Stem cell therapy is rapidly gaining attention as a groundbreaking alternative to traditional treatments for hip conditions such as osteoarthritis, avascular necrosis (AVN), labral tears, and chronic inflammation. This regenerative approach taps into the body’s natural healing mechanisms, offering a non-surgical path to pain relief, joint repair, and improved mobility.
Clinical research and real-world outcomes suggest that stem cell therapy can deliver success rates ranging from 65% to over 85%, particularly in early to moderate stages of degeneration. Patients often report significant reductions in pain, increased joint function, and a delay—or even complete avoidance of hip replacement surgery.
This article explores how stem cell therapy works, the types of hip conditions it treats, what the research shows about its effectiveness, and which factors influence results. It also compares stem cell therapy to traditional treatments and highlights patient experiences from around the world, including access to advanced care through providers like Viezec in India.
If you’re searching for a future-focused, minimally invasive solution for hip pain, stem cell therapy could offer the renewal and mobility you’re looking for.
Understanding Stem Cell Therapy for Hip Conditions
What Is Stem Cell Therapy?
Stem cell therapy is a cutting-edge, regenerative treatment that taps into the body’s own healing power. By extracting stem cells typically from bone marrow or adipose (fat) tissue doctors can inject these powerful cells into damaged or degenerative areas of the hip joint. Once there, stem cells have the remarkable potential to develop into specialized tissue, like cartilage or bone, making them ideal for orthopedic repair.
Think of it as upgrading your body’s repair kit, naturally restoring structure and function without the need for invasive surgery.
How Stem Cells Support Hip Joint Healing
Stem cells don’t just fill in the gaps they actively guide healing. These cells release growth factors and anti-inflammatory signals that reduce swelling, improve circulation, and attract other repair cells to the site of injury. Over time, this can lead to the regeneration of healthy joint tissue, not just the temporary relief of symptoms.
Regeneration vs. Symptom Management
Here’s the big difference: traditional treatments like corticosteroid injections or painkillers only mask discomfort. Stem cell therapy, on the other hand, addresses the root cause. It aims to repair the joint from the inside out stimulating regrowth of damaged cartilage, reducing inflammation at its source, and slowing the progression of chronic conditions.
