Atopic dermatitis (AD), a chronic inflammatory skin condition, affects millions of individuals worldwide, leading to discomfort, impaired quality of life, and substantial healthcare costs. Traditional treatments such as topical corticosteroids and immunosuppressants offer relief but often come with side effects and limited efficacy, especially in severe cases. In recent years, stem cell therapy has emerged as a promising frontier in the management of atopic dermatitis, offering potential for disease modification and tissue repair. This article explores the science behind stem cell therapy, its application in atopic dermatitis, current research findings, challenges, and future prospects.
Understanding Atopic Dermatitis
What is Atopic Dermatitis?
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin disorder characterized by red, itchy, and inflamed skin patches. It often begins in infancy or childhood and can persist into adulthood, significantly impacting the quality of life. While the exact cause of atopic dermatitis remains elusive, a combination of genetic, environmental, and immune system factors is believed to play a role in its development.
Current Treatment Challenges
Traditional treatments for atopic dermatitis primarily focus on symptom management and include topical corticosteroids, moisturizers, antihistamines, and immunomodulators. However, these treatments have limitations, including incomplete efficacy, potential side effects such as skin thinning and increased susceptibility to infections, and the need for long-term use, which can lead to medication fatigue and decreased compliance. Additionally, some patients, particularly those with severe or refractory disease, may not respond adequately to available therapies, highlighting the need for alternative treatment approaches.
Promise of Stem Cell Therapy
What are Stem Cells?
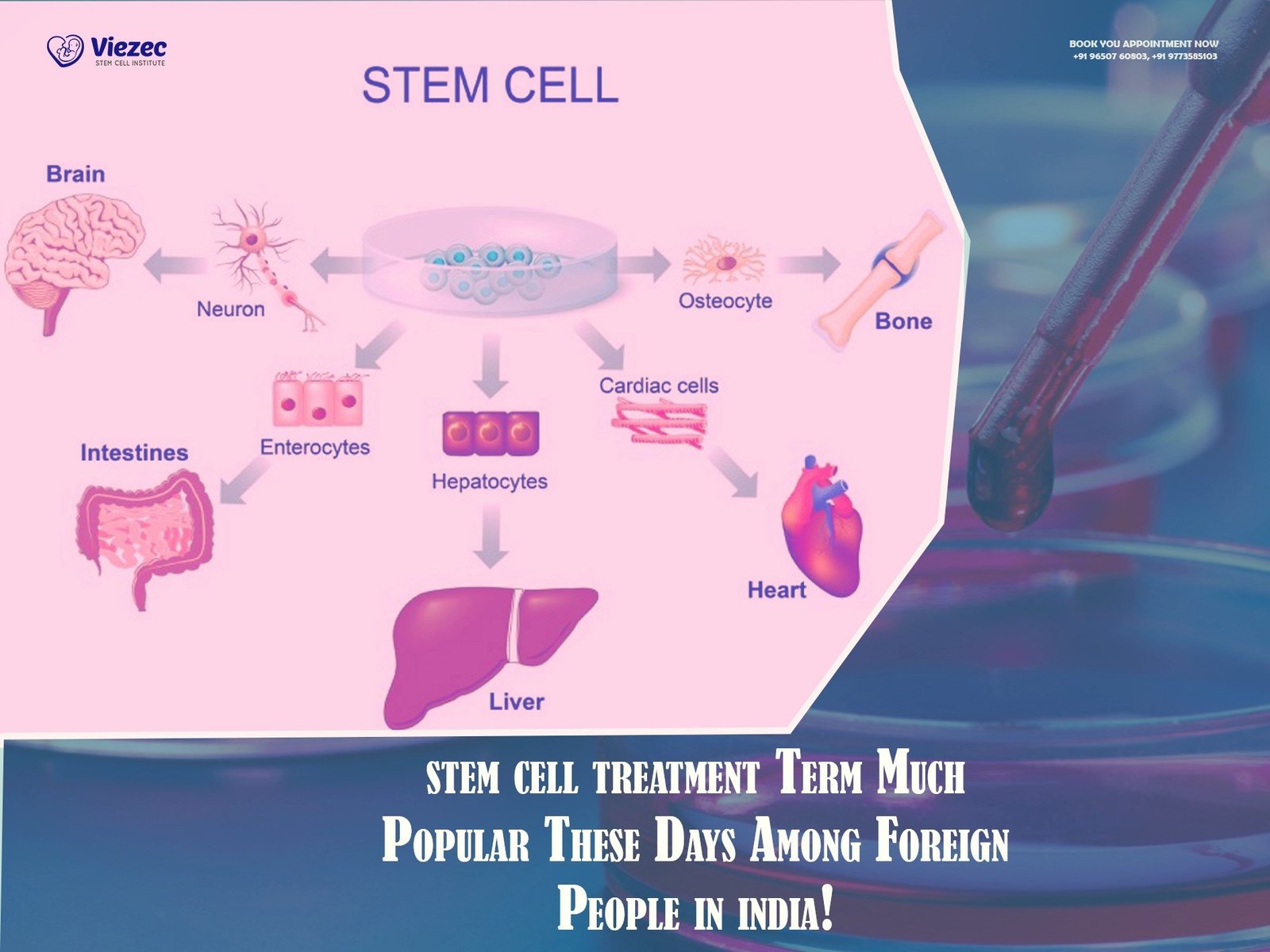
Stem cells are undifferentiated cells capable of self-renewal and differentiation into various cell types. They hold immense therapeutic potential due to their ability to regenerate damaged tissues, modulate immune responses, and promote tissue repair. Stem cells can be sourced from various tissues, including bone marrow, adipose tissue, umbilical cord blood, and embryonic tissue.
