Surgery, whether minor or major, is often accompanied by a long recovery period. Patients are constantly searching for ways to accelerate healing, minimize pain, and return to normal activities faster. One of the most promising advancements in regenerative medicine is stem cell therapy, which has been gaining attention for its potential to reduce recovery time after surgery.
In this article, we’ll explore what stem cell treatment is, how it works in the context of surgical recovery, its benefits, risks, and what current research suggests about its effectiveness.
What is Stem Cell Therapy?
Stem cells are unique cells with the ability to develop into different types of specialized cells in the body. They are also capable of self-renewal, which means they can multiply to repair damaged tissues.
Stem cell therapy involves injecting or transplanting stem cells into injured or damaged areas to promote healing. In surgical recovery, these cells can potentially accelerate tissue repair, reduce inflammation, and improve overall outcomes.
Common Types of Stem Cells Used in Recovery:
-
Mesenchymal Stem Cells (MSCs) – often derived from bone marrow or fat, commonly used for musculoskeletal injuries.
-
Hematopoietic Stem Cells (HSCs) – primarily used for blood disorders, but emerging applications in recovery exist.
-
Induced Pluripotent Stem Cells (iPSCs) – lab-engineered cells that can become any tissue type.
How Stem Cell Therapy May Reduce Recovery Time After Surgery?
The primary goal of stem cell therapy in post-surgical care is to enhance the body’s natural healing process. Here’s how it works:
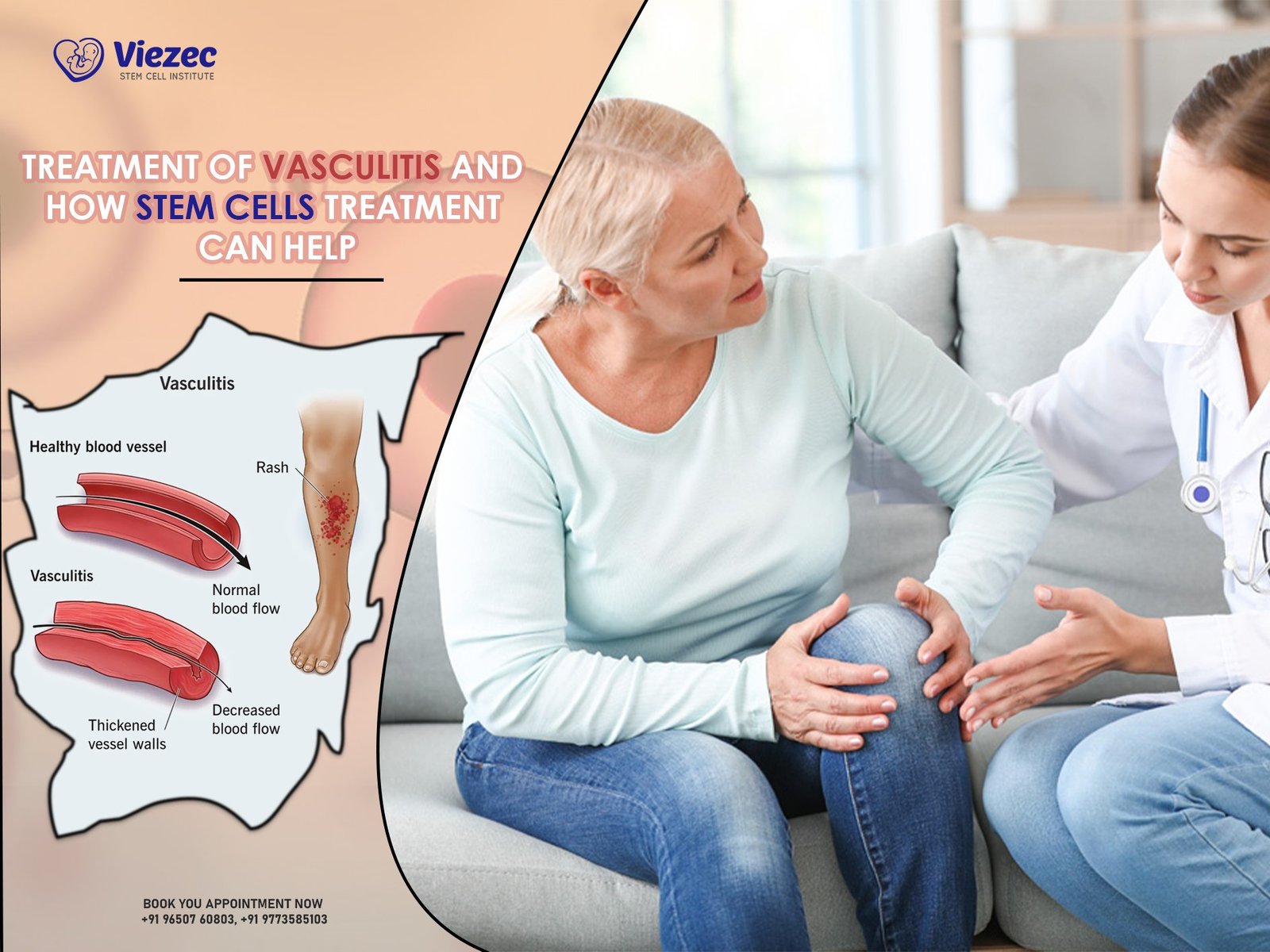
1. Reducing Inflammation
After surgery, inflammation is a natural response that helps repair tissue but can also cause pain, swelling, and slower healing. Stem cells release anti-inflammatory molecules that modulate the immune response, which can lead to faster recovery and less post-operative pain.
