Neurological disorders encompass a broad spectrum of conditions affecting the brain, spinal cord, and nerves throughout the body. These disorders can manifest in various forms, including cognitive impairment, motor dysfunction, sensory deficits, and disruptions in autonomic functions. Examples of neurological disorders include Parkinson’s disease, Alzheimer’s disease, stroke, spinal cord injuries, and multiple sclerosis.
Understanding the Complexity of Neurological Disorders
Neurological disorders are characterized by their intricate interplay of genetic, environmental, and lifestyle factors. The pathophysiology of these conditions often involves complex molecular and cellular mechanisms, making treatment challenging. Traditional therapeutic approaches, such as pharmacological interventions and rehabilitative strategies, have limitations in addressing the underlying causes of neurological damage and restoring normal function.
Current Challenges in Treatment Approaches
Despite significant advancements in medical science, neurological disorders remain a major healthcare burden worldwide. Many existing treatment modalities focus on symptom management rather than disease modification. Additionally, the blood-brain barrier presents a formidable obstacle to drug delivery, limiting the effectiveness of conventional therapies. As a result, there is a pressing need for innovative treatment strategies that can target the root causes of neurological dysfunction.
Fundamentals of Stem Cell Therapy
Stem cell therapy has emerged as a promising approach for treating neurological disorders by harnessing the regenerative potential of stem cells to repair damaged tissues and restore lost function. Stem cells are unique cells capable of self-renewal and differentiation into various cell types, making them ideal candidates for regenerative medicine applications.
Overview of Stem Cells and Their Properties
Stem cells can be broadly classified into three main categories based on their origin and developmental potential: embryonic stem cells (ESCs), adult stem cells, and induced pluripotent stem cells (iPSCs). Each type of stem cell offers distinct advantages and challenges for therapeutic use.
Types of Stem Cells Used in Therapy
Embryonic Stem Cells
Derived from the inner cell mass of early-stage embryos, ESCs have the ability to differentiate into any cell type in the body. Their pluripotent nature makes them valuable for studying development and for potential therapeutic applications. However, ethical concerns and the risk of immune rejection limit their clinical utility.
Adult Stem Cells
Adult stem cells are found in various tissues throughout the body and play essential roles in tissue maintenance and repair. Unlike ESCs, adult stem cells are multipotent or tissue-specific, meaning they can differentiate into a limited range of cell types. These cells offer advantages such as reduced risk of immune rejection and ethical considerations compared to ESCs.
Induced Pluripotent Stem Cells
iPSCs are generated by reprogramming adult somatic cells to a pluripotent state using genetic manipulation or other reprogramming techniques. Like ESCs, iPSCs have the potential to differentiate into any cell type, making them a valuable resource for disease modeling, drug discovery, and personalized regenerative medicine.
Mechanisms of Action in Neurological Disorders
Stem cells exert their therapeutic effects through various mechanisms, including cell replacement, neuroprotection, modulation of inflammation, and promotion of endogenous repair processes. By integrating into damaged tissues and secreting trophic factors, stem cells can promote tissue regeneration, enhance synaptic connectivity, and improve neurological function.
Advancements in Stem Cell Research
Recent years have witnessed significant breakthroughs in stem cell technology, paving the way for more efficient and reliable methods of stem cell isolation, culturing, and differentiation. Innovative techniques such as CRISPR-Cas9 gene editing have revolutionized the field by enabling precise genetic modifications in stem cells for therapeutic applications.
Breakthroughs in Stem Cell Technology
Advanced imaging techniques and biomaterials have facilitated the development of three-dimensional (3D) culture systems that better mimic the physiological microenvironment of neural tissues. These organoid models allow researchers to study disease mechanisms and screen potential therapeutics in a more physiologically relevant context.
Innovative Techniques in Stem Cell Isolation and Culturing
Novel methods for isolating and expanding stem cells have been developed to overcome technical challenges and improve the scalability of stem cell production. Automation and bioreactor systems enable large-scale culture of stem cells under controlled conditions, ensuring reproducibility and quality control in manufacturing processes.
Emerging Trends in Stem Cell Therapy
Stem cell therapy holds great promise for the treatment of a wide range of neurological disorders, including Parkinson’s disease, Alzheimer’s disease, stroke, spinal cord injuries, and multiple sclerosis. Preclinical and clinical studies have demonstrated the safety and efficacy of stem cell-based interventions in improving motor function, cognitive abilities, and quality of life in patients.
Neurological Disorders Amenable to Stem Cell Therapy
Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disorder characterized by the progressive loss of dopaminergic neurons in the substantia nigra region of the brain. Stem cell transplantation offers a potential strategy for replenishing lost dopaminergic neurons and restoring dopamine levels in the brain, thereby alleviating motor symptoms associated with the disease.