Mechanisms of Action in Atopic Dermatitis
Stem cell therapy for atopic dermatitis operates through several mechanisms:
- Immunomodulation: Stem cells possess immunomodulatory properties, which can help regulate the dysregulated immune response observed in atopic dermatitis, thereby reducing inflammation and preventing disease progression.
- Tissue Repair and Regeneration: Stem cells can differentiate into skin cells and promote tissue repair, restoring the integrity of the skin barrier compromised in atopic dermatitis.
- Anti-inflammatory Effects: Stem cells secrete various anti-inflammatory factors that suppress pro-inflammatory cytokines and promote a more balanced immune response, mitigating the inflammatory cascade characteristic of atopic dermatitis.
Types of Stem Cells Used in Therapy
Several types of stem cells have been investigated for their potential therapeutic efficacy in atopic dermatitis:
- Mesenchymal Stem Cells (MSCs): MSCs, derived from sources such as bone marrow and adipose tissue, have shown promise in preclinical studies for their immunomodulatory and regenerative properties.
- Adipose-Derived Stem Cells (ADSCs): ADSCs, isolated from adipose tissue, have demonstrated anti-inflammatory effects and the ability to promote wound healing, making them attractive candidates for atopic dermatitis therapy.
- Umbilical Cord Blood-Derived Stem Cells: Umbilical cord blood contains a rich source of hematopoietic and mesenchymal stem cells, which exhibit immunomodulatory properties and may hold therapeutic potential for atopic dermatitis.
Current Research and Clinical Trials
Preclinical Studies
Preclinical studies investigating the use of stem cells for atopic dermatitis have yielded promising results. Animal models of the disease treated with stem cell therapy have shown improvements in skin inflammation, barrier function, and overall disease severity. These studies have provided valuable insights into the mechanisms of action and potential therapeutic applications of stem cells in atopic dermatitis.
Clinical Trials
While the field of stem cell therapy for atopic dermatitis is still in its early stages, several clinical trials are underway to evaluate its safety and efficacy in human patients. These trials aim to determine the optimal cell source, dosage, and route of administration for stem cell therapy while monitoring for adverse effects and long-term outcomes. Initial results from early-phase clinical trials suggest that stem cell therapy may offer benefits in terms of symptom improvement and disease modification, although further research is needed to establish its definitive role in clinical practice.
Challenges and Considerations
Safety Concerns
One of the primary challenges in stem cell therapy is ensuring its safety, particularly regarding the risk of tumorigenesis, immunogenicity, and ectopic tissue formation. Rigorous preclinical and clinical studies are essential to evaluate the long-term safety profile of stem cell therapy in atopic dermatitis and mitigate potential risks.
Standardization and Quality Control
Standardization of stem cell manufacturing processes, including isolation, expansion, and characterization, is critical to ensure product consistency and quality. Robust quality control measures are needed to maintain the potency and viability of stem cell products throughout the manufacturing and storage process.
Regulatory Hurdles
Regulatory considerations pose challenges to the development and commercialization of stem cell therapies for atopic dermatitis. Regulatory agencies must establish clear guidelines for the approval and oversight of stem cell products, balancing the need for innovation with patient safety and ethical considerations.
Future Directions and Opportunities
Despite the challenges, stem cell therapy holds tremendous promise as a novel treatment approach for atopic dermatitis. Future research directions may include:
- Optimization of Treatment Protocols: Further optimization of stem cell therapy protocols, including cell dosage, timing, and delivery methods, to enhance therapeutic efficacy and minimize adverse effects.
- Combination Therapies: Exploration of combination therapies integrating stem cell therapy with conventional treatments or other emerging modalities to achieve synergistic effects and improve patient outcomes.
- Personalized Medicine: Advancement towards personalized medicine approaches, tailoring stem cell therapies based on individual patient characteristics, disease severity, and genetic factors to optimize treatment responses.
Make an informed Decision
Stem cell therapy represents a promising frontier in the management of atopic dermatitis, offering potential for disease modification, tissue repair, and immune modulation. While significant progress has been made in preclinical and early-phase clinical studies, numerous challenges remain to be addressed, including safety concerns, standardization, and regulatory considerations. However, with continued research efforts and collaboration between scientists, clinicians, and regulatory agencies, advanced skin disease treatments using stem cells have the potential to revolutionize the treatment landscape for atopic dermatitis, providing hope for patients with this debilitating condition.