Multiple sclerosis (MS) is a chronic, autoimmune disease that affects the central nervous system (CNS), including the brain, spinal cord, and optic nerves. It is characterized by inflammation, demyelination (loss of the protective myelin sheath around nerves), and subsequent axonal damage, which leads to a variety of neurological symptoms. The exact cause of MS is unknown, but it is believed to result from a complex interaction of genetic, environmental, and immunological factors. Understanding MS begins with comprehending its pathological processes and their impact on the CNS.
Importance of Early Prognosis in Multiple Sclerosis
Early prognosis in MS is crucial for several reasons. Early identification and intervention can significantly alter the disease course, potentially delaying or preventing significant disability. Early prognosis allows for timely initiation of disease-modifying therapies (DMTs), which can reduce the frequency and severity of relapses, slow disease progression, and improve long-term outcomes. Moreover, understanding the likely progression helps in planning and managing life with MS, including addressing physical, emotional, and social aspects, thereby enhancing the overall quality of life for patients.
Overview of Multiple Sclerosis Pathophysiology
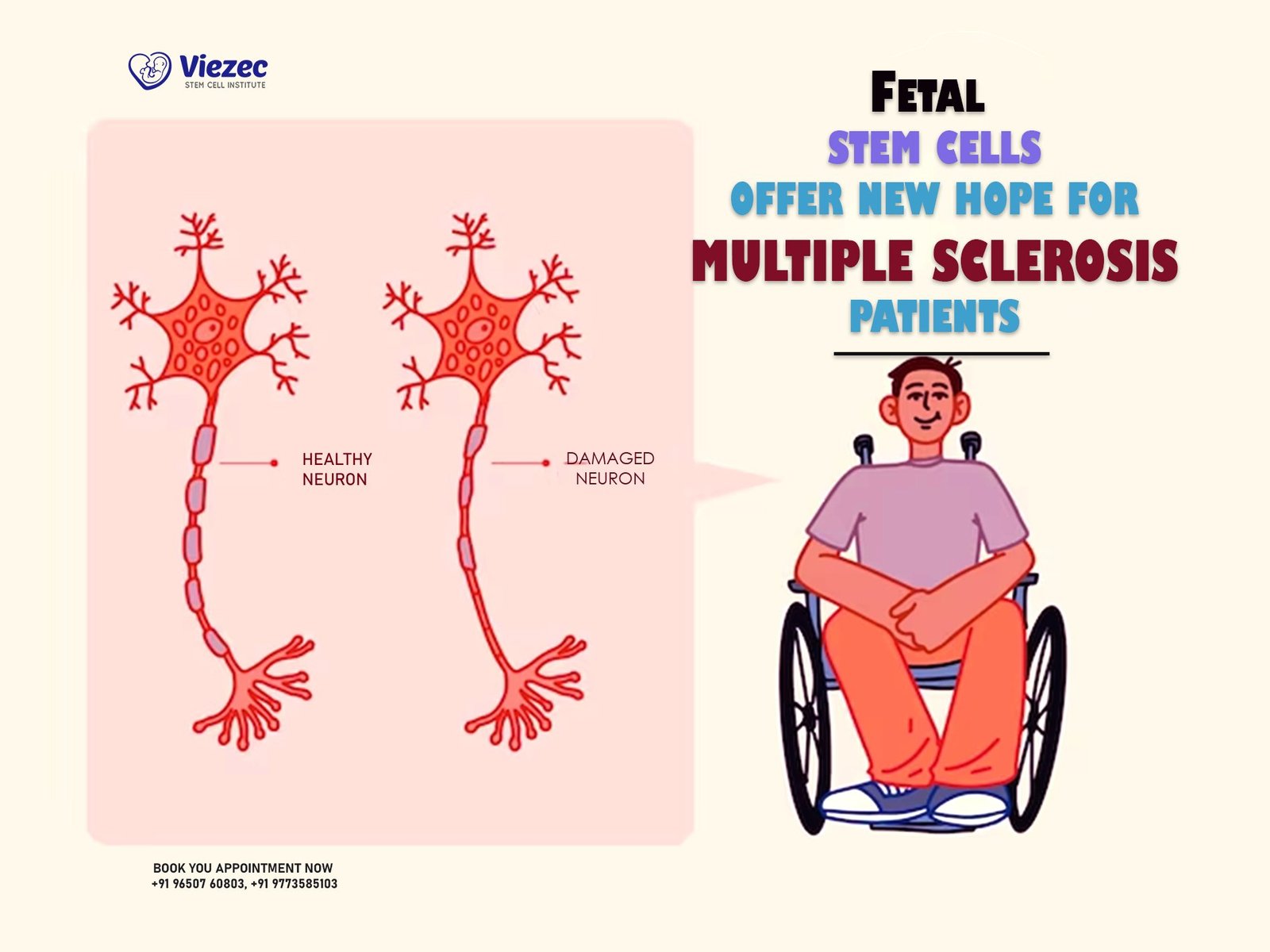
The pathophysiology of MS involves immune system dysregulation, where the body’s immune cells mistakenly attack myelin, the protective covering of nerve fibers. This leads to inflammation and the formation of scar tissue or plaques, disrupting normal nerve transmission. Over time, repeated attacks can cause permanent damage to the underlying nerve fibers (axons), contributing to a decline in neurological function. The severity and patterns of demyelination and axonal loss vary among individuals, contributing to the diverse clinical presentations of MS.
