Orthopedic conditions such as arthritis, joint degeneration, tendon injuries, and cartilage damage affect millions of people worldwide. Traditional treatments—like pain medications, physical therapy, or even surgery—often provide temporary relief but may not fully restore damaged tissues. This has led both doctors and researchers to explore more advanced, regenerative approaches — and that’s where stem cell therapy is showing promising results.
Stem cells are unique cells with the remarkable ability to develop into various specialized cell types such as bone, cartilage, or muscle cells. In orthopedic medicine, they are being studied and used to repair, regenerate, and restore tissues that were once thought irreparable. From easing chronic joint pain to potentially delaying the need for joint replacement, stem cell–based therapies are at the frontier of modern orthopedic care.
However, not all stem cells are the same. Different types of stem cells have distinct properties, sources, and therapeutic potential — and understanding these differences is essential for patients considering regenerative treatment.
In this article, we’ll clearly explain the best types of stem cells used in orthopedic conditions, how each one works, and what current scientific evidence says about their effectiveness. Whether you’re a patient researching treatment options or a healthcare professional looking to stay informed, this guide will help you understand the real potential — and the limitations — of stem cell therapy in orthopedics.
Key Takeaways
- 01. Stem cells help regenerate damaged tissues, reduce inflammation, and improve joint mobility.
- 02. Mesenchymal stem cells (MSCs) are the most widely used in orthopedic therapy for bone, cartilage, and tendon repair.
- 03. Safety, transparency, and doctor expertise are critical when selecting a stem cell clinic.
- 04. Always choose providers that follow guidelines and use GMP-certified labs for cell processing.
- 05. Combine therapy with physical rehabilitation, good nutrition, and post-treatment carefor the best outcomes.
Understanding Stem Cells in Orthopedics
To understand why stem cells are being called the future of orthopedic care, it’s important to know what makes them so special. Stem cells are the body’s raw materials — undifferentiated cells capable of developing into many different cell types, such as bone cells (osteoblasts), cartilage cells (chondrocytes), or muscle cells (myocytes). This unique ability allows them to play a crucial role in tissue regeneration and healing.
How Stem Cells Help in Orthopedic Repair
When bones, tendons, or joints are injured, the body’s natural repair mechanisms can be limited—especially with age or in chronic conditions like osteoarthritis. Stem cells, when introduced into damaged tissues, may help by:
-
Reducing inflammation in affected joints and soft tissues
-
Stimulating new cell growth and collagen production
-
Supporting tissue repair and regeneration of cartilage, bone, or ligament
-
Improving local blood flow, which aids in healing
-
Releasing growth factors and cytokines that enhance recovery
These properties make stem cell therapy a potential game-changer in treating orthopedic conditions such as knee osteoarthritis, tendon injuries, ligament tears, and non-healing bone fractures.
Types of Stem Cells Used in Orthopedic Medicine
In orthopedic treatments, doctors typically work with adult stem cells rather than embryonic ones. Adult stem cells are derived from sources such as bone marrow, fat tissue (adipose), or umbilical cord blood. These cells are valued for being safe, ethical, and capable of differentiating into musculoskeletal tissue types.
Each source has its own benefits and clinical applications — which we’ll explore in the next section.
Why Understanding Cell Type Matters
Different stem cell types vary in potency, availability, and effectiveness for certain orthopedic issues. For example, bone marrow–derived cells may be better for bone healing, while adipose-derived cells might excel in soft tissue repair. Choosing the right type is essential for better treatment outcomes, which is why patients should always consult with experienced regenerative medicine specialists.
Major Types of Stem Cells Used in Orthopedic Treatments
Stem cell–based orthopedic therapies use several different types of cells — each with unique origins, biological characteristics, and healing potential. Understanding the differences helps patients and clinicians choose the most appropriate option based on the condition being treated and the desired outcome.
Below are the most common and clinically studied stem cell types used in orthopedic and regenerative medicine.
