Myelodysplastic Syndrome (MDS) is a group of disorders characterized by ineffective production of blood cells in the bone marrow. It is considered a type of blood cancer that affects the bone marrow’s ability to produce healthy blood cells. MDS primarily impacts the production of red blood cells, white blood cells, and platelets, leading to anemia, infections, and bleeding disorders.
Causes and Risk Factors
While the exact cause of MDS remains unclear, several risk factors have been identified. Exposure to certain chemicals, such as benzene and pesticides, as well as radiation therapy or chemotherapy for other cancers, increases the risk of developing MDS. Additionally, advanced age, smoking, and certain genetic conditions like Down syndrome are associated with a higher likelihood of developing MDS.
Symptoms and Diagnosis
Symptoms of MDS can vary depending on the severity of the condition and which types of blood cells are affected. Common symptoms include fatigue, shortness of breath, pale skin, frequent infections, easy bruising or bleeding, and weakness. Diagnosis often involves blood tests to evaluate blood cell counts and morphology, bone marrow biopsy, and genetic testing to assess chromosomal abnormalities.
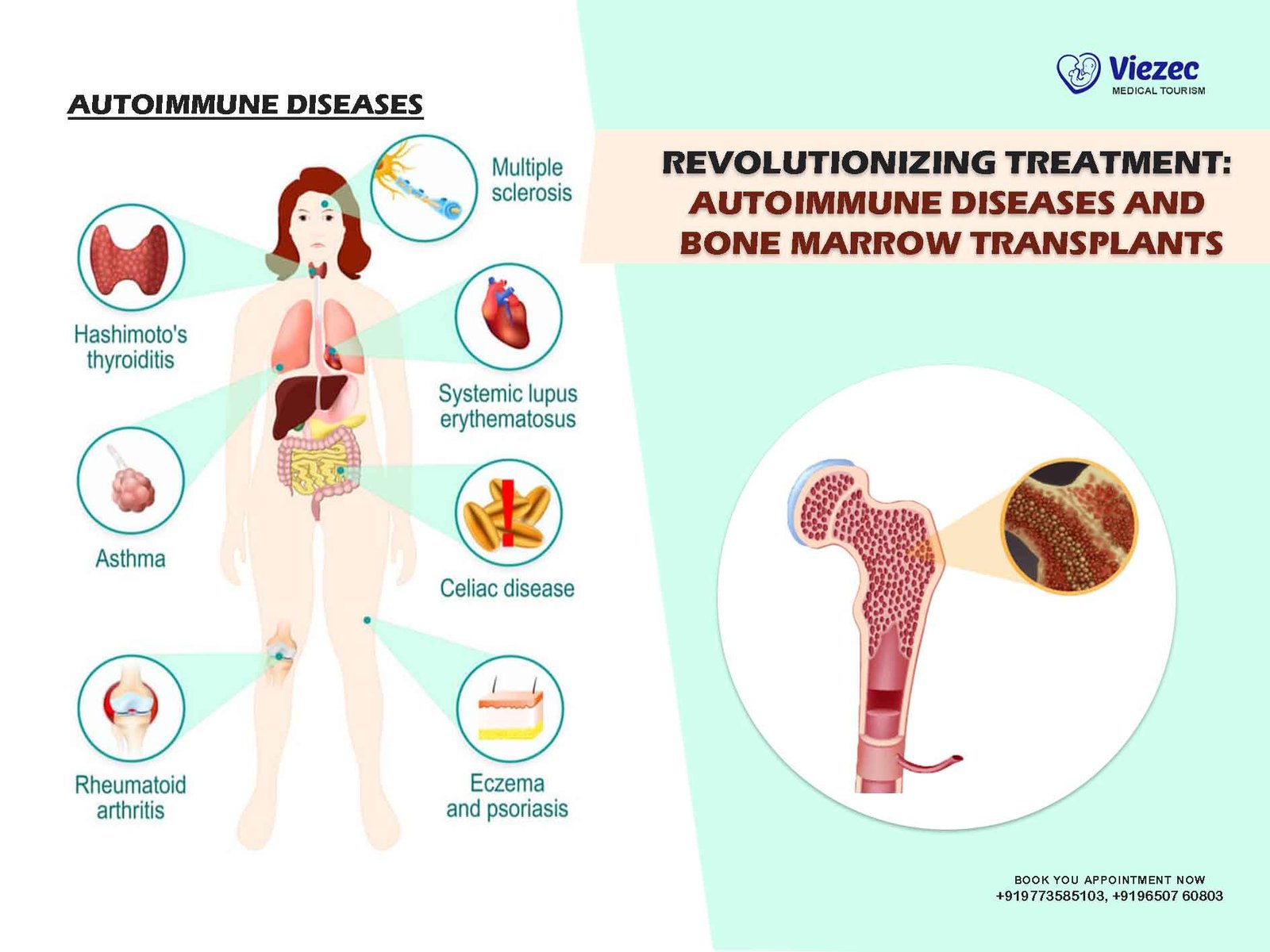
Bone Marrow Transplantation: An Overview
What is a Bone Marrow Transplant?
A bone marrow transplant (BMT), also known as a hematopoietic stem cell transplant (HSCT), is a procedure used to replace damaged or diseased bone marrow with healthy stem cells. These stem cells can be obtained from the patient (autologous transplant), a matched donor (allogeneic transplant), or umbilical cord blood. BMT allows for the restoration of normal blood cell production in individuals with various blood disorders, including MDS.