Alzheimer’s Disease
Alzheimer’s disease is the most common cause of dementia, characterized by the accumulation of amyloid-beta plaques and neurofibrillary tangles in the brain. Stem cell-based approaches aim to replace damaged neurons, promote synaptic plasticity, and modulate neuroinflammation to mitigate cognitive decline and improve memory function in Alzheimer’s patients.
Stroke
Stroke occurs when blood flow to the brain is interrupted, leading to tissue damage and neurological deficits. Stem cell therapy holds promise for promoting neuroregeneration, angiogenesis, and neuroprotection in the ischemic brain, thereby enhancing functional recovery and reducing disability in stroke survivors.
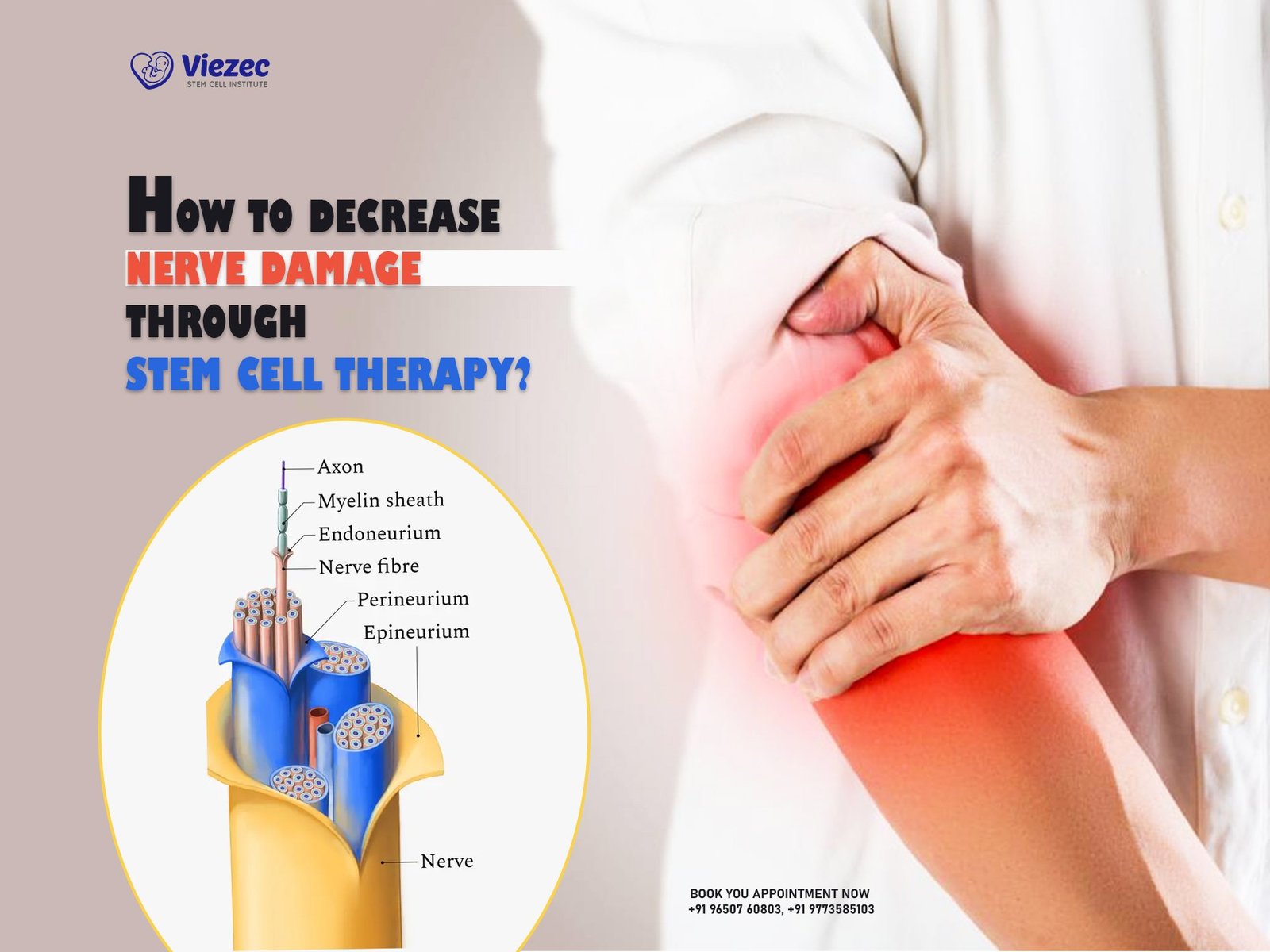
Spinal Cord Injuries
Spinal cord injuries result in loss of motor and sensory function below the level of injury, often leading to paralysis and sensory deficits. Stem cell transplantation offers a potential avenue for repairing damaged spinal cord tissue, promoting axonal regeneration, and restoring neuronal connectivity to facilitate recovery of motor and sensory function.
