Multiple Sclerosis (MS) and Amyotrophic Lateral Sclerosis (ALS) are two neurological diseases that, while different in their pathophysiology and progression, have significant impacts on the lives of those affected. Understanding the symptoms, diagnosis, and treatment options for these conditions is crucial for patients, caregivers, and healthcare providers. This article provides a comprehensive comparison of MS and ALS, focusing on their symptoms, diagnostic procedures, underlying mechanisms, and treatment approaches, including the emerging role of stem cell therapy.
Overview of Multiple Sclerosis (MS)
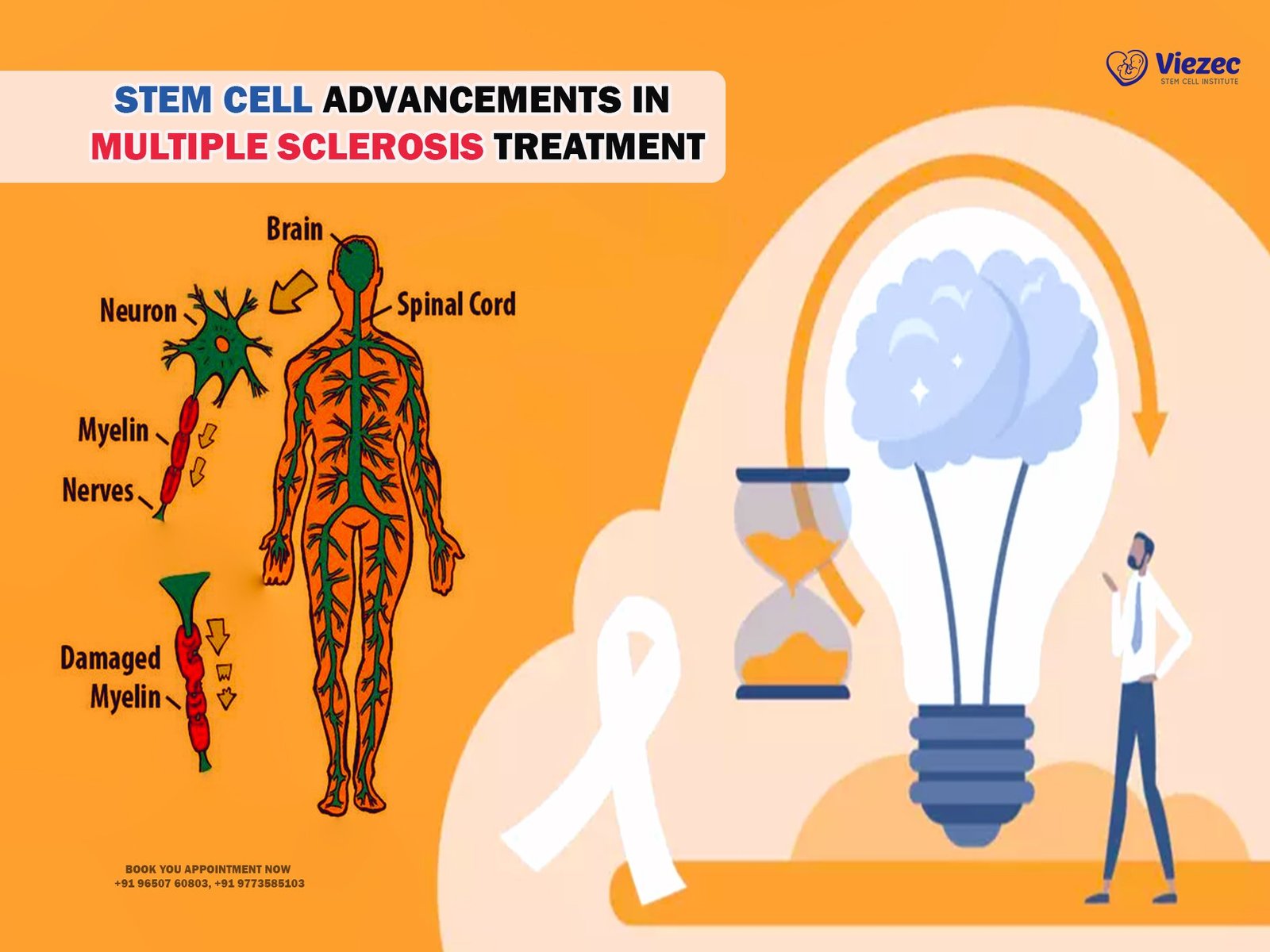
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, particularly the brain and spinal cord. The condition is characterized by the immune system mistakenly attacking the myelin sheath, a protective covering of nerve fibers, leading to inflammation and scar tissue formation, known as sclerosis. This damage disrupts the communication between the brain and the rest of the body, resulting in a wide range of neurological symptoms. MS can present in various forms, including relapsing-remitting MS (RRMS), primary progressive MS (PPMS), secondary progressive MS (SPMS), and progressive-relapsing MS (PRMS). Each type has a different pattern of disease progression and symptom severity.