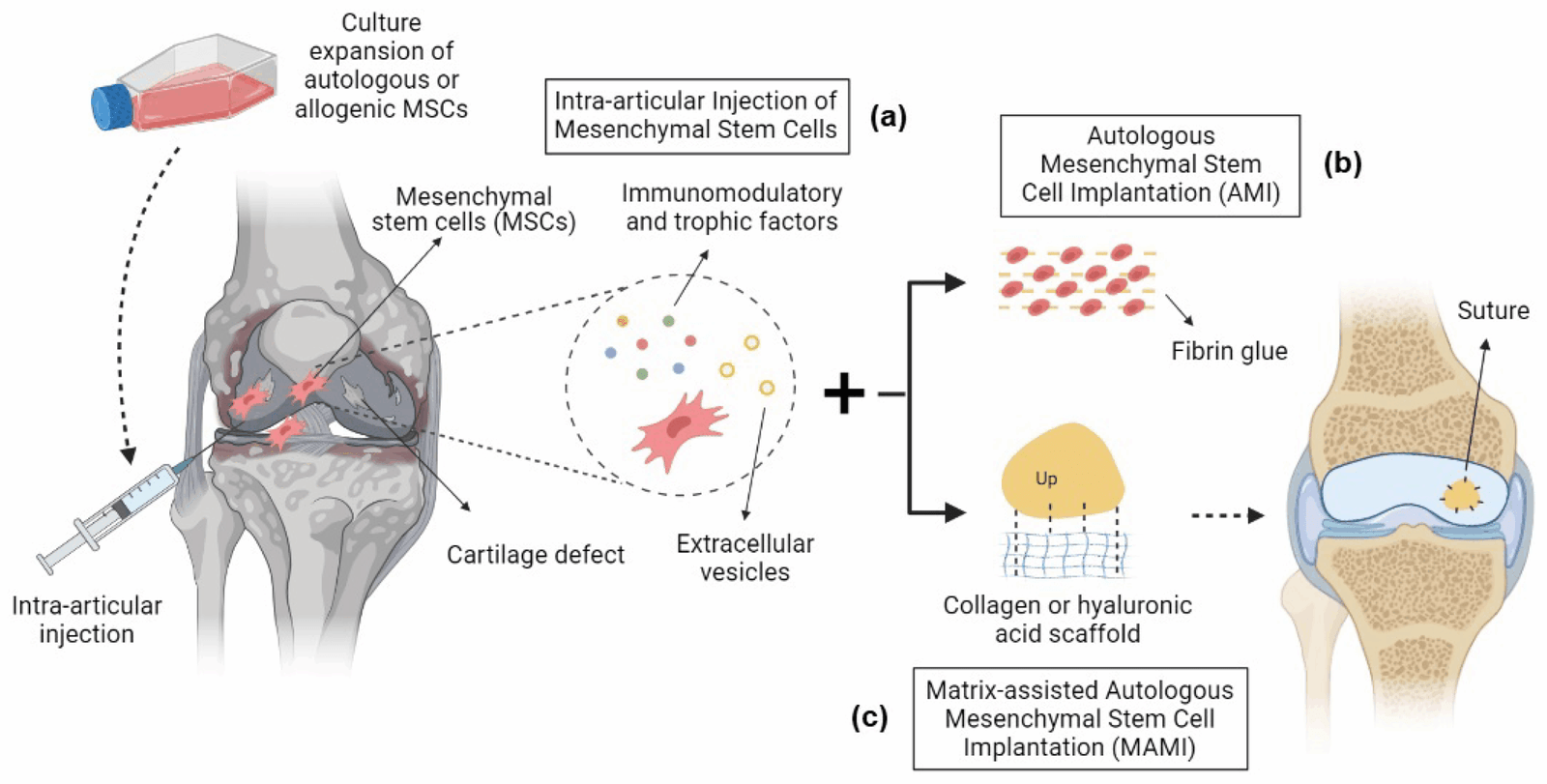
Mesenchymal Stem Cells (MSCs)
Mesenchymal stem cells, or MSCs, are the most widely researched and commonly used type of stem cells in orthopedic applications. These cells are multipotent, meaning they can differentiate into several musculoskeletal tissues, including bone, cartilage, tendon, and muscle.
