Male fertility is a critical aspect of reproductive health and overall well-being. However, certain medical treatments, such as chemotherapy and radiation therapy, can significantly impact fertility by damaging sperm production. For individuals facing conditions like cancer, where aggressive treatments like autologous stem cell transplant (ASCT) are necessary, preserving fertility becomes a pressing concern. ASCT involves harvesting a patient’s own stem cells before administering high-dose chemotherapy or radiation, then reintroducing the stem cells to restore the bone marrow. While ASCT is a life-saving procedure for many, it often comes with the risk of infertility due to the damage inflicted on the testes during the process. In recent years, advancements in reproductive medicine have offered hope for male fertility restoration post-ASCT through various interventions, including stem cell therapies. We will explore the challenges of male fertility post-ASCT and the emerging strategies for restoration.
Understanding Autologous Stem Cell Transplantation
What Is Autologous Stem Cell Transplantation?
Autologous stem cell transplantation is a procedure in which a patient’s own stem cells are harvested and then reinfused after the patient has received high-dose chemotherapy or radiation therapy. This approach is commonly used to treat blood cancers such as leukemia, lymphoma, and multiple myeloma. The primary goal is to eradicate cancerous cells and then repopulate the patient’s bone marrow with healthy stem cells.
Impact on Male Fertility
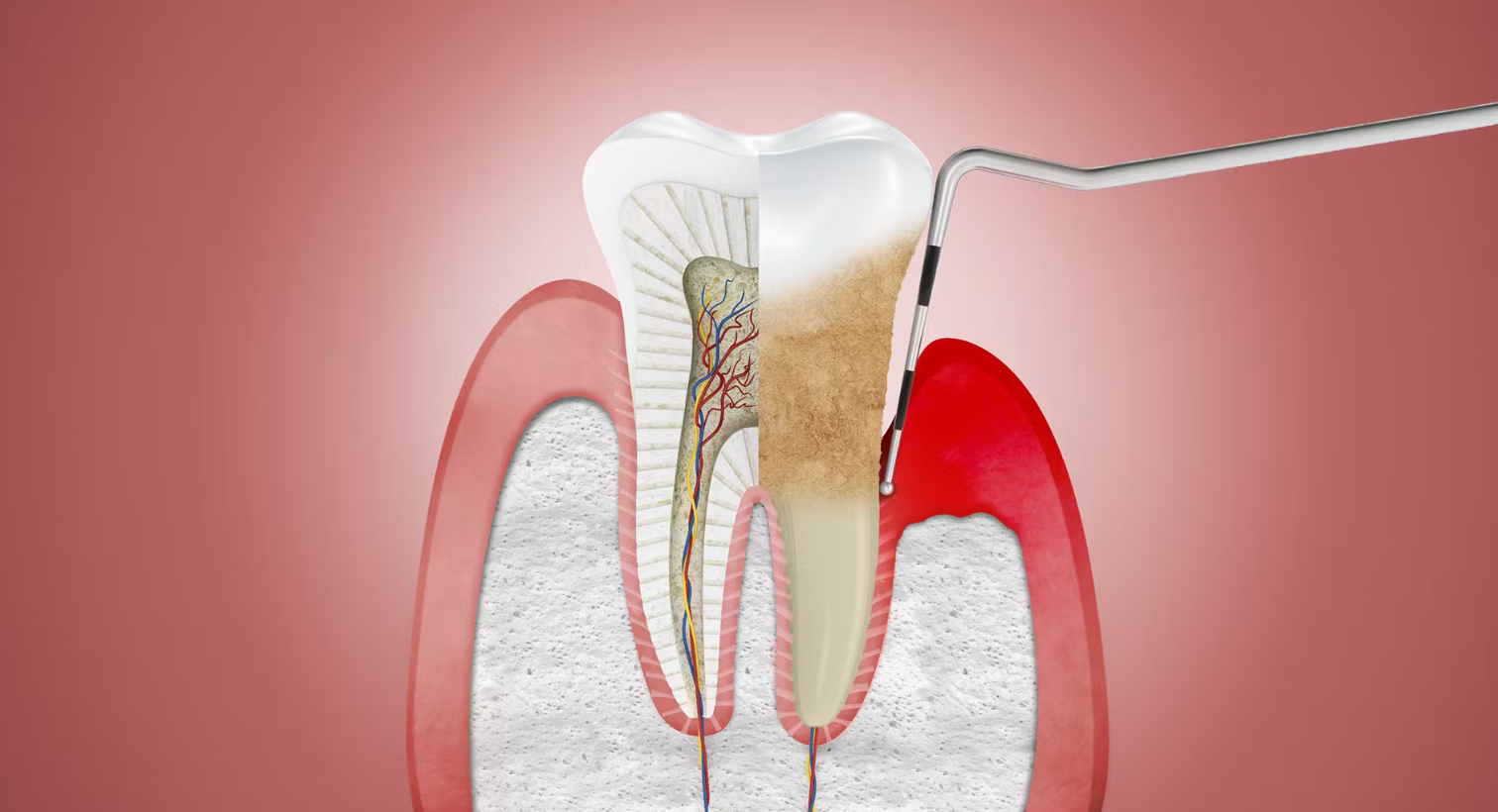
The high-dose chemotherapy and radiation therapy that precedes the transplantation can severely damage the germ cells in the testes, leading to temporary or permanent infertility. Germ cells are responsible for producing sperm, and damage to these cells can affect sperm production and quality.
Duration and Extent of Fertility Impairment
The duration and extent of fertility impairment post-ASCT can vary depending on several factors, including:
- Age: Younger patients may recover fertility more quickly than older patients.
- Type of Chemotherapy/Radiation: The specific agents and doses used can impact fertility differently.
- Pre-Existing Fertility: Patients with higher fertility levels before ASCT may have a better chance of recovery.
Understanding Male Fertility Post-ASCT
Impact of ASCT on Male Fertility