Types of Bone Marrow Transplant
Autologous Transplant
In an autologous transplant, the patient’s own stem cells are collected prior to undergoing intensive chemotherapy or radiation therapy. After the treatment, the collected stem cells are infused back into the patient’s bloodstream, where they travel to the bone marrow and begin producing healthy blood cells. Autologous transplants are commonly used in treating certain types of lymphomas and multiple myeloma.
Allogeneic Transplant
Allogeneic transplants involve using stem cells from a donor, typically a sibling or unrelated matched donor. This type of transplant offers the advantage of potentially eradicating remaining cancer cells and providing a new immune system to the recipient. However, it carries a higher risk of complications, including graft-versus-host disease (GVHD), where the donor immune cells attack the recipient’s tissues.
Umbilical Cord Blood Transplant
Umbilical cord blood transplants utilize stem cells collected from the umbilical cord and placenta after childbirth. These stem cells are frozen and stored in cord blood banks for future use. While cord blood transplants offer the advantage of wider availability and lower risk of GVHD, they may take longer to engraft and reconstitute the immune system compared to other types of transplants.
Preparing for a Bone Marrow Transplant
Patient Evaluation
Before undergoing a bone marrow transplant, patients undergo a comprehensive evaluation to assess their overall health and suitability for the procedure. This evaluation typically includes medical history review, physical examination, blood tests, imaging studies, and assessment of organ function.
Conditioning Regimen
Prior to transplant, patients receive a conditioning regimen, which consists of high-dose chemotherapy and/or total body irradiation. This intensive treatment aims to destroy any remaining cancer cells in the body and suppress the recipient’s immune system to prevent rejection of the donor stem cells.
Donor Matching
For allogeneic transplants, finding a suitable donor with matching human leukocyte antigen (HLA) markers is crucial to minimize the risk of rejection and GVHD. Siblings are often the first choice for donors, but unrelated donors may be sought through national and international registries.
Bone Marrow Transplantation Process
Stem Cell Collection
For autologous transplants, stem cells are collected from the patient’s bloodstream using a process called apheresis. Prior to collection, the patient may receive medications to stimulate the production and release of stem cells from the bone marrow into the bloodstream.
Stem Cell Infusion
Once collected, the stem cells are processed and purified in the laboratory before being infused back into the patient’s bloodstream through a central venous catheter. The infused stem cells travel to the bone marrow, where they begin to grow and produce healthy blood cells.
Engraftment and Recovery
Engraftment refers to the successful establishment of the donor stem cells in the recipient’s bone marrow, leading to the production of new blood cells. Following transplant, patients are closely monitored for signs of engraftment, complications, and graft rejection. Recovery from a bone marrow transplant can be a lengthy process, often requiring weeks to months of hospitalization and ongoing medical care.
Bone Marrow Transplantation for Myelodysplastic Syndrome
Indications for Transplantation
High-Risk Disease
Bone marrow transplantation is considered a potentially curative treatment option for patients with high-risk MDS, particularly those with advanced disease or poor prognostic features. High-risk features may include high-risk cytogenetics, refractory anemia with excess blasts (RAEB), or transformation to acute myeloid leukemia (AML).
Disease Progression
Patients who have failed to respond to conventional treatments for MDS or have experienced disease progression despite treatment may be candidates for bone marrow transplantation. Transplantation offers the possibility of achieving long-term remission and improving overall survival in these individuals.
Treatment Outcomes
Survival Rates
The outcomes of bone marrow transplantation for MDS vary depending on several factors, including disease risk, patient age, donor type, and comorbidities. Overall survival rates have improved significantly in recent years, with studies reporting 1-year survival rates ranging from 50% to 70% for allogeneic transplants in MDS patients.
Disease-Free Survival
Achieving disease-free survival following bone marrow transplantation is an important goal in the treatment of MDS. Studies have demonstrated that patients who achieve complete remission after transplant have a higher likelihood of long-term disease control and improved quality of life.
Complications and Side Effects
Graft-versus-Host Disease (GVHD)
One of the most significant complications of allogeneic bone marrow transplantation is graft-versus-host disease, where the donor immune cells attack the recipient’s tissues, leading to inflammation and organ damage. GVHD can affect the skin, liver, gastrointestinal tract, and other organs and may occur acutely or chronically.
Infections
Patients undergoing bone marrow transplantation are at increased risk of infections due to the suppression of their immune system during the conditioning regimen and early post-transplant period. Common infections include bacterial, viral, and fungal infections, which can be life-threatening if not promptly diagnosed and treated.
Graft Failure
Graft failure, where the donor stem cells fail to engraft and produce new blood cells, is a rare but serious complication of bone marrow transplantation. Risk factors for graft failure include older age, prior transplant history, and underlying bone marrow dysfunction.
Bone marrow transplantation offers a potentially curative treatment option for patients with high-risk Myelodysplastic Syndrome who have failed to respond to conventional therapies or have experienced disease progression. While transplantation carries risks and complications, recent advances in transplant techniques, donor selection, and supportive care have led to improved outcomes and survival rates for MDS patients undergoing transplantation. Ongoing research and clinical trials are focused on further refining transplantation strategies and developing novel therapies to enhance the efficacy and safety of transplantation for MDS.