object recognition and voice commands, further aiding those with vision loss.
Vision Rehabilitation Services
Low Vision Therapy
Low vision therapy involves working with specialists to maximize the use of remaining vision through adaptive techniques and tools. Occupational therapists and low vision specialists provide training on using magnifiers, electronic aids, and other assistive devices. They also teach strategies for improving contrast, lighting, and organization in the home. Personalized rehabilitation plans can help patients maintain independence and enhance their ability to perform everyday tasks despite vision loss.
Mobility Training
Mobility training is essential for individuals with significant vision impairment, helping them navigate their environment safely and confidently. Certified orientation and mobility specialists offer training in using white canes, guide dogs, and other mobility aids. They also provide instruction on spatial awareness and navigating public transportation and community spaces. This training is crucial for maintaining independence and reducing the risk of falls and injuries.
Home Modifications
Lighting and Contrast Enhancements
Enhancing lighting and contrast in the home environment can significantly aid individuals with macular degeneration. Proper lighting, such as task lighting for reading and cooking, reduces eye strain and improves visibility. Using high-contrast colors for household items and labeling can make them easier to identify. Simple modifications like these can improve safety and functionality in daily activities, contributing to a better quality of life.
Organization and Accessibility Tools
Organizing the home environment to make it more accessible is crucial for individuals with vision loss. This includes arranging furniture to create clear pathways, using large-print labels and tactile markers, and keeping frequently used items in consistent, easily reachable locations. Accessibility tools such as voice-activated assistants, smart home devices, and adaptive kitchen tools can further support independence. These modifications and tools help individuals with macular degeneration manage their daily tasks more effectively and safely.
Support Systems and Resources
Professional Support
Ophthalmologists and Optometrists
Ophthalmologists and optometrists play a critical role in diagnosing, treating, and managing macular degeneration. Regular eye examinations and monitoring are essential for early detection and effective treatment. These professionals can provide medical interventions, prescribe vision aids, and offer guidance on lifestyle modifications to support eye health. Building a strong relationship with eye care providers ensures comprehensive and continuous care.
Counselors and Social Workers
Counselors and social workers provide emotional and practical support for individuals coping with macular degeneration. They can assist with adjusting to vision loss, addressing mental health concerns, and accessing community resources. Counseling can help patients and their families navigate the emotional challenges of vision loss, while social workers can connect them with support services, financial assistance, and adaptive programs. These professionals are integral to a holistic approach to managing macular degeneration.
Support Groups and Communities
Local Support Groups
Local support groups offer a sense of community and shared experience for individuals with macular degeneration. These groups provide opportunities to share coping strategies, receive emotional support, and learn from others facing similar challenges. Meeting regularly with others who understand the impact of vision loss can reduce feelings of isolation and provide valuable insights into managing the condition. Local support groups often collaborate with healthcare providers and organizations to offer educational resources and advocacy.
Online Communities and Forums
Online communities and forums provide a platform for individuals with macular degeneration to connect, share experiences, and access information from anywhere in the world. These virtual spaces offer flexibility and anonymity, allowing for open discussion and support. Participants can exchange tips on managing daily tasks, learn about the latest treatments and research, and receive encouragement from a global community. Online resources also often include webinars, podcasts, and virtual events, enhancing access to information and support.
Educational Materials and Workshops
Books and Brochures
Educational materials, such as books and brochures, provide valuable information on macular degeneration, including its causes, symptoms, and treatment options. These resources are often available through healthcare providers, libraries, and online platforms. They offer practical advice on managing vision loss, maintaining eye health, and adapting daily activities. Accessible formats, such as large print and audiobooks, ensure that these materials are available to individuals with varying degrees of vision impairment.
Webinars and Seminars
Webinars and seminars offer interactive and accessible ways to learn about macular degeneration. These events, often hosted by healthcare organizations, research institutions, and support groups, feature experts discussing the latest advancements in treatment, research, and management strategies. Participants can engage in Q&A sessions, share their experiences, and connect with professionals and peers. These educational opportunities are invaluable for staying informed and proactive in managing macular degeneration.
FAQs
1. What is the difference between dry and wet macular degeneration?
Dry macular degeneration involves the gradual thinning of the macula, leading to vision loss over time. Wet macular degeneration is characterized by the growth of abnormal blood vessels under the retina, which can leak fluid or blood, causing rapid and severe vision loss.
2. Can lifestyle changes really impact the progression of macular degeneration?
Yes, lifestyle changes such as a healthy diet, regular exercise, quitting smoking, and managing stress can significantly impact the progression of macular degeneration. These changes help reduce risk factors and support overall eye health.
3. Are there any new treatments for macular degeneration on the horizon?
Emerging treatments such as gene therapy and stem cell research hold promise for macular degeneration. These therapies aim to address the underlying causes of the disease and potentially restore lost vision. Clinical trials are ongoing to determine their safety and efficacy.
4. How can vision aids help individuals with macular degeneration?
Vision aids, such as magnifiers, telescopic lenses, and electronic vision devices, enhance remaining vision and support daily activities. They are tailored to individual needs, helping to improve reading, recognizing faces, and maintaining independence.