Sources: Bone marrow, adipose tissue, umbilical cord tissue, and amniotic membrane.
Key Benefits:
-
Promote cartilage and bone regeneration
-
Reduce joint inflammation and pain
-
Support healing of tendons and ligaments
-
Safe and non-controversial (derived from adult tissues)
Common Uses: Knee osteoarthritis, rotator cuff tears, meniscus injuries, and chronic tendonitis.
Bone Marrow–Derived Stem Cells (BMSCs)
These stem cells are harvested from a patient’s bone marrow, usually from the hip bone (iliac crest). They have been used for decades in orthopedic and sports medicine procedures.
How They Work:
Bone marrow–derived stem cells help stimulate bone and cartilage repair and are rich in growth factors that aid tissue healing.
Advantages:
-
Clinically established and well-studied
-
Effective in bone healing and cartilage regeneration
-
Can be used in autologous (self-donated) procedures, reducing rejection risk
Limitations:
-
Invasive harvesting process
-
Cell yield may be lower in older patients
Ideal For: Bone fractures, joint cartilage damage, and early-stage osteoarthritis.
Adipose-Derived Stem Cells (ADSCs)
Adipose-derived stem cells are extracted from fat tissue, typically through a minimally invasive liposuction procedure. They are rich in regenerative and anti-inflammatory properties.
Advantages:
-
Abundant and easy to collect
-
High stem cell concentration compared to bone marrow
-
Strong anti-inflammatory and tissue-repair potential
Ideal For: Soft tissue injuries, tendon and ligament repair, and joint inflammation control.
Note: ADSCs are gaining popularity in clinics because of their accessibility and safety profile.
Umbilical Cord–Derived Stem Cells (UC-MSCs)
Umbilical cord–derived mesenchymal stem cells are collected from donated umbilical cords after childbirth. These cells are young, highly potent, and immune-privileged, meaning they are less likely to cause rejection.
Benefits:
-
High regenerative capacity
-
Non-invasive source (donor-derived)
-
Lower inflammatory response compared to adult stem cells
Applications: Early research shows promise for treating joint degeneration, cartilage defects, and ligament injuries.
Note: While widely used in research and some clinical trials, UC-MSC use in orthopedic treatments is still regulated differently in each country.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells are lab-engineered cells created by reprogramming adult cells (like skin or blood cells) back into a stem-like state. These cells can theoretically transform into any cell type in the human body.
Advantages:
-
Unlimited potential for tissue engineering
-
No ethical concerns like embryonic stem cells
-
Can be patient-specific (autologous)
Challenges:
-
High cost and complex production process
-
Still in early research for orthopedic use
-
Requires strict laboratory and regulatory oversight
Potential Uses: In the future, iPSCs could help rebuild complex tissues such as cartilage and intervertebral discs.
Summary Table: Stem Cell Types in Orthopedics
| Stem Cell Type | Source | Best For | Key Benefit |
|---|---|---|---|
| Mesenchymal (MSCs) | Bone marrow, fat, cord tissue | Bone, cartilage, tendon repair | Multipotent, safe, widely used |
| Bone Marrow–Derived | Bone marrow | Bone and cartilage regeneration | Clinically proven, autologous |
| Adipose-Derived | Fat tissue | Joint and tendon repair | Abundant, easy to harvest |
| Umbilical Cord–Derived | Cord tissue after birth | Joint degeneration, ligament healing | Young, potent, immune-friendly |
| Induced Pluripotent (iPSCs) | Lab-engineered | Experimental tissue regeneration | Unlimited differentiation potential |
Comparing Stem Cell Types — Which Is Best for Specific Orthopedic Conditions
Not all stem cells act the same way or are equally effective for every orthopedic problem. The success of stem cell therapy depends on the type of cell used, the condition being treated, and the patient’s overall health.
Below is a detailed comparison showing which stem cell types have shown the most promise for common orthopedic disorders.