Epidemiology of Multiple Sclerosis
Global Prevalence of Multiple Sclerosis
MS affects millions of people worldwide, with a prevalence that varies significantly by region. It is more common in temperate climates and less common near the equator, suggesting environmental factors such as sunlight exposure and vitamin D levels may play a role. In North America and Europe, the prevalence is estimated to be around 100-200 cases per 100,000 people, while in Asia and Africa, the rates are considerably lower. Understanding the epidemiological patterns of MS helps in identifying potential risk factors and planning public health strategies.
Demographic Variations in Multiple Sclerosis
MS is more prevalent in women than men, with a female-to-male ratio of approximately 2-3:1. The disease typically presents between the ages of 20 and 40, although it can occur at any age. Genetic predisposition also plays a significant role, with higher incidence rates observed in individuals of Northern European descent. Familial aggregation of MS suggests that genetic factors, possibly in combination with shared environmental exposures, contribute to the risk of developing the disease.
Risk Factors Influencing Early Prognosis of Multiple Sclerosis
Several risk factors can influence the early prognosis of MS. These include genetic factors such as specific HLA gene variants, environmental factors like low vitamin D levels and smoking, and infectious agents such as Epstein-Barr virus. Gender also influences disease progression, with males often experiencing a more aggressive course. Understanding these risk factors is vital for identifying individuals at high risk and implementing early intervention strategies.
Clinical Manifestations of Multiple Sclerosis
Common Symptoms Impacting Early Prognosis
The clinical manifestations of MS are highly variable, reflecting the diverse areas of the CNS that can be affected. Common early symptoms include fatigue, visual disturbances (such as optic neuritis), sensory impairments (like numbness or tingling), and motor dysfunction (such as weakness or spasticity). These symptoms can significantly impact daily functioning and quality of life. Identifying and managing these symptoms early can help mitigate their impact and improve long-term outcomes.
Atypical Presentations of Multiple Sclerosis
While there are common symptoms, MS can also present atypically, making diagnosis challenging. Atypical presentations may include isolated cognitive impairment, psychiatric symptoms, or paroxysmal attacks (sudden, brief episodes of neurological dysfunction). These atypical symptoms can lead to misdiagnosis or delays in diagnosis, underscoring the importance of a comprehensive clinical evaluation and high index of suspicion in patients with unexplained neurological symptoms.
Progression Patterns in Multiple Sclerosis
MS progression patterns vary, with the most common being relapsing-remitting MS (RRMS), characterized by periods of symptom exacerbation followed by remission. Over time, many patients with RRMS may transition to secondary progressive MS (SPMS), marked by a steady worsening of symptoms with fewer or no relapses. Primary progressive MS (PPMS), which involves a gradual decline in function from the onset, is less common but associated with a poorer prognosis. Understanding these patterns is crucial for predicting disease course and tailoring treatment strategies.
Diagnostic Criteria for Multiple Sclerosis
McDonald Criteria in Multiple Sclerosis
The McDonald criteria, established by an international panel, are the standard for diagnosing MS. These criteria incorporate clinical findings, MRI evidence, and, when necessary, cerebrospinal fluid (CSF) analysis. The criteria emphasize the demonstration of dissemination of lesions in both time and space—meaning multiple episodes of neurological symptoms and multiple affected areas of the CNS. Accurate and early diagnosis using these criteria is essential for initiating appropriate treatment and improving prognosis.