For patients seeking more than just a Band-Aid solution, stem cells offer hope for long-term improvement.
Types of Hip Conditions Treated with Stem Cell Therapy
Stem cell therapy isn’t a one-size-fits-all solution—it’s a tailored treatment that can address several underlying issues in the hip joint. Whether it’s worn cartilage, injured soft tissue, or disrupted blood supply, stem cells are showing promise in a range of orthopedic conditions.
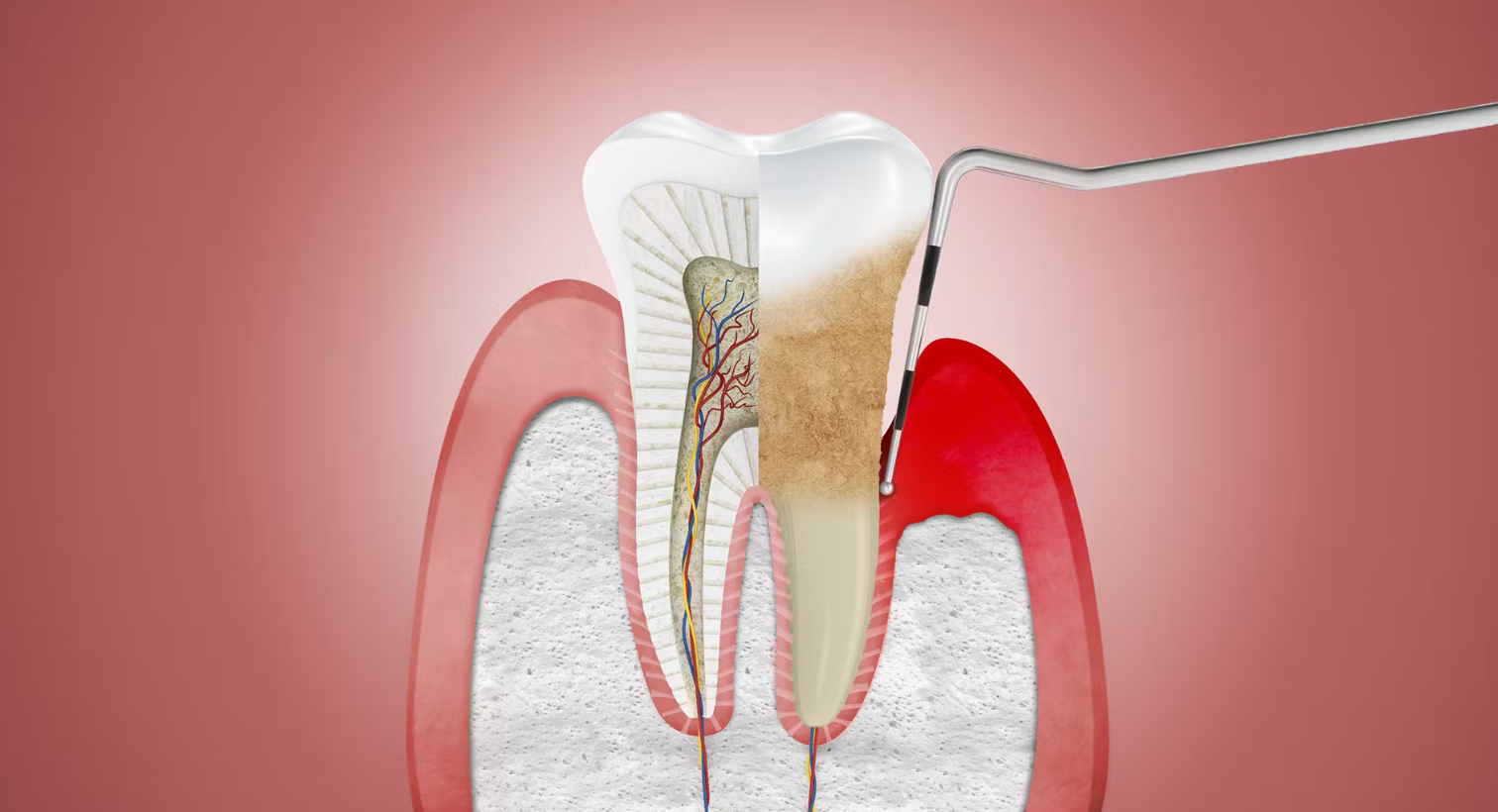
Hip Osteoarthritis
Osteoarthritis is the most common reason patients explore stem cell therapy for the hip. It’s a degenerative joint disease where the cartilage—the smooth, cushioning tissue at the ends of bones gradually breaks down, causing stiffness, pain, and reduced mobility.
Cartilage Breakdown and Joint Stiffness
Stem cell therapy may help slow the breakdown of cartilage while reducing joint inflammation. These regenerative cells can stimulate new cartilage formation or strengthen existing tissue, easing stiffness and improving function. While it may not restore the joint to its youthful state, patients often report noticeable improvements in movement and pain relief.
Hip Labral Tears
The labrum is a ring of cartilage that lines the hip socket, helping to stabilize the joint. Labral tears—common among athletes and active adults can cause sharp pain, clicking, and instability.
Stem cell injections into the damaged tissue may promote cellular healing, reducing inflammation and potentially restoring the labrum’s integrity. This makes it an appealing option for those looking to avoid arthroscopic surgery.
Avascular Necrosis (AVN)
Avascular necrosis is a serious condition where blood flow to the femoral head (the ball of the hip joint) is compromised, leading to bone tissue death. Left untreated, it can cause joint collapse and necessitate total hip replacement.
Early-stage AVN has shown excellent response to stem cell therapy. Studies have demonstrated that stem cells can encourage the growth of new blood vessels (angiogenesis) and bone cells (osteogenesis), helping to stabilize or even reverse disease progression.
Chronic Tendinopathies and Inflammation
Conditions like gluteal tendinopathy or iliopsoas tendinitis involve chronic inflammation of the soft tissues around the hip. These injuries are often slow to heal and frustratingly persistent.
Stem cell therapy has shown potential to calm chronic inflammation and support tendon regeneration, offering a non-surgical solution for pain that lingers after physical therapy or rest.