Knee Osteoarthritis and Cartilage Damage
Best Options:
-
Bone Marrow–Derived Stem Cells (BMSCs)
-
Adipose-Derived Stem Cells (ADSCs)
-
Umbilical Cord–Derived MSCs (UC-MSCs)
How They Help:
Stem cells injected into arthritic joints can reduce inflammation, promote cartilage regeneration, and improve joint lubrication.
-
BMSCs are effective in stimulating new cartilage formation.
-
ADSCs provide strong anti-inflammatory support and are easier to harvest.
-
UC-MSCs (from cord tissue) show excellent potential in early-stage arthritis for tissue regeneration and pain reduction.
Evidence Snapshot:
Several clinical studies report improved pain scores, mobility, and cartilage thickness in patients with mild to moderate osteoarthritis after stem cell therapy.
Tendon and Ligament Injuries (e.g., Rotator Cuff, ACL Tears)
Best Options:
-
Mesenchymal Stem Cells (MSCs) from bone marrow or adipose tissue
How They Help:
MSCs release growth factors and cytokines that encourage new collagen formation — essential for strong, flexible tendons and ligaments.
-
They also reduce scar tissue formation and enhance natural repair.
-
Commonly used in rotator cuff tears, Achilles tendonitis, and ACL injuries.
Non-Healing Bone Fractures and Delayed Union
Best Options:
-
Bone Marrow–Derived Stem Cells (BMSCs)
-
Induced Pluripotent Stem Cells (iPSCs) (experimental)
How They Help:
Bone marrow cells can differentiate directly into osteoblasts, the cells responsible for bone formation.
In stubborn fractures or bone non-unions, BMSCs are often combined with bone grafts or scaffolds to enhance regeneration.
iPSCs are being studied for engineered bone tissue, though still in research phases.
Spine and Disc Degeneration
Best Options:
-
Mesenchymal Stem Cells (MSCs) from bone marrow or umbilical cord
How They Help:
Spinal disc degeneration is caused by loss of cells and hydration in the intervertebral discs.
MSCs help by:
-
Restoring disc cell population
-
Improving hydration and cushioning
-
Reducing inflammation in the spinal environment
Sports Injuries and Muscle Tears
Best Options:
-
Adipose-Derived Stem Cells (ADSCs)
-
Bone Marrow–Derived MSCs
How They Help:
Athletes benefit from stem cell therapies for quicker recovery and reduced inflammation.
ADSCs have a high regenerative factor and can accelerate muscle fiber repair and tendon regeneration after strain injuries.
Quick Comparison Table: Best Stem Cells for Common Orthopedic Conditions
| Orthopedic Condition | Best Stem Cell Type(s) | Key Therapeutic Effect |
|---|---|---|
| Knee Osteoarthritis | Bone Marrow, Adipose, Umbilical Cord MSCs | Cartilage regeneration, pain relief |
| Tendon/Ligament Injuries | MSCs (Bone Marrow/Adipose) | Collagen repair, tissue regeneration |
| Bone Fractures | Bone Marrow MSCs, iPSCs (research) | Bone formation and union |
| Spine Degeneration | Bone Marrow or Cord MSCs | Disc repair, anti-inflammatory |
| Sports Injuries | Adipose MSCs, Bone Marrow MSCs | Muscle and tendon repair |
Key Takeaway
There’s no single “best” stem cell for every patient or condition. Instead, treatment success depends on matching the right cell type to the right orthopedic need, using clinically validated methods under professional guidance. Consulting with a qualified regenerative medicine specialist ensures safety, appropriate dosing, and realistic expectations.
Clinical Evidence and Research Updates
When considering stem cell therapies for orthopedic conditions, it’s essential to base decisions on the best available clinical evidence, understand where the science is well-established and where it remains investigational, and recognise the gaps in knowledge. This section summarises major findings from recent research, highlights what is known about safety and efficacy, and points out where further work is needed.
What the Evidence Shows
-
Multiple systematic reviews and meta-analyses show that therapies using Mesenchymal Stem Cells (MSCs) can be safe and feasible for musculoskeletal use — for example, in conditions such as osteoarthritis, cartilage defects and bone repair.