2. Promoting Tissue Regeneration
Stem cells can differentiate into muscle, cartilage, or bone cells, depending on the area of injury. This ability allows them to directly contribute to repairing tissues damaged during surgery.
3. Enhancing Angiogenesis (Blood Vessel Formation)
Adequate blood supply is critical for healing. Stem cells release growth factors that promote the formation of new blood vessels, improving oxygen and nutrient delivery to surgical sites.
4. Reducing Scar Tissue Formation
Scar tissue can limit mobility and prolong recovery. Stem cell therapy may help minimize excessive scar formation by encouraging more natural tissue regeneration.
Evidence Supporting Stem Cell Use in Post-Surgical Recovery
Several studies suggest stem cells can shorten recovery time, although outcomes may vary depending on the type of surgery and patient condition.
Musculoskeletal Surgery
Joint replacement. Research on mesenchymal stromal/stem cells (MSCs) — particularly intra-articular or adjunctive MSC applications around knee and hip procedures — shows reductions in inflammation and improvements in pain and function in several clinical trials and reviews. These studies support the potential for faster functional recovery when MSCs are used as an adjunct to standard care.
(Key read: Lamo-Espinosa et al., a Phase II randomized trial and several MSC clinical-trial reviews.)
Tendon repair
Clinical studies and systematic reviews report that MSCs (autologous or allogeneic, bone-marrow or adipose-derived) can promote tendon healing, reduce re-tear rates or stiffness, and improve functional scores in rotator cuff and other tendon repairs. There are randomized controlled trials showing benefit for partial supraspinatus tears and multiple clinical trials testing MSC augmentation for rotator cuff repair.
(Key read: a 2023 rotator-cuff stem-cell review and a randomized study of MSC injection for supraspinatus tears.)
Orthopedic Trauma
Patients with fractures or ligament injuries may benefit from stem cell–based approaches such as bone-marrow aspirate concentrate (BMAC) or progenitor-cell injections. Classic clinical work (Hernigou et al.) and subsequent reviews report improved union rates and faster radiographic/healing times for delayed union and non-union when autologous bone-marrow grafts or BMAC are used. Systematic reviews summarize this evidence while noting heterogeneity in methods and patient selection.
(Key read: Hernigou 2005 on percutaneous autologous bone-marrow grafting for nonunions; multiple reviews on BMAC in fracture healing.)
Cardiovascular and Organ Surgery
Heart / cardiac surgery
Cardiac cell therapy trials and reviews show safety and some signals of functional or quality-of-life improvement, but efficacy results (e.g., consistent improvement in left ventricular ejection fraction) have been mixed and are still evolving. Newer approaches (cell patches, extracellular vesicles) are promising in preclinical and early clinical work.
Liver regeneration
Multiple clinical studies and systematic reviews report that MSC infusion or transplantation can improve biochemical markers and clinical scores in patients with acute or chronic liver failure and liver fibrosis. These applications are promising but heterogeneous in protocols and are still moving through clinical validation.
Advantages of Using Stem Cell Therapy During Surgical Recovery
Stem cell–supported recovery introduces several meaningful improvements that go beyond traditional healing methods. When stem cells are applied after surgery, patients often experience a more efficient and balanced healing process.
Accelerated Healing Response
Stem cells promote quicker restoration of damaged tissues by stimulating cellular growth and repair pathways, allowing patients to regain strength sooner. This enhanced regeneration contributes to a smoother, more predictable recovery timeline that supports better overall healing quality.
Less Pain and Inflammation
Anti-inflammatory properties of stem cells help decrease discomfort. Their ability to modulate inflammation helps minimize post-operative pain, swelling, and stiffness, leading to a more comfortable recovery experience. This reduction in inflammation also allows rehabilitation exercises to begin earlier, which further supports faster progress and mobility.
Better Functional Outcomes
Stem cells support structural repair and functional restoration across different tissues, helping patients regain movement, flexibility, and strength after surgery. This improvement in physical performance leads to better long-term outcomes and decreases the chances of chronic discomfort or limited mobility.
Minimized Scar Tissue Formation
Promotes natural tissue regrowth rather than fibrotic tissue. By guiding the healing process toward healthy tissue regeneration instead of thick scar formation, stem cells help maintain elasticity and natural function. This is especially beneficial in surgeries involving joints, tendons, or skin where excessive scarring may restrict movement or create cosmetic concerns.