Overview of Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that primarily affects motor neurons responsible for voluntary muscle movements. The degeneration of these neurons leads to muscle weakness, atrophy, and eventually, paralysis. ALS is classified into two main types: sporadic ALS, which occurs randomly and accounts for the majority of cases, and familial ALS, which is inherited and constitutes a smaller percentage of cases. The disease progression in ALS is typically rapid, with most patients experiencing significant disability and a reduced life expectancy. ALS affects the ability to speak, swallow, and breathe, making it a particularly devastating condition.
Symptoms Comparison
Early Symptoms of Multiple Sclerosis (MS)
Early symptoms of Multiple Sclerosis (MS) can be subtle and vary widely among individuals. Common initial signs include fatigue, numbness or tingling in the limbs, weakness, and visual disturbances such as double vision or optic neuritis. Other early symptoms may involve difficulty with coordination and balance, muscle spasms, and cognitive changes like memory problems or difficulty concentrating. These symptoms often appear during the relapsing-remitting phase of the disease, where they can come and go, sometimes remaining dormant for months or years before reappearing. Early recognition and diagnosis are crucial for managing MS and initiating treatment to slow disease progression.
Early Symptoms of Amyotrophic Lateral Sclerosis (ALS)
The early symptoms of Amyotrophic Lateral Sclerosis (ALS) are often subtle and can be easily overlooked. Initial signs typically include muscle weakness or stiffness, which may be localized to one part of the body, such as the hands, arms, legs, or the muscles involved in speech and swallowing. Patients may experience muscle cramps or twitches (fasciculations) and notice a gradual loss of strength and coordination. As the disease progresses, these symptoms become more pronounced and widespread, leading to significant impairment in motor functions. Early detection of ALS is essential for managing the disease and exploring treatment options that can potentially slow its progression.
Progression of Symptoms in MS
The progression of symptoms in Multiple Sclerosis (MS) can vary significantly depending on the type of MS and individual patient factors. In relapsing-remitting MS (RRMS), patients experience episodes of symptom exacerbation (relapses) followed by periods of partial or complete recovery (remissions). Over time, these relapses may lead to cumulative neurological damage and progression to secondary progressive MS (SPMS), characterized by a steady worsening of symptoms without distinct relapses. Primary progressive MS (PPMS) involves a continuous decline in neurological function from the onset, with no relapses or remissions. Symptoms that may worsen over time include mobility issues, muscle spasticity, pain, and cognitive impairment, severely impacting the patient’s quality of life.
Progression of Symptoms in ALS
The progression of symptoms in Amyotrophic Lateral Sclerosis (ALS) is typically rapid and relentless. As the disease advances, muscle weakness spreads from its initial location to other parts of the body, leading to widespread muscle atrophy and loss of motor function. Patients may lose the ability to perform daily activities independently, such as walking, speaking, swallowing, and eventually breathing. Respiratory failure is the most common cause of death in ALS, often occurring within three to five years after the onset of symptoms. However, the rate of progression can vary, and some patients may live longer with proper medical care and supportive therapies. Despite the rapid decline, maintaining quality of life through palliative care and symptom management is a crucial aspect of ALS treatment.
Diagnosis
Diagnostic Procedures for Multiple Sclerosis (MS)
Diagnosing Multiple Sclerosis (MS) involves a combination of clinical evaluation, imaging studies, and laboratory tests. Neurologists often begin with a thorough medical history and physical examination to identify characteristic symptoms and neurological deficits. Magnetic Resonance Imaging (MRI) is the primary imaging tool used to detect lesions or plaques in the brain and spinal cord, indicative of MS. Additional tests may include lumbar puncture (spinal tap) to analyze cerebrospinal fluid for signs of inflammation or abnormal immune activity, and evoked potentials to assess the electrical activity of the brain in response to stimuli. A diagnosis of MS requires evidence of disease activity in different parts of the central nervous system over time.
Diagnostic Procedures for Amyotrophic Lateral Sclerosis (ALS)
The diagnosis of Amyotrophic Lateral Sclerosis (ALS) is primarily clinical, based on a detailed medical history, physical examination, and ruling out other conditions with similar symptoms. Electromyography (EMG) and nerve conduction studies (NCS) are essential tests that measure the electrical activity of muscles and nerves, helping to confirm the presence of motor neuron degeneration. MRI scans may be used to exclude other neurological disorders. Blood tests and genetic testing can identify familial ALS or exclude other causes of motor neuron disease. A definitive ALS diagnosis relies on the progressive spread of symptoms and signs of upper and lower motor neuron involvement in multiple regions of the body.