-
One review found MSC-based therapies relieved pain in patients with knee osteoarthritis, but the evidence of improved knee function or cartilage repair remains limited.
-
Other recent work indicates that stem-cell therapies in orthopaedics (including bone defects, tendon injuries, non-unions) are rising in research interest and showing promise for regeneration and improved healing outcomes.
-
For example: “Clinical studies have demonstrated the safety and feasibility of MSC-based therapies for conditions like osteoarthritis, with improvements in pain reduction and function observed in many cases.”
Key Highlights from Recent Studies
-
A systematic review in 2023 found that while stem-cell therapy reduced pain in some patients, improvements in knee function and cartilage repair were not reliably demonstrated across trials.
-
A review of MSCs in orthopaedics concluded that these cells showed successful and safe use in multiple applications (cartilage, osteonecrosis) but emphasised the need for standardised cell-characterisation and robust clinical studies.
-
A regulatory overview noted that although MSCs differentiate into musculoskeletal tissues (bone, cartilage, ligament) and have immunomodulatory functions, their clinical use in orthopaedics remains “active research” rather than established therapy.
What This Means for Patients & Clinicians
-
Patients should be informed: Stem cell therapy may offer pain relief and some functional improvement—but it is not yet a guaranteed cure for all orthopedic conditions.
-
Clinic or provider selection matters: Therapies that are well-designed, conducted within clinical trials or regulated environments, with transparent reporting, offer higher assurance of quality and safety.
-
Maintenance and follow-up are important: Because long-term durability is uncertain, real-world outcomes must be monitored; combining stem cell therapy with physical rehabilitation and lifestyle measures often yields better results.
-
Stay updated: The field is evolving rapidly—new trials, longer follow-ups, improved cell processing methods and delivery systems are emerging, so what is considered “standard” now may change in a few years.
Key Benefits of Stem Cell Therapy in Orthopedic Conditions
1. Natural Tissue Regeneration
Stem cells have the remarkable ability to differentiate into bone, cartilage, muscle, and tendon cells. This allows them to potentially repair or replace damaged tissues rather than merely relieving symptoms.
Example: In osteoarthritis or meniscus injuries, stem cells may stimulate cartilage regrowth and improve joint cushioning — offering long-term relief.
2. Reduction in Pain and Inflammation
Stem cells secrete anti-inflammatory molecules and growth factors that help reduce chronic joint inflammation. Many patients report gradual pain reduction and improved mobility within months of treatment.
3. Minimally Invasive and Low Recovery Time
Most stem cell procedures are performed via injections, often using a patient’s own cells (autologous). This means shorter recovery times, lower risk of surgical complications, and minimal hospital stay.
4. Delay or Prevention of Surgery
For patients with mild to moderate joint degeneration, stem cell therapy can delay the need for joint replacement surgery or other invasive interventions, preserving natural tissue for as long as possible.
5. Personalized, Biologic Healing
Because stem cells can be harvested from the patient’s own bone marrow or fat tissue, they provide a personalized regenerative solution with a very low risk of immune rejection.
Key Factors to Consider When Choosing a Stem Cell Clinic
Medical Expertise and Credentials
Always confirm that the treatment is conducted under the supervision of qualified orthopedic or regenerative medicine specialists.
Look for clinics that:
-
Employ board-certified doctors with proven experience in cell therapy
-
Work in partnership with accredited hospitals or research institutions
-
Offer a clear, science-backed treatment protocol
At Viezec — one of India’s trusted regenerative medicine providers — all treatments are overseen by experienced clinicians specializing in orthopedics and cell-based therapies, ensuring that every procedure meets international medical standards.
Source and Quality of Stem Cells
Ask where the stem cells come from — whether they are:
-
Autologous (from the patient’s own bone marrow or fat tissue), or
-
Allogeneic (from donated umbilical cord or other safe, ethical sources)
Reputable providers like Viezec ensure that all cells are ethically sourced, tested for sterility and viability, and processed in GMP-certified laboratories following strict safety protocols.