Multiple Sclerosis
Multiple sclerosis is an autoimmune disorder characterized by inflammation, demyelination, and axonal damage in the central nervous system. Stem cell-based therapies aim to modulate the immune response, promote remyelination, and protect neuronal integrity to prevent disease progression and improve functional outcomes in MS patients.
Preclinical and Clinical Studies
Animal models play a crucial role in preclinical research for evaluating the safety and efficacy of stem cell therapies in neurological disorders. Translational studies bridge the gap between preclinical findings and clinical applications, informing the design and implementation of human clinical trials to assess the therapeutic potential of stem cell-based interventions.
Clinical Trials: Efficacy and Safety Assessment
Clinical trials are essential for evaluating the efficacy and safety of stem cell therapies in human subjects. Rigorous clinical trial design, including randomized controlled trials with placebo controls and long-term follow-up assessments, is necessary to establish the safety profile and therapeutic benefits of stem cell-based interventions in neurological disorders.
Stem Cell Delivery Strategies
The method of stem cell delivery is a critical consideration in optimizing therapeutic outcomes and minimizing potential risks. Various routes of administration, including intravenous infusion, intracerebral injection, and intrathecal administration, have been explored for targeted delivery of stem cells to the central nervous system.
Intravenous Infusion
Intravenous infusion of stem cells allows for systemic distribution and homing of cells to sites of injury or inflammation in the brain and spinal cord. This non-invasive delivery approach offers advantages such as ease of administration, minimal procedural risk, and the potential for repeated dosing over time.
Intracerebral Injection
Intracerebral injection involves direct implantation of stem cells into specific brain regions affected by neurological disorders. This targeted delivery approach enables precise localization of stem cells to areas of tissue damage or neuronal loss, maximizing therapeutic efficacy while minimizing off-target effects.
Intrathecal Administration
Intrathecal administration involves the injection of stem cells into the cerebrospinal fluid surrounding the spinal cord and brain. This route of delivery allows for widespread distribution of stem cells throughout the central nervous system, offering potential benefits for treating multifocal or diffuse neurological disorders.
Non-Invasive Delivery Methods
Advances in non-invasive delivery methods, such as focused ultrasound and magnetic targeting, hold promise for enhancing the precision and efficiency of stem cell delivery to specific brain regions. These innovative approaches enable spatially controlled release of stem cells and therapeutic agents, minimizing systemic side effects and improving therapeutic outcomes.
Challenges and Limitations
Despite the potential benefits of stem cell therapy, several challenges and limitations must be addressed to realize its full therapeutic potential in neurological disorders.
Immune Rejection
The immune response poses a significant barrier to the success of stem cell transplantation, leading to rejection of transplanted cells and activation of inflammatory pathways. Strategies to mitigate immune rejection, such as immunosuppressive therapy and cell engineering techniques, are needed to improve the long-term survival and engraftment of transplanted stem cells.
Tumorigenicity
One of the major safety concerns associated with stem cell therapy is the risk of tumorigenicity, particularly with pluripotent stem cells such as ESCs and iPSCs. The potential for uncontrolled proliferation and differentiation of stem cells into teratomas or other malignant tumors underscores the importance of rigorous safety assessments and monitoring protocols in clinical trials.
Ethical Considerations
The ethical implications of stem cell research and therapy, particularly with regard to the use of human embryos and genetic manipulation techniques, raise important ethical considerations that must be carefully weighed and addressed. Ethical guidelines and regulatory frameworks are essential for ensuring responsible conduct and safeguarding the rights and welfare of research participants and patients.
Standardization of Protocols
Standardization of protocols for stem cell isolation, culturing, and characterization is essential for ensuring reproducibility and consistency in experimental procedures and clinical applications. Quality control measures and regulatory oversight are necessary to establish standardized protocols and best practices for stem cell therapy.
Safety and Regulatory Considerations
Regulatory agencies such as the U.S. Food and Drug Administration (FDA) play a crucial role in overseeing the development and commercialization of stem cell therapies. Stringent regulatory requirements, including preclinical testing, Good Manufacturing Practice (GMP) standards, and clinical trial oversight, are necessary to ensure the safety, efficacy, and quality of stem cell-based interventions.
FDA Regulations on Stem Cell Therapies
The FDA regulates stem cell therapies as biological products or drugs, depending on their intended use and manufacturing process. Stem cell products intended for clinical use must undergo rigorous preclinical and clinical testing to demonstrate safety and efficacy before receiving regulatory approval for commercialization.
Ethical Guidelines and Informed Consent
Informed consent is an essential ethical principle in stem cell research and therapy, ensuring that research participants and patients are fully informed about the nature of the treatment, potential risks and benefits, and alternatives. Ethical guidelines and institutional review boards (IRBs) provide oversight and ensure compliance with ethical standards and regulatory requirements.