Why Patients Are Turning to Stem Cell Therapy
In recent years, more patients are leaning toward regenerative medicine especially those seeking a less invasive path to healing. Stem cell therapy isn’t just about avoiding surgery; it’s about reclaiming mobility, reducing pain, and taking control of long-term joint health in a more natural way.
Avoiding Hip Replacement Surgery
Hip replacement can be life-changing, but it’s also a major operation with a long recovery time and significant risks. For those in the early to moderate stages of joint damage, stem cell therapy offers an exciting alternative. By targeting the root of the problem, stem cells may delay or even eliminate—the need for surgery.
Patients in their 40s, 50s, or even 60s often say they’re “not ready” for a joint replacement. Stem cell therapy gives them a way to buy time while improving quality of life.
Quicker Recovery Times
Another major appeal? The recovery. Stem cell procedures are typically performed in an outpatient setting and don’t require general anesthesia or hospital stays. Most patients are up and walking the same day, with only a few days of downtime.
Compared to the months of recovery after a hip replacement, stem cell therapy feels refreshingly low-impact—literally and figuratively.
Potential for Natural Tissue Regrowth
Perhaps the most compelling reason patients choose stem cell therapy is its regenerative potential. Instead of masking the pain with temporary fixes, stem cells encourage the body to heal itself. This shift from symptom suppression to tissue restoration represents a major leap forward in orthopedic care.
It’s not just about feeling better it’s about rebuilding what’s been lost. For active people who want to stay that way, that’s a powerful motivator.
Let’s Talk Numbers – Success Rates and Outcomes
When it comes to medical decisions, outcomes matter. The good news? Stem cell therapy for hip conditions is backed by an encouraging (and growing) body of research. While results can vary from person to person, many patients are experiencing real, measurable improvements.
What Clinical Trials and Research Show
Recent studies have shown that stem cell therapy can lead to significant reductions in hip pain and improvements in joint function—especially in patients with early to moderate damage. It’s not just anecdotal; clinical trials across the U.S. and internationally are consistently reporting positive outcomes.
Improvements in Pain and Mobility Scores
Most patients begin to notice changes within a few weeks of treatment, with optimal results often developing over 3 to 6 months. Reports of 50% to 75% reductions in pain are not uncommon, and many individuals regain the ability to walk, climb stairs, or exercise with greater ease.
These improvements aren’t just physical—they’re emotional too. Regaining independence and movement has a ripple effect on mood, energy, and overall lifestyle.
Longevity of Results Over Time
One of the biggest questions people ask: How long do the results last?
While it varies depending on age, activity level, and the underlying condition, most patients report sustained benefits for 1 to 3 years. In some cases, booster treatments may be needed, especially for progressive conditions like osteoarthritis. However, even temporary regeneration can delay or prevent the need for surgery.
And the field is still evolving—new techniques in cell concentration, imaging guidance, and biologic enhancements continue to push the boundaries of what stem cell therapy can achieve.
Real-World Results and Patient Experiences
Beyond the studies and statistics, stem cell therapy shines in the stories of real people who’ve felt the difference. These firsthand accounts paint a powerful picture of what life after treatment can look like—not just improved joints, but restored freedom, confidence, and movement.
Before and After Stem Cell Injections
Many patients begin their journey with pain that disrupts daily life—whether it’s difficulty getting in and out of a car, climbing stairs, or simply standing for long periods. After treatment, these same individuals often report going from “gritting through every step” to walking comfortably again.
In clinical follow-ups, patients commonly share that pain levels dropped within a few weeks and mobility steadily returned. Even when pain isn’t fully eliminated, it’s often reduced enough to resume normal activities with far less discomfort.
Success Stories: Regaining Active Lifestyles
The most inspiring results often come from patients who were sidelined by hip issues but are now back to doing what they love:
-
A 52-year-old avid cyclist returned to biking long distances after stem cell therapy for hip osteoarthritis—avoiding the hip replacement her doctor initially recommended.
-
A retired schoolteacher with early AVN regained the ability to walk without a cane and travel again after a single round of treatment.
-
Weekend warriors, yoga enthusiasts, and grandparents chasing after grandkids all report a renewed sense of mobility and hope.
These aren’t rare miracles—they’re becoming more common as the science evolves and access improves.
Stem cell therapy is helping people not only heal but also rewrite what’s possible for their future health. That’s what makes it more than a treatment it’s a chance at transformation.