Role of MRI in Early Prognosis of Multiple Sclerosis
MRI is a critical tool in the diagnosis and monitoring of MS. It allows for the visualization of demyelinating lesions in the brain and spinal cord, providing evidence of disease activity. MRI can detect both new and old lesions, aiding in the assessment of disease progression. Advanced MRI techniques, such as high-resolution imaging and contrast enhancement, further improve diagnostic accuracy and help in the early identification of disease activity, which is crucial for prognosis and treatment planning.
Differential Diagnoses in Multiple Sclerosis
Given the variability in MS symptoms, it is essential to consider and rule out other conditions that can mimic MS, such as neuromyelitis optica spectrum disorder (NMOSD), acute disseminated encephalomyelitis (ADEM), and systemic autoimmune diseases like lupus. A thorough clinical evaluation, detailed patient history, and appropriate use of diagnostic tools, including MRI and laboratory tests, are necessary to differentiate MS from these conditions and ensure accurate diagnosis and treatment.
Biomarkers for Early Prognosis of Multiple Sclerosis
Blood Biomarkers in Multiple Sclerosis
Identifying reliable blood biomarkers for MS is an area of active research. Biomarkers such as neurofilament light chain (NfL), which reflects neuronal damage, and glial fibrillary acidic protein (GFAP), indicating astrocytic injury, are showing promise in predicting disease activity and progression. These biomarkers could potentially be used to monitor treatment response and adjust therapies accordingly, improving patient outcomes by allowing for more personalized and timely interventions.
Cerebrospinal Fluid Analysis for Early Prognosis
CSF analysis is a valuable tool in MS diagnosis, often used to identify the presence of oligoclonal bands (OCBs), which indicate an abnormal immune response within the CNS. Elevated levels of NfL in CSF are also associated with neuronal damage and can provide insights into disease activity and prognosis. Regular CSF analysis in conjunction with other diagnostic methods can enhance early prognosis and guide treatment decisions, helping to manage the disease more effectively.
Genetic Markers in Multiple Sclerosis Prognosis
Genetic factors play a significant role in MS susceptibility and progression. Variants in the HLA-DRB1 gene are strongly associated with increased risk, and ongoing research aims to identify other genetic markers that influence disease course. Understanding these genetic factors can help in predicting prognosis and tailoring individualized treatment plans. Genetic testing, combined with other prognostic tools, holds promise for more accurate early prognosis and better management of MS.
Neuroimaging in Early Prognosis of Multiple Sclerosis
Advanced MRI Techniques for Multiple Sclerosis
Advanced MRI techniques, such as diffusion tensor imaging (DTI) and magnetization transfer imaging (MTI), provide detailed insights into the microstructural changes in the brain and spinal cord. These techniques can detect subtle changes in myelin integrity and axonal damage that are not visible on conventional MRI. By offering a more precise assessment of disease burden and progression, these advanced imaging modalities can improve early prognosis and inform treatment strategies.
PET and CT Scans in Multiple Sclerosis Prognosis
Positron emission tomography (PET) and computed tomography (CT) scans, while less commonly used than MRI, can provide additional information about metabolic activity and inflammation in the CNS. PET imaging, for example, can detect areas of active inflammation by using tracers that bind to inflammatory cells. These imaging techniques can complement MRI findings and contribute to a more comprehensive understanding of disease activity, aiding in early prognosis and personalized treatment planning.
Emerging Imaging Modalities for Early Prognosis
Emerging imaging modalities, such as optical coherence tomography (OCT) and ultrahigh-field MRI, offer new avenues for assessing MS. OCT measures retinal nerve fiber layer thickness, providing insights into neurodegeneration, while ultrahigh-field MRI offers unprecedented resolution for detecting small lesions and subtle changes in the CNS. These innovative techniques hold promise for enhancing early diagnosis and prognosis, enabling more effective monitoring and management of MS.
Immunological Aspects of Multiple Sclerosis
Immune System Dysregulation in Multiple Sclerosis
MS is fundamentally an immune-mediated disease, where the immune system erroneously targets myelin and other CNS components. This dysregulation involves multiple immune cells, including T cells, B cells, and macrophages, which coordinate the inflammatory response leading to demyelination. Understanding the mechanisms of immune system dysregulation is crucial for developing targeted therapies that can modulate the immune response and potentially halt or slow disease progression.