Transparency of Treatment Plan
A trustworthy clinic will always:
-
Explain the type of stem cells being used
-
Provide clear pre- and post-treatment guidelines
-
Set realistic expectations rather than guaranteeing miraculous results
At Viezec, each patient receives a personalized treatment plan tailored to their specific orthopedic condition, medical history, and recovery goals.
Regulatory Compliance and Ethics
Avoid clinics that:
-
Promise instant or guaranteed cures
-
Refuse to share data or scientific references
-
Operate without medical oversight
Choose facilities that comply with global regenerative medicine regulations. Viezec adheres to ethical standards and transparent communication, ensuring patients are fully informed before treatment.
Patient Support and Aftercare
Post-procedure care is crucial for success. Look for centers that provide:
-
Follow-up evaluations
-
Physical therapy support
-
Rehabilitation guidance
-
Long-term progress tracking
Viezec’s dedicated patient care team provides continuous follow-up support, helping patients recover safely and monitor long-term improvement.
⚠️ Red Flags to Watch Out For
-
Unrealistic claims such as “100% guaranteed results”
-
No mention of doctor names or credentials
-
Lack of published results or data
-
No formal consent process
-
One-size-fits-all treatment plans
Remember: credible stem cell providers emphasize safety, evidence, and individualized care, not hype.
Why India Is Emerging as a Global Hub for Stem Cell Therapy
India is becoming one of the top destinations for affordable and advanced stem cell treatments. The combination of skilled specialists, advanced technology, and cost-effective care makes it attractive for both domestic and international patients.
Institutions like Viezec in New Delhi have contributed significantly to this growth by offering world-class facilities and transparent treatment practices to patients from over 50 countries.
Conclusion
Stem cell therapy has opened a new chapter in orthopedic and regenerative medicine, offering hope to patients suffering from chronic joint pain, cartilage damage, tendon tears, and degenerative bone diseases. Unlike conventional treatments that only manage symptoms, stem cells aim to repair and regenerate the damaged tissues naturally.
Through this guide, we’ve learned that not all stem cells are the same — mesenchymal stem cells (MSCs) from bone marrow, adipose tissue, and umbilical cord are currently the most promising for orthopedic applications. Each type offers unique strengths, and the success of therapy largely depends on the quality of cells, the expertise of the doctors, and the clinical environment where treatment is performed.
FAQs
The most effective stem cells for orthopedic conditions are mesenchymal stem cells (MSCs) — commonly derived from bone marrow, adipose (fat) tissue, or umbilical cord blood. These cells can regenerate cartilage, tendons, and bone, making them ideal for treating joint and musculoskeletal problems.
When performed by qualified doctors in regulated clinics, stem cell therapy is generally safe. Providers like Viezec use GMP-certified labs and adhere to international guidelines to ensure ethical and sterile procedures.
Most patients notice improvements in pain, stiffness, and mobility within 2 to 3 months, depending on the severity of their condition. Full healing and tissue regeneration can continue for up to 6–12 months post-treatment.
Stem cell therapy cannot “cure” arthritis permanently, but it can significantly reduce pain, improve joint function, and delay or avoid surgery in many patients. Results depend on factors like age, damage level, and overall health.
Studies suggest 60–80% of patients experience measurable improvement in pain and function after stem cell therapy for orthopedic conditions. Clinics like Viezec track outcomes through imaging and clinical evaluation to ensure transparency.
Unlike surgery, stem cell therapy is minimally invasive and aims to repair and regenerate tissues naturally. There’s no major incision, fewer risks, and a shorter recovery time. It focuses on healing rather than replacement.
In India, the overall expense for stem cell therapy varies based on the treatment type, stem cell source, and condition severity. Viezec offers personalized and affordable treatment plans that maintain high medical standards and provide excellent value compared to Western countries.
Stem cell therapy may not be suitable for patients with active cancer, severe infection, bleeding disorders, or autoimmune complications. A certified regenerative medicine specialist should always review your medical history before proceeding.