Pathophysiology
Underlying Mechanisms of Multiple Sclerosis (MS)
The underlying mechanisms of Multiple Sclerosis (MS) involve an abnormal immune response that targets the central nervous system. The immune system mistakenly attacks the myelin sheath, the protective layer surrounding nerve fibers, leading to inflammation, demyelination, and subsequent formation of scar tissue (sclerosis). This process disrupts the normal transmission of electrical impulses along the nerves, resulting in the neurological symptoms of MS. The exact cause of this immune dysfunction is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental factors, such as viral infections or vitamin D deficiency, that trigger the autoimmune response.
Underlying Mechanisms of Amyotrophic Lateral Sclerosis (ALS)
The underlying mechanisms of Amyotrophic Lateral Sclerosis (ALS) involve the degeneration of motor neurons in the brain and spinal cord. This degeneration leads to the progressive loss of muscle control and function. The exact cause of ALS remains unclear, but several factors are believed to contribute to the disease process, including genetic mutations, oxidative stress, mitochondrial dysfunction, and abnormal protein aggregation. In familial ALS, specific genetic mutations have been identified that affect various cellular pathways. In sporadic ALS, the causes are more heterogeneous and may involve a complex interplay of genetic and environmental factors. The result is the selective death of motor neurons, leading to muscle weakness, atrophy, and paralysis.
Treatment Options
Current Treatment Approaches for Multiple Sclerosis (MS)
Disease-modifying Therapies
Disease-modifying therapies (DMTs) are the cornerstone of Multiple Sclerosis (MS) treatment. These medications aim to reduce the frequency and severity of relapses, slow the progression of disability, and limit the formation of new lesions in the central nervous system. Commonly used DMTs include interferon beta, glatiramer acetate, and newer agents like natalizumab, fingolimod, and ocrelizumab. These drugs modulate the immune response to prevent the autoimmune attacks on myelin. Early initiation of DMTs is crucial for improving long-term outcomes in MS patients.
Symptomatic Management
In addition to DMTs, symptomatic management plays a vital role in the comprehensive care of MS patients. This approach addresses the wide range of symptoms associated with MS, such as fatigue, pain, spasticity, bladder and bowel dysfunction, and cognitive impairment. Pharmacological treatments, physical therapy, occupational therapy, and psychological support are all essential components of symptomatic management. Tailoring these interventions to the individual needs of each patient can significantly enhance their quality of life and functional abilities.
Emerging Therapies and Research
Ongoing research in Multiple Sclerosis (MS) is focused on developing new therapies that target different aspects of the disease. Emerging treatments include oral medications, monoclonal antibodies, and remyelination therapies aimed at repairing damaged myelin and restoring nerve function. Clinical trials are exploring the efficacy and safety of these novel approaches. Additionally, research into the genetic and environmental factors contributing to MS may lead to more personalized and effective treatment strategies in the future.
Current Treatment Approaches for Amyotrophic Lateral Sclerosis (ALS)
Riluzole and Edaravone
Riluzole and edaravone are the only FDA-approved medications for Amyotrophic Lateral Sclerosis (ALS). Riluzole is believed to reduce the release of glutamate, a neurotransmitter that can cause motor neuron damage, thereby slowing disease progression and extending survival. Edaravone, an antioxidant, is thought to reduce oxidative stress and delay the decline in daily functioning. While these drugs do not cure ALS, they can modestly slow its progression and improve patients’ quality of life.
Supportive Care and Symptom Management
Supportive care and symptom management are critical components of ALS treatment. Multidisciplinary care teams, including neurologists, physical therapists, occupational therapists, speech therapists, and nutritionists, work together to address the diverse needs of ALS patients. Interventions may include respiratory support with non-invasive ventilation, nutritional support via feeding tubes, physical therapy to maintain mobility, and speech therapy to manage communication difficulties. Palliative care services are also essential to provide comfort and support as the disease progresses.
Investigational Treatments and Clinical Trials
Research into new treatments for Amyotrophic Lateral Sclerosis (ALS) is ongoing, with numerous clinical trials investigating potential therapies. These include gene therapy, stem cell therapy, and novel pharmacological agents targeting various disease mechanisms. Participation in clinical trials offers patients access to experimental treatments and contributes to the advancement of ALS research. While these investigational treatments hold promise, their efficacy and safety must be rigorously evaluated before they can become standard care options.
Stem Cell Therapy
Role of Stem Cell Therapy in Multiple Sclerosis (MS)
Stem cell therapy is an emerging area of research in Multiple Sclerosis (MS) with the potential to repair damaged myelin and modulate the immune response. Hematopoietic stem cell transplantation (HSCT) involves harvesting a patient’s stem cells, followed by high-dose chemotherapy to suppress the immune system and reintroduce the stem cells to rebuild a healthier immune system. Early studies have shown promising results in reducing disease activity and improving neurological function. Mesenchymal stem cells (MSCs) are also being investigated for their regenerative and immunomodulatory properties. While stem cell therapy for MS is still in the experimental stages, it offers hope for more effective treatments in the future.