Patient Selection Criteria
Patient selection criteria are important considerations in determining eligibility for stem cell therapy and optimizing treatment outcomes. Factors such as disease stage, severity, comorbidities, and patient demographics influence the selection of appropriate candidates for stem cell-based interventions.
Clinical Outcomes and Case Studies
Clinical studies have reported encouraging outcomes following stem cell therapy in neurological disorders, including improvements in motor function, cognitive abilities, and quality of life.
Improvement in Motor Function
Stem cell transplantation has been shown to improve motor function in patients with Parkinson’s disease, stroke, and spinal cord injuries by promoting neuronal survival, axonal regeneration, and synaptic connectivity.
Cognitive Enhancement
Stem cell-based interventions have demonstrated potential benefits for cognitive enhancement and memory improvement in patients with Alzheimer’s disease and other neurodegenerative disorders.
Quality of Life Measures
Quality of life measures, including activities of daily living, mobility, and independence, have shown improvement following stem cell therapy in neurological disorders, leading to enhanced overall well-being and functional outcomes.
Long-term Follow-up Studies
Long-term follow-up studies are essential for assessing the durability and safety of stem cell therapy over time, monitoring for potential adverse events, and evaluating the sustainability of therapeutic benefits in patients with neurological disorders.
Combination Therapies and Future Directions
Combination therapies involving stem cells and pharmacological agents, gene therapy, personalized medicine approaches, and nanotechnology hold promise for enhancing the efficacy and safety of stem cell-based interventions in neurological disorders.
Stem Cells with Pharmacological Agents
Combining stem cells with pharmacological agents, such as growth factors, neurotrophic factors, and immunomodulators, can synergistically enhance therapeutic outcomes by promoting cell survival, neuroprotection, and tissue repair mechanisms.
Gene Therapy Combined with Stem Cells
Gene therapy approaches, including gene editing and gene delivery techniques, can be combined with stem cell transplantation to modulate gene expression, correct genetic mutations, and enhance the regenerative potential of stem cells in neurological disorders.
Personalized Medicine Approaches
Personalized medicine approaches, based on patient-specific characteristics, genetic profiles, and disease biomarkers, can tailor treatment strategies to individual patients’ needs, maximizing therapeutic efficacy and minimizing potential risks.
Nanotechnology in Stem Cell Delivery
Nanotechnology-based approaches, such as nanoparticle-mediated drug delivery and targeted cell therapies, offer opportunities for enhancing the precision, efficiency, and safety of stem cell delivery to specific brain regions affected by neurological disorders.
Cost-effectiveness and Accessibility
The cost-effectiveness and accessibility of stem cell therapy pose significant challenges to widespread adoption and equitable access to advanced treatments for neurological disorders.
Economic Impact of Stem Cell Therapy
The economic burden of neurological disorders, including healthcare costs, caregiver burden, and lost productivity, underscores the importance of developing cost-effective treatment strategies that can improve patient outcomes and reduce long-term healthcare expenditures.
Insurance Coverage and Reimbursement Policies
Insurance coverage and reimbursement policies play a critical role in facilitating patient access to stem cell therapy and ensuring equitable reimbursement for healthcare providers, researchers, and patients.
Global Disparities in Access to Advanced Treatments
Disparities in healthcare infrastructure, resources, and regulatory frameworks contribute to inequalities in access to advanced treatments for neurological disorders, highlighting the need for global collaboration and advocacy efforts to address healthcare disparities and promote health equity.
Conclusion and Future Prospects
Stem cell therapy holds great promise for revolutionizing the treatment of neurological disorders by addressing the underlying causes of disease and promoting tissue regeneration and functional recovery. Despite the challenges and limitations, ongoing research efforts and collaborative initiatives are driving innovation and advancing the field of regenerative medicine. With continued scientific progress and regulatory support, stem cell therapy has the potential to transform clinical practice and improve the lives of millions of patients worldwide.
Summary of Key Findings
Stem cell therapy offers a promising approach for treating neurological disorders by promoting tissue regeneration, neuroprotection, and functional recovery.
Promising Areas for Future Research
Future research directions include optimizing stem cell delivery strategies, enhancing the safety and efficacy of stem cell therapies, and exploring combination therapies and personalized medicine approaches.
Implications for Clinical Practice and Patient Care
Stem cell therapy has the potential to revolutionize clinical practice by providing novel treatment options for patients with neurological disorders and improving overall patient outcomes and quality of life.
The Role of Collaborative Efforts in Advancing Stem Cell Therapies
Collaborative efforts among researchers, clinicians, policymakers, and patient advocacy groups are essential for advancing stem cell therapies, overcoming barriers to translation, and ensuring equitable access to advanced treatments for neurological disorders.