Factors That Affect the Success of Stem Cell Therapy
Not all stem cell treatments produce the same results and that’s a good thing to understand up front. Success depends on a mix of personal health factors, timing, and the specifics of how the therapy is performed. Knowing what influences your outcome can help you make the most informed choice.
Age and Health of the Patient
Stem cells are drawn from your own body, which means their regenerative capacity is influenced by your age and overall wellness. Generally, younger and healthier patients tend to have better outcomes, as their stem cells are more potent and active. However, that doesn’t mean older individuals can’t benefit—many do, especially when other factors are optimized.
Good lifestyle habits (like a healthy diet, regular movement, and avoiding smoking) also support recovery and enhance the body’s healing response after treatment.
Stage of the Hip Condition
Timing is everything. Early to moderate stages of degeneration respond best to stem cell therapy. At this point, there’s enough tissue left for stem cells to work with, and inflammation hasn’t yet reached a chronic or unmanageable stage.
If the hip joint has already collapsed or cartilage loss is severe, the likelihood of full recovery through stem cells alone is lower. However, some patients still pursue the treatment to reduce pain or delay surgery.
Type and Source of Stem Cells Used
The kind of stem cells and where they come from matters more than many patients realize.
Bone Marrow-Derived vs. Adipose-Derived Stem Cells
-
Bone marrow-derived stem cells (BMSCs) are often considered the gold standard for orthopedic conditions. They contain a higher percentage of mesenchymal stem cells (MSCs)—the type most effective in bone, cartilage, and soft tissue repair.
-
Adipose-derived stem cells (from fat tissue) are easier to harvest in larger quantities and are still biologically active. While their regenerative profile is slightly different, they’re often used when bone marrow extraction isn’t ideal or for patients with metabolic conditions.
In some cases, clinics may combine stem cells with platelet-rich plasma (PRP) to enhance healing an approach that continues to show promise in preliminary studies.
For decades, traditional treatments like pain medication, physical therapy, and eventually hip replacement have been the standard path for managing hip conditions. But now, regenerative medicine is changing that conversation offering a new lane for those who want to stay active, avoid surgery, and pursue long-term healing.
Comparing Success Rates with Hip Surgery
Let’s be honest: total hip replacement is a highly successful procedure for many patients. Studies show that 90–95% of hip replacements last 15 to 20 years, providing significant pain relief and restored function.
However, surgery isn’t always the best first step—especially for those in the earlier stages of degeneration or those looking to postpone major procedures.
By comparison, stem cell therapy has shown success rates between 65–80% for hip osteoarthritis and over 85% for early-stage avascular necrosis (AVN) in published studies. While not as definitive as joint replacement, these outcomes are meaningful—especially when you factor in the reduced risks and recovery time.
For younger patients, athletes, or anyone who’s “not quite ready” for a hip replacement, stem cells offer a valuable middle ground.
Cost, Recovery, and Risks: A Side-by-Side Look
Here’s how the two options compare on practical terms:
| Factor | Stem Cell Therapy | Hip Replacement Surgery |
|---|---|---|
| Cost | $3,000–$8,000 (often not covered by insurance) | $20,000–$40,000 (frequently covered) |
| Recovery Time | 1–4 weeks | 2–3 months |
| Procedure Risk | Low (minimally invasive, no anesthesia) | Moderate to high (infection, blood clots, etc.) |
| Hospitalization | Not required | Required (1–3 days typical) |
| Durability | 1–3 years (may require boosters) | 15–20 years |
While insurance usually covers surgery, many patients still choose stem cell therapy for the chance to heal without going under the knife—especially when they want to stay mobile and working during recovery.
What to Expect During the Process
One of the biggest advantages of stem cell therapy is how streamlined and accessible the treatment has become. If you’re considering it, knowing what to expect can make the process less intimidating and much more empowering.
The Consultation and Imaging Phase
Everything starts with a thorough evaluation. During your initial consultation, a specialist will review your symptoms, physical activity level, and medical history. Imaging—typically X-rays or an MRI—is used to assess the condition of your hip joint and determine if you’re a good candidate.
This step is crucial. The effectiveness of stem cell therapy hinges on timing so catching degeneration early enough makes a real difference in potential outcomes.