Role of Stem Cell Therapy in Amyotrophic Lateral Sclerosis (ALS)
Stem cell therapy is also being explored as a potential treatment for Amyotrophic Lateral Sclerosis (ALS). The goal of stem cell therapy in ALS is to replace damaged motor neurons, protect existing neurons, and modulate the disease environment. Various types of stem cells, including mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), are being studied for their potential to slow disease progression and improve motor function. Clinical trials are ongoing to assess the safety and efficacy of stem cell therapy in ALS patients. While early results are promising, more research is needed to determine the long-term benefits and risks of this innovative approach.
Prognosis
Prognostic Factors in Multiple Sclerosis (MS)
The prognosis for Multiple Sclerosis (MS) varies widely among individuals and is influenced by several factors. Early diagnosis and treatment with disease-modifying therapies (DMTs) can significantly improve long-term outcomes. Patients with relapsing-remitting MS (RRMS) generally have a better prognosis than those with primary progressive MS (PPMS). Other favorable prognostic factors include being female, younger age at onset, and fewer initial neurological deficits. Conversely, a high frequency of relapses, early disability, and extensive MRI lesions are associated with a worse prognosis. Ongoing monitoring and individualized treatment plans are essential for optimizing outcomes in MS patients.
Prognostic Factors in Amyotrophic Lateral Sclerosis (ALS)
The prognosis for Amyotrophic Lateral Sclerosis (ALS) is generally poor, with most patients experiencing rapid disease progression and a reduced life expectancy. Several factors can influence the rate of disease progression and overall survival. Younger age at onset, a slower rate of symptom progression, and a higher level of physical function at diagnosis are associated with a better prognosis. Genetic factors, such as specific mutations, can also impact the disease course. Early intervention with supportive therapies, respiratory care, and participation in clinical trials may help improve quality of life and extend survival for ALS patients.
Quality of Life Considerations
Managing Daily Life with Multiple Sclerosis (MS)
Managing daily life with Multiple Sclerosis (MS) involves addressing the physical, emotional, and cognitive challenges associated with the disease. Patients may benefit from physical and occupational therapy to maintain mobility and independence. Assistive devices, such as canes, walkers, or wheelchairs, can help with mobility. Cognitive rehabilitation and psychological support are crucial for managing cognitive symptoms and emotional well-being. Lifestyle modifications, such as regular exercise, a balanced diet, and stress management techniques, can also improve overall health and quality of life. Support groups and patient education programs provide valuable resources and social support for individuals living with MS.
Managing Daily Life with Amyotrophic Lateral Sclerosis (ALS)
Managing daily life with Amyotrophic Lateral Sclerosis (ALS) requires a comprehensive and multidisciplinary approach to address the progressive physical and emotional challenges of the disease. Assistive technologies, such as speech-generating devices, power wheelchairs, and adaptive equipment, can enhance communication and mobility. Respiratory support, including non-invasive ventilation, is critical as respiratory muscles weaken. Nutritional support, often through feeding tubes, ensures adequate caloric intake. Psychological support and palliative care services are essential for maintaining quality of life and providing comfort. Engaging in social activities and support groups can help ALS patients and their families cope with the emotional impact of the disease.
FAQs
1. What are the primary differences between Multiple Sclerosis (MS) and Amyotrophic Lateral Sclerosis (ALS)?
Multiple Sclerosis (MS) is an autoimmune disease affecting the central nervous system, characterized by relapsing-remitting or progressive symptoms. Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder that primarily affects motor neurons, leading to muscle weakness and atrophy. While MS involves immune-mediated damage to the myelin sheath, ALS involves the degeneration of motor neurons.
2. Can stem cell therapy cure MS or ALS?
Currently, stem cell therapy is not a cure for MS or ALS. However, it is an emerging area of research with potential to repair damaged tissues and modulate the disease process. Clinical trials are ongoing to evaluate the safety and efficacy of stem cell treatments for these conditions.
3. How can early diagnosis impact the prognosis of MS and ALS?
Early diagnosis of MS allows for timely initiation of disease-modifying therapies (DMTs), which can slow disease progression and improve long-term outcomes. In ALS, early diagnosis enables patients to access supportive care and symptom management strategies, potentially improving quality of life and extending survival.
4. What lifestyle modifications can help manage MS symptoms?
Lifestyle modifications for managing MS symptoms include regular exercise, a balanced diet, stress management techniques, and maintaining a healthy weight. Physical and occupational therapy, cognitive rehabilitation, and psychological support are also important for optimizing overall health and quality of life.
For more information or to learn more about managing MS and ALS, please visit us online.