Stem cell therapy is transforming the way we approach periodontal disease — shifting the focus from symptom management to true regeneration. Traditionally, gum disease treatments aimed to stop further damage, but they couldn’t rebuild lost bone or gum tissue. Now, with stem cells, dentistry has entered a new era of biological healing.
This article explores how stem cells work, the types used in periodontal treatment, and how they stimulate the regrowth of gums, ligaments, and bone. We compare stem cell therapy with conventional options, explain who qualifies for this innovative treatment, and break down the associated risks, costs, and accessibility in regions like India.
Whether you’re a patient looking for advanced treatment, or a healthcare provider curious about the future of periodontics, this guide offers an in-depth, reader-friendly look at how regenerative dentistry is reshaping oral health.
Introduction to Periodontal Diseases
What Are Periodontal Diseases?
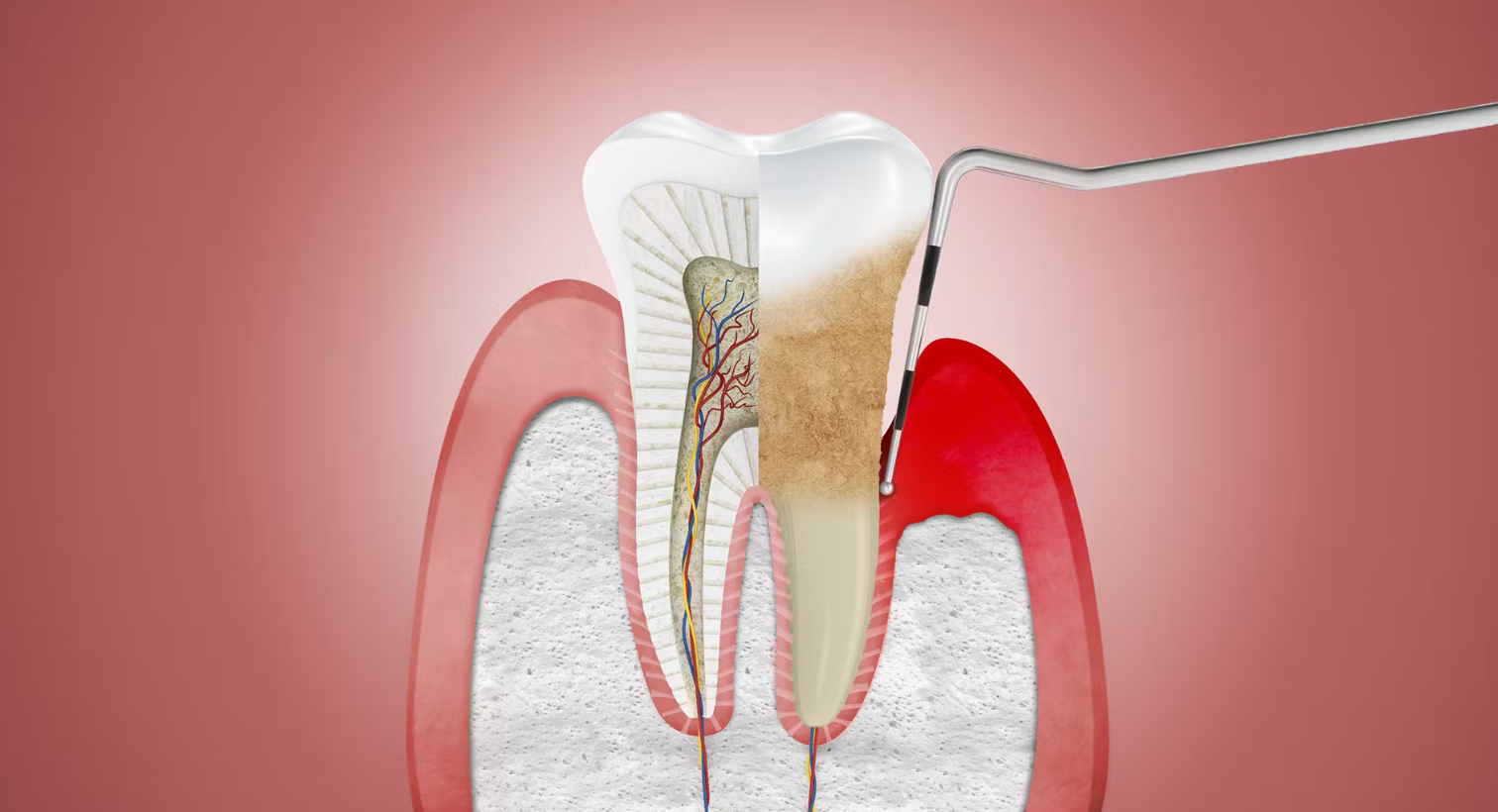
Periodontal diseases are chronic infections that damage the structures supporting your teeth — including the gums, bone, and periodontal ligament. The two most common forms are gingivitis, which causes gum inflammation, and periodontitis, a more serious stage that leads to gum recession, bone loss, and tooth loosening. If left untreated, these conditions can seriously impact your oral health, aesthetics, and even your ability to chew comfortably.