Autoantibodies and Early Prognosis
The presence of autoantibodies, such as those targeting myelin oligodendrocyte glycoprotein (MOG) or aquaporin-4 (AQP4), can influence the diagnosis and prognosis of MS and related disorders. These autoantibodies help differentiate MS from other demyelinating diseases and can provide insights into disease mechanisms and potential therapeutic targets. Monitoring autoantibody levels may also help predict disease activity and response to treatment, aiding in early prognosis and personalized management.
Role of T and B Cells in Multiple Sclerosis
T cells and B cells play pivotal roles in the pathogenesis of MS. T cells are involved in initiating and sustaining the inflammatory response, while B cells contribute through antibody production and cytokine secretion. Therapies targeting these cells, such as anti-CD20 monoclonal antibodies (e.g., rituximab, ocrelizumab), have shown efficacy in reducing disease activity. Understanding the specific contributions of T and B cells to MS pathophysiology is essential for developing and optimizing these targeted treatments.
Environmental and Lifestyle Factors in Multiple Sclerosis Prognosis
Impact of Vitamin D on Multiple Sclerosis
Vitamin D deficiency has been associated with an increased risk of developing MS and may influence disease progression. Vitamin D modulates the immune system and has anti-inflammatory properties, suggesting that adequate levels could have a protective effect. Studies indicate that vitamin D supplementation may reduce relapse rates and slow disease progression in MS patients. Monitoring and managing vitamin D levels could thus play a crucial role in early prognosis and overall disease management.
Smoking and its Effects on Early Prognosis
Smoking is a well-established risk factor for MS and is associated with a more aggressive disease course. It increases the risk of developing MS and can exacerbate disease activity and progression. The harmful effects of smoking on the immune system and CNS are believed to contribute to these adverse outcomes. Encouraging smoking cessation is therefore an important component of MS management, potentially improving prognosis and reducing the burden of disease.
Dietary Influences in Multiple Sclerosis
Dietary factors may also impact MS prognosis. Diets high in saturated fats and low in fruits and vegetables have been linked to increased inflammation and oxidative stress, which can exacerbate MS symptoms. Conversely, diets rich in omega-3 fatty acids, antioxidants, and other anti-inflammatory nutrients may have protective effects. While more research is needed, adopting a balanced, nutrient-rich diet could support overall health and potentially improve disease outcomes in MS patients.
Current and Emerging Therapies in Multiple Sclerosis
Disease-Modifying Therapies for Multiple Sclerosis
Disease-modifying therapies (DMTs) are the cornerstone of MS treatment, aimed at reducing the frequency and severity of relapses and slowing disease progression. DMTs include interferons, glatiramer acetate, and newer agents like fingolimod, natalizumab, and ocrelizumab. These therapies work by modulating the immune response to prevent further CNS damage. Early initiation of DMTs, guided by a thorough understanding of disease activity, can significantly improve long-term prognosis and quality of life for MS patients.
Symptomatic Treatments in Early Prognosis
In addition to DMTs, symptomatic treatments play a crucial role in managing MS. These treatments address specific symptoms such as spasticity, pain, fatigue, and bladder dysfunction, improving daily functioning and quality of life. Medications, physical therapy, occupational therapy, and lifestyle modifications are all integral to symptomatic management. Early and proactive symptom management can prevent complications, enhance prognosis, and support overall well-being.
Future Therapeutic Directions for Multiple Sclerosis
Research into MS is ongoing, with several promising therapeutic directions on the horizon. These include novel DMTs targeting different aspects of the immune response, neuroprotective agents aimed at preserving neuronal function, and remyelination therapies to repair damaged myelin. Advances in personalized medicine, driven by a deeper understanding of genetic and biomarker profiles, are also expected to enhance treatment precision and efficacy. These future therapies hold the potential to transform MS management and improve early prognosis significantly.