ASCT is a standard treatment for various hematological malignancies, including leukemia, lymphoma, and multiple myeloma. While it offers a chance for remission or cure, the high-dose chemotherapy or radiation used in ASCT can have detrimental effects on the reproductive system. The testes, responsible for sperm production, are particularly vulnerable to the cytotoxic effects of these treatments. Chemotherapy drugs such as alkylating agents and radiation can damage the germinal epithelium within the testes, leading to impaired spermatogenesis and ultimately infertility.
Factors Influencing Fertility Restoration
Several factors influence the likelihood of fertility restoration post-ASCT:
- Age: Younger males tend to have better chances of restoring fertility post-ASCT due to their higher baseline sperm counts and regenerative capacity of the testes.
- Type and Intensity of Conditioning Regimen: The specific chemotherapy drugs and radiation doses used in the conditioning regimen play a crucial role in determining the extent of testicular damage and, consequently, the potential for fertility restoration.
- Duration Since ASCT: The longer the duration since ASCT, the more time the testes have had to recover from the damage caused by the treatment. However, fertility restoration may become increasingly challenging with prolonged intervals due to irreversible testicular damage.
- Presence of Pre-existing Fertility Issues: Individuals with pre-existing fertility issues or comorbidities may face additional challenges in restoring fertility post-ASCT.
Strategies for Male Fertility Restoration
Pharmacological Interventions
Hormonal Therapy
Hormonal therapies such as testosterone replacement therapy (TRT) and gonadotropin-releasing hormone (GnRH) analogs have been explored for fertility restoration post-ASCT. TRT can help alleviate symptoms of hypogonadism resulting from testicular damage, but its efficacy in restoring fertility is limited. GnRH analogs, on the other hand, work by suppressing gonadotropin secretion, thereby reducing testicular damage during chemotherapy. However, the long-term effects of GnRH analogs on fertility restoration require further investigation.
Growth Factors and Cytokines
Several growth factors and cytokines, such as granulocyte colony-stimulating factor (G-CSF) and stem cell factor (SCF), have shown potential in promoting testicular regeneration and spermatogenesis post-ASCT. These agents act by stimulating the proliferation and differentiation of spermatogonial stem cells, thereby enhancing sperm production. Clinical studies evaluating the efficacy of growth factors and cytokines in restoring fertility post-ASCT are ongoing.