Common Causes and Risk Factors
The primary culprit behind periodontal disease is plaque — a sticky bacterial film that forms on your teeth daily. Without proper brushing and flossing, plaque hardens into tartar, which harbors harmful bacteria that trigger inflammation and infection. Several other factors can increase your risk, including:
Smoking and tobacco use
Diabetes and other chronic illnesses
Genetics and family history
Hormonal changes, especially in pregnancy or menopause
Certain medications that reduce saliva or affect gum health
Chronic stress, which weakens immune defenses
Even with good oral hygiene, your body’s unique immune response plays a major role in how aggressively gum disease develops.
The Role of Stem Cells in Dentistry
What Are Stem Cells?
Stem cells are the body’s master builders — unique cells with the extraordinary ability to divide and transform into various specialized cell types. Unlike regular cells, which have a fixed identity (like muscle or skin cells), stem cells can regenerate and become whatever the body needs, making them vital for healing and repair.
In dentistry, stem cells offer incredible potential. They can regenerate gum tissue, bone, and the periodontal ligament — all of which are typically damaged in periodontal disease. This regenerative ability is what positions stem cells at the forefront of modern dental innovation.
Types of Stem Cells Relevant to Periodontics
Several types of stem cells have shown promise in treating periodontal conditions:
-
Mesenchymal Stem Cells (MSCs): These are multipotent cells typically harvested from bone marrow, fat tissue, or umbilical cord blood. MSCs are widely used in regenerative therapies due to their ability to transform into bone, cartilage, and connective tissues, and their natural anti-inflammatory properties.
-
Dental Pulp Stem Cells (DPSCs): Extracted from the soft tissue inside your teeth — particularly wisdom or baby teeth — DPSCs are known for their high regenerative capacity and compatibility with oral tissues.
-
Gingival-Derived Mesenchymal Stem Cells (GMSCs): Found in the gums themselves, these are among the easiest to collect and show excellent results in gum and ligament regeneration, making them particularly useful for treating periodontal diseases.
How Stem Cells Aid Tissue Regeneration
Once delivered into the damaged periodontal area, stem cells don’t just sit passively. They actively communicate with the surrounding tissues and differentiate into the specific cell types needed — such as:
Osteoblasts (bone-forming cells)
Fibroblasts (connective tissue cells)
Cementoblasts (cells that help anchor teeth)
Even more impressive, stem cells release growth factors and cytokines — signaling molecules that guide the body’s natural healing systems. This not only boosts tissue regeneration but also modulates the immune response, reducing harmful inflammation and accelerating healing.
How Stem Cell Therapy Works for Periodontal Disease
Mechanism of Action in Gum and Bone Repair
Stem cell therapy for periodontal disease is designed to regenerate — not just repair — the tissues that support your teeth. Once stem cells are introduced into the affected area, they migrate to the site of damage, where they begin a complex, coordinated response:
They differentiate into essential cell types — such as osteoblasts (for bone), fibroblasts (for connective tissue), and cementoblasts (for anchoring roots).
They release bioactive molecules (growth factors, cytokines, and chemokines) that stimulate nearby dormant cells to join in the healing.
They help restore the extracellular matrix, a critical framework for holding tissues together and guiding regeneration.
Importantly, they modulate the immune system, reducing the chronic inflammation that fuels periodontitis and often hinders healing.
This two-pronged effect — regenerating structure and regulating inflammation — is what sets stem cell therapy apart from conventional periodontal treatments.