Stem Cell Therapy in Multiple Sclerosis
Basics of Stem Cell Therapy in Multiple Sclerosis
Stem cell therapy involves using stem cells to repair or replace damaged tissues, offering a novel approach to treating MS. Hematopoietic stem cell transplantation (HSCT) is one such therapy, where the patient’s immune system is reset through high-dose chemotherapy followed by the infusion of stem cells. This approach aims to halt disease progression and promote regeneration. While still experimental, stem cell therapy holds promise for providing long-term benefits and improving prognosis in MS.
Current Research on Stem Cell Therapy for Early Prognosis
Ongoing research is exploring the efficacy and safety of various stem cell therapies for MS. Studies have shown that HSCT can lead to prolonged remission in some patients, particularly those with aggressive forms of the disease. Research is also investigating the use of mesenchymal stem cells (MSCs), which have anti-inflammatory and neuroprotective properties, as a potential treatment for MS. These studies aim to refine treatment protocols, identify optimal patient candidates, and establish long-term safety and efficacy.
Clinical Trials of Stem Cell Therapy in Multiple Sclerosis
Numerous clinical trials are evaluating the potential of stem cell therapy in MS. These trials are essential for determining the effectiveness, safety, and practical application of these therapies in clinical practice. Early results from trials of HSCT and MSCs are promising, showing potential for significant disease modification and improvement in patients’ quality of life. Continued research and clinical trials will be crucial in bringing these innovative therapies to the forefront of MS treatment and improving early prognosis.
Rehabilitation and Lifestyle Modifications for Multiple Sclerosis
Physical Therapy and Early Prognosis
Physical therapy is a critical component of MS management, aimed at maintaining and improving physical function, mobility, and overall well-being. Tailored exercise programs can help manage symptoms such as spasticity, weakness, and balance issues, preventing secondary complications and enhancing quality of life. Early intervention with physical therapy can mitigate the impact of MS on daily activities and contribute to a more favorable prognosis.
Cognitive Rehabilitation in Multiple Sclerosis
Cognitive impairment is a common symptom of MS, affecting memory, attention, and executive function. Cognitive rehabilitation involves targeted therapies to improve cognitive function, compensate for deficits, and enhance patients’ ability to manage daily tasks. Techniques such as cognitive training, compensatory strategies, and assistive technologies can significantly improve cognitive outcomes. Early and ongoing cognitive rehabilitation can help maintain cognitive function and support overall quality of life.
Role of Exercise and Diet in Multiple Sclerosis
Exercise and diet are integral to managing MS and improving prognosis. Regular physical activity can enhance muscle strength, cardiovascular health, and mental well-being, while also reducing fatigue and depression. A balanced diet rich in anti-inflammatory foods can support overall health and potentially modulate disease activity. Integrating exercise and dietary modifications into a comprehensive MS management plan can provide significant benefits and improve long-term outcomes.
Psychosocial Aspects and Support Systems in Multiple Sclerosis
Psychological Impact of Multiple Sclerosis on Patients
Living with MS can take a significant psychological toll, leading to anxiety, depression, and social isolation. The uncertainty of disease progression and the impact on daily life can be overwhelming. Psychological support, including counseling, psychotherapy, and support groups, is essential for addressing these challenges. Early and ongoing psychological care can help patients cope with the emotional aspects of MS, enhancing overall well-being and quality of life.
Support Systems and Resources for Early Prognosis
Support systems, including family, friends, healthcare providers, and patient advocacy groups, play a crucial role in managing MS. These resources provide emotional support, practical assistance, and information about the disease and treatment options. Engaging with support systems early in the disease course can help patients navigate the challenges of MS, access necessary resources, and improve their prognosis and quality of life.
Strategies for Enhancing Quality of Life in Multiple Sclerosis
Enhancing quality of life for MS patients involves a holistic approach that addresses physical, emotional, and social needs. Strategies include personalized treatment plans, regular physical and cognitive therapy, psychological support, and lifestyle modifications. Encouraging active engagement in social and recreational activities, providing education about the disease, and promoting self-management skills are also vital. By addressing all aspects of the disease, these strategies can help patients live fulfilling lives despite the challenges of MS.
In conclusion, understanding the early prognosis of multiple sclerosis is a multifaceted endeavor that involves recognizing the disease’s complex pathophysiology, identifying risk factors, and employing a comprehensive approach to diagnosis and management. Early intervention with disease-modifying therapies, symptomatic treatments, and supportive care can significantly improve outcomes for MS patients. Ongoing research and emerging therapies hold promise for even better prognosis and quality of life in the future.