Surgical Interventions
Testicular Tissue Cryopreservation and Transplantation
Testicular tissue cryopreservation involves the extraction and freezing of testicular tissue containing spermatogonial stem cells before ASCT. After completion of cancer treatment, the cryopreserved tissue can be thawed and transplanted back into the patient’s testes, where it can regenerate spermatogenesis. While still considered experimental, testicular tissue cryopreservation holds promise as a potential fertility preservation option for prepubertal boys undergoing ASCT.
Microdissection Testicular Sperm Extraction (Micro-TESE)
Micro-TESE is a surgical procedure performed to retrieve sperm directly from the testes of men with non-obstructive azoospermia, a condition characterized by an absence of sperm in the ejaculate due to testicular dysfunction. For male cancer survivors with impaired spermatogenesis post-ASCT, Micro-TESE offers a chance to obtain viable sperm for use in assisted reproductive techniques such as intracytoplasmic sperm injection (ICSI).
Stem Cell Therapies
Spermatogonial Stem Cell Transplantation
Spermatogonial stem cell (SSC) transplantation involves the transfer of SSCs into the seminiferous tubules of the testes to restore spermatogenesis. This experimental approach holds promise for fertility restoration in male cancer survivors post-ASCT. Preclinical studies in animal models have demonstrated the feasibility and efficacy of SSC transplantation in restoring fertility following gonadotoxic treatments. Clinical trials investigating the safety and efficacy of SSC transplantation in humans are underway, offering hope for a novel therapeutic option for male fertility restoration post-ASCT.
Psychological Support
In addition to medical interventions, psychological support plays a crucial role in addressing the emotional and psychosocial impact of infertility on male cancer survivors post-ASCT. Fertility preservation counseling and support groups can help individuals navigate their fertility options, cope with feelings of loss and grief, and make informed decisions about their reproductive future.
India’s Approach to Male Fertility Restoration Post-ASCT
India has made significant strides in male fertility restoration post-ASCT, with specialized clinics and advanced research initiatives contributing to the development of effective treatments.
Advancements in Fertility Preservation
India is home to a number of cutting-edge fertility clinics that offer advanced fertility preservation services, such as:
- Sperm Banking: Many clinics provide high-quality sperm banking services, ensuring that patients have the option to preserve their fertility before undergoing ASCT.
- Testicular Tissue Cryopreservation: For prepubertal boys facing ASCT, India offers experimental testicular tissue cryopreservation services.
Research and Development
Indian research institutions are actively exploring new approaches to male fertility restoration post-ASCT, including:
- Stem Cell Research: Indian researchers are investigating the potential of stem cell therapies to regenerate damaged germ cells and restore fertility.
- Hormone Therapies: Studies in India are focusing on hormone therapies that may stimulate sperm production in patients post-ASCT.
- Antioxidants: Indian scientists are exploring the potential benefits of antioxidants in improving sperm quality and motility.
Restoring Fertility in Male
Male fertility restoration post-ASCT presents a complex and multifaceted challenge. While ASCT offers a chance for remission or cure in individuals with hematological malignancies, it often comes at the cost of infertility due to testicular damage. However, advancements in reproductive medicine, including pharmacological interventions, surgical techniques, and stem cell therapies—including emerging applications such as stem cell therapy for Huntington’s disease—offer hope for restoring fertility in male cancer survivors post-ASCT. Further research and clinical trials are needed to elucidate the safety and efficacy of these interventions and improve outcomes for individuals seeking to preserve their fertility after cancer treatment. In addition to medical interventions, providing psychological support and counseling services is essential for addressing the emotional and psychosocial needs of male cancer survivors facing infertility post-ASCT. By integrating medical and psychosocial approaches, healthcare professionals can better support individuals in their journey to preserve their fertility and achieve their reproductive goals after cancer treatment.