Steps Involved in the Treatment Process
Stem cell-based periodontal therapy typically follows a personalized, step-by-step clinical protocol:
-
Diagnosis and Imaging:
Your periodontist begins with a thorough evaluation using tools like X-rays, 3D imaging, and clinical measurements to map out the extent of bone or tissue loss. -
Stem Cell Harvesting:
Depending on the approach, stem cells may be taken from:-
Your own bone marrow (usually the hip)
-
Adipose (fat) tissue
-
Extracted dental pulp
-
Or, in some cases, pre-prepared donor cells
-
-
Processing and Culturing:
The harvested cells are purified, sometimes expanded in a laboratory setting, and tested for quality and sterility to ensure they are viable and safe for use. -
Delivery into the Site:
The stem cells are applied to the affected periodontal area. This can be done by:-
Injecting a stem cell suspension
-
Embedding them in a biocompatible scaffold (a matrix that holds them in place)
-
Combining with platelet-rich plasma (PRP) to enhance the healing effect
-
-
Follow-up and Monitoring:
Post-treatment, the area is regularly examined to monitor regeneration progress. Healing times vary, but many patients report visible improvements in gum coverage, bone density, and tooth stability within months.
Types of Stem Cells Used in Periodontal Treatments
Mesenchymal Stem Cells (MSCs)
Mesenchymal Stem Cells (MSCs) are among the most extensively researched and commonly used stem cells in regenerative dentistry. These multipotent cells can differentiate into a wide variety of tissue types — including bone, ligament, and connective tissue — making them ideal for rebuilding the structures affected by periodontal disease.
MSCs are typically harvested from:
Bone marrow (usually from the iliac crest)
Adipose tissue (fat deposits)
Umbilical cord tissue (in allogeneic cases)
What makes MSCs particularly valuable is their immunomodulatory ability — meaning they can reduce inflammation while simultaneously promoting tissue growth. Clinical trials have shown that MSCs can significantly improve bone regeneration, reduce pocket depth, and increase attachment levels in patients with moderate to severe periodontitis.
Dental Pulp Stem Cells and Gingival Stem Cells
Other valuable sources of stem cells come directly from the oral cavity:
-
Dental Pulp Stem Cells (DPSCs):
These are harvested from the soft tissue inside extracted teeth — especially wisdom teeth or primary (baby) teeth. DPSCs are known for their high proliferative capacity and excellent compatibility with oral environments, making them effective in regenerating both soft tissue and alveolar bone. -
Gingival Mesenchymal Stem Cells (GMSCs):
Found within the gum tissue itself, GMSCs are incredibly promising because of their accessibility, ease of harvesting, and strong anti-inflammatory properties. Studies have shown that they can play a major role in restoring gum tissue, periodontal ligament, and even cementum — the mineral layer anchoring the teeth.
What sets these dental-derived stem cells apart is that they’re readily available, require less invasive harvesting, and are tissue-specific, meaning they’re naturally predisposed to regenerate oral structures.
Clinical Benefits of Stem Cell Therapy
Regeneration of Gum and Supporting Structures
Stem cell therapy does more than halt periodontal disease — it rebuilds what was lost. Unlike conventional treatments that focus on reducing inflammation or preventing further tissue damage, stem cell therapy actively promotes the regrowth of essential structures, including:
Gum tissue
Periodontal ligament
Alveolar bone
Cementum (root surface layer)
Clinical studies have reported remarkable improvements in attachment gain, bone fill, and tooth stability following stem cell application. This means patients not only experience better oral health but also have a lower risk of tooth loss — a significant shift from managing disease to restoring function and form.
Reduced Inflammation and Faster Healing
Another major advantage is the anti-inflammatory effect of stem cells. They don’t just replace damaged cells; they also modulate the body’s immune response, calming chronic inflammation that typically fuels periodontitis. This results in:
-
Less pain, swelling, and bleeding
-
Faster tissue regeneration
-
Improved comfort and recovery after treatment
Stem cells also secrete factors that encourage nearby cells to divide and repair themselves, speeding up the natural healing cycle without the need for aggressive surgical interventions.
Long-Term Disease Control
One of the most exciting aspects of stem cell therapy is its durability. By regenerating healthy gum and bone tissue, stem cell treatment creates a more stable oral environment — one that’s less prone to recurring infection.
When paired with good oral hygiene and regular dental checkups, the benefits can last for years. In many cases, this therapy reduces the need for repeated surgical procedures and offers patients a long-term solution for maintaining gum health.