The Injection Procedure
Once you’re cleared for treatment, the actual procedure is surprisingly straightforward:
-
Stem cell harvesting: Depending on your provider, cells are collected from either bone marrow (usually from the pelvis) or adipose tissue (usually from the abdomen or thighs). This is done under local anesthesia, and it’s typically painless or mildly uncomfortable.
-
Cell processing: The harvested cells are then processed and concentrated in a lab—either in-office or off-site. This ensures a high-quality injection filled with active, regenerative cells.
-
Injection: Using real-time imaging (ultrasound or fluoroscopy), the doctor injects the stem cell concentrate directly into the damaged area of your hip joint. The procedure usually takes less than an hour from start to finish.
There’s no hospital stay, no general anesthesia, and no surgical incision. Most patients walk out the same day.
Recovery Timeline and Activity Guidelines
Recovery is where the healing truly begins:
-
First few days: You may feel some mild soreness at the injection site, but pain is typically minimal. Over-the-counter meds and light walking are usually enough to manage discomfort.
-
Week 1–2: Most patients return to desk work and light activity within days. You’ll likely be advised to avoid high-impact movements.
-
Week 3–6: Mobility starts to improve, and inflammation typically decreases. At this stage, many patients begin noticing reduced pain and smoother movement.
-
Months 3–6: This is when stem cells reach their peak effect. The regenerative process continues, and patients often report their biggest improvements in pain relief and function around this time.
Is Stem Cell Therapy Right for You?
If you’re struggling with hip pain and looking for alternatives to surgery, stem cell therapy may be a compelling option—but it’s not for everyone. Understanding your candidacy starts with asking the right questions and knowing what makes someone a good fit.
Key Questions to Ask Your Doctor
Before deciding on treatment, take these questions to your orthopedic or regenerative medicine specialist:
-
Am I a good candidate based on my diagnosis and stage of joint damage?
-
What type of stem cells will be used, and why?
-
What results can I reasonably expect based on your experience?
-
Will the procedure be image-guided for accuracy?
-
Do you recommend combining stem cell therapy with PRP or physical therapy?
The answers to these questions will help set clear expectations and ensure you’re choosing a provider who’s committed to evidence-based care.
Who’s a Good Candidate and Who Isn’t?
✅ Ideal Candidates:
-
Individuals with mild to moderate hip osteoarthritis
-
Patients with early-stage avascular necrosis (AVN)
-
Active people who want to avoid or delay surgery
-
Those who haven’t responded well to conservative treatments (like NSAIDs, physical therapy, or steroid injections)
-
Patients who are in good general health and free of serious autoimmune or metabolic conditions
⛔ Not Ideal Candidates:
-
Patients with advanced joint collapse or bone deformities
-
Individuals with severe cartilage loss or complete joint deterioration
-
People with poor overall health or compromised immune systems
-
Anyone expecting a quick fix rather than a long-term healing process
Hip Joint Stem Cell Treatment in India
If you’re considering stem cell therapy for your hip condition and exploring international options, India has emerged as a global hub for affordable, advanced regenerative treatments and Viezec is one of the country’s most trusted names in this field.
Why Choose Viezec for Stem Cell Therapy?
Viezec offers cutting-edge stem cell therapy using internationally accredited protocols, skilled specialists, and advanced medical technology all at a fraction of the cost you might pay in Western countries. They specialize in treating orthopedic conditions like hip osteoarthritis, AVN, labral tears, and chronic inflammation, offering personalized care from consultation to recovery.
What sets Viezec apart is their focus on patient-centered care, with a dedicated team that guides you through the entire journey—right from pre-treatment evaluations to post-treatment rehabilitation plans.
Benefits of Choosing Viezec in India
-
Internationally recognized stem cell protocols
-
Board-certified doctors and regenerative specialists
-
Comprehensive medical travel support (airport pickup, accommodation, translators)
-
Transparent pricing with no hidden costs
-
Ethically sourced stem cells, handled under strict quality standards
Take the First Step Toward Healing
Viezec has helped hundreds of international patients regain their mobility and reduce pain without the need for joint replacement surgery. Whether you’re looking to delay surgery or restore your quality of life naturally, their team can help you explore whether stem cell therapy is right for you.
To learn more about treatment options or schedule a consultation, visit www.viezec.com or reach out directly to their patient care team for guidance.