Comparing Traditional and Stem Cell-Based Treatments
Scaling and Root Planing vs Regenerative Therapy
Scaling and root planing (SRP) — often referred to as a “deep cleaning” — is the standard first-line treatment for periodontal disease. It removes plaque and tartar from below the gumline and smooths the root surfaces to reduce bacterial accumulation. While SRP can stop the progression of the disease, it does not regenerate lost tissues.
By contrast, stem cell-based regenerative therapy goes a step further. It not only halts the infection but also:
Promotes new tissue formation
Enhances bone regeneration
Stimulates periodontal ligament reattachment
Think of SRP as damage control — helpful but limited. Stem cell therapy, on the other hand, represents a true reversal of periodontal damage, offering patients the possibility of restoring a stronger and healthier periodontium.
Surgical Procedures vs Minimally Invasive Stem Cell Use
Traditional periodontal surgeries (like flap surgery, bone grafting, and guided tissue regeneration) can be effective in treating advanced cases, but they often involve:
-
Tissue cutting and sutures
-
Longer recovery periods
-
Discomfort and swelling
Stem cell therapy offers a minimally invasive alternative. In many cases, stem cells can be:
-
Injected directly into periodontal defects
-
Delivered via biocompatible scaffolds
-
Combined with PRP (Platelet-Rich Plasma) for enhanced healing
As a result, patients benefit from:
Shorter downtime
Less post-operative discomfort
More natural regeneration
For patients who want to avoid invasive surgeries — or for those who haven’t responded well to traditional approaches — stem cell therapy opens an exciting new door.
Are You a Candidate for Stem Cell Therapy?
Factors That Influence Eligibility
Stem cell therapy offers incredible promise — but it’s not a one-size-fits-all solution. Ideal candidates are those with moderate to severe periodontitis, especially when there is significant loss of gum tissue, bone, or tooth stability. You might be a strong candidate if you:
-
Have not responded well to conventional treatments
-
Are seeking a regenerative, long-term solution
-
Are in overall good health (free of uncontrolled chronic diseases)
-
Maintain good oral hygiene and are committed to aftercare
-
Do not smoke or are willing to quit, as smoking impairs healing
Dentists will often use digital imaging, clinical measurements, and sometimes biomarker analysis to determine the severity of your condition and how well you may respond to a regenerative approach.
Who Should Avoid This Treatment?
While stem cell therapy is generally safe, there are some situations where it may not be advisable. You may not be a suitable candidate if you:
Have uncontrolled diabetes or other systemic health issues that impair healing
Are undergoing immunosuppressive therapy (e.g., after organ transplant or cancer treatment)
Have active infections in the mouth or elsewhere
Are pregnant or nursing (precautionary reasons)
Have a history of autoimmune diseases affecting the oral cavity
In these cases, your periodontist may recommend stabilizing your condition with traditional methods before exploring stem cell therapy in the future.
Cost and Accessibility of Stem Cell Treatment
Average Treatment Costs
Stem cell therapy for periodontal disease is considered an advanced, specialized treatment — and naturally, that comes with a higher price tag compared to traditional dental procedures. In India, where medical innovation is growing rapidly, costs generally range from:
-
$5000 to $9,000 USD approx.)
This pricing varies based on factors like:
-
The source of stem cells (autologous vs donor-derived)
-
Whether lab culturing or scaffolds are required
-
The extent of periodontal damage
-
The reputation and location of the clinic
Although the initial cost is higher, many patients and practitioners see it as a long-term investment. By addressing the root cause and regenerating tissue, stem cell therapy may reduce the need for repeat surgeries, deep cleanings, or tooth replacements in the future.
Insurance and Availability by Region
Currently, most dental insurance policies do not cover stem cell therapy — viewing it as experimental or elective. However, this is gradually changing as more clinical trials validate its effectiveness and medical boards begin integrating regenerative treatments into standard care protocols.
As for availability, stem cell-based periodontal therapy is:
-
Readily available in major metro cities and advanced dental clinics in India
-
Less accessible in rural or small-town areas
-
Offered by select specialty centers and dental research institutions
That said, the landscape is shifting. With growing awareness, improved affordability, and broader regulatory support, stem cell treatment is expected to become more mainstream in the coming years — bringing cutting-edge care closer to everyday patients.