Lower Chances of Post-Surgical Complications
Potentially decreases the likelihood of infections and other post-operative complications. Stem cells support immune regulation and improve the body’s ability to respond to early healing challenges, helping reduce risks such as infection, delayed repair, or tissue breakdown. Their regenerative activity creates a more stable healing environment, contributing to safer recovery outcomes.
Types of Surgeries That May Benefit From Stem Cell Therapy
Stem cell therapy can support recovery across various surgical procedures, particularly those that involve tissue damage, inflammation, or structural repair. By enhancing natural healing pathways, stem cells may improve outcomes and support faster post-operative recovery.
Orthopedic Surgeries
Stem cell applications are widely explored in orthopedic surgeries because these procedures often involve significant tissue trauma and lengthy healing periods. Incorporating regenerative cells may help improve mobility, reduce inflammation, and strengthen damaged bone, cartilage, and ligaments after surgery.
Examples include:
-
Knee, hip, or shoulder replacement
-
ACL or rotator cuff repair
-
Fracture repair
-
Cartilage regeneration procedures
Cosmetic and Reconstructive Surgeries
Regenerative therapies may enhance cosmetic and reconstructive outcomes by promoting healthier tissue formation and reducing scarring. Stem cells can support skin repair, improve blood flow, and help regenerate soft tissue, making them a useful addition in aesthetic or restorative surgical treatments.
Examples include:
-
Facial reconstruction
-
Burn treatment and skin grafts
-
Scar revision surgery
Organ-Related Surgeries (Experimental)
For complex organ-related procedures, stem cell therapy is still emerging but shows encouraging potential in early studies. Researchers are exploring how regenerative cells may restore damaged organ tissue, improve functional recovery, and support long-term healing after major surgical interventions.
Examples include:
-
Heart bypass and repair
-
Liver surgery or transplantation
-
Kidney and lung tissue regeneration
How Stem Cell Therapy is Administered Post-Surgery?
Stem cells can be delivered in multiple ways depending on the surgical area and goal:
-
Local Injection – Directly into the surgical site or surrounding tissue.
-
Intravenous (IV) Infusion – For systemic effects, commonly used in organ repair or trauma cases.
-
Tissue-Seeded Scaffolds – Stem cells are combined with biodegradable scaffolds to enhance tissue growth.
Most post-surgical therapies are performed within days to weeks after surgery to maximize tissue regeneration during the critical healing phase.
What Patients Can Expect During Recovery With Stem Cell Therapy?
Every patient’s healing journey is unique, but many individuals notice meaningful improvements when stem cell therapy is part of their post-surgical recovery plan.
Reduced Pain and Swelling –
Many patients experience noticeably less discomfort and inflammation after surgery, allowing them to move more comfortably and begin rehabilitation activities earlier in the healing process.
Improved Mobility –
Stem cell support often helps patients regain movement, strength, and flexibility sooner, contributing to a smoother transition back to daily routines and physical activities.
Shorter Hospital Stay –
Because healing may progress more efficiently, some individuals are discharged earlier than expected, reducing overall hospital time and helping them recover in a more comfortable environment.
Better Long-Term Outcomes –
Enhanced tissue quality and stronger repair may lower the chances of complications or secondary injuries, decreasing the likelihood of needing revision procedures in the future.
Combining Stem Cell Therapy with Traditional Rehabilitation
Stem cell therapy is not a standalone solution. Its benefits are maximized when combined with traditional post-surgical rehabilitation:
-
Physical Therapy – Helps restore strength, flexibility, and range of motion.
-
Nutritional Support – Adequate protein, vitamins, and minerals aid tissue regeneration.
-
Pain Management – Anti-inflammatory medications may be used in conjunction with stem cells.
-
Lifestyle Adjustments – Avoiding smoking and excessive alcohol improves stem cell effectiveness.
FAQs
When administered by a certified physician, stem cell therapy is generally safe, though minor risks like infection or immune reactions exist.
Timing depends on the surgery type, but many protocols apply stem cells within days to a few weeks post-operation.
Most insurance plans currently do not cover stem cell therapy, especially for experimental applications.
Studies suggest recovery may be 20–40% faster for certain orthopedic procedures, though outcomes vary.
Not all patients are candidates. Age, overall health, type of surgery, and existing medical conditions are important factors.
Stem cell therapy may support healing by promoting tissue repair and reducing inflammation. Its effectiveness depends on the type of surgery and the patient’s overall condition.
Stem cells might aid in reducing pain and improving joint function after knee replacement. However, they do not replace the implanted joint, and results vary among patients.
It may help enhance recovery by supporting tendon and muscle healing around the shoulder. The benefits depend on the injury severity and the patient’s response to treatment.
Conclusion
Stem cell therapy represents a revolutionary approach to post-surgical recovery. By reducing inflammation, promoting tissue regeneration, and enhancing overall healing, stem cells may significantly reduce recovery time after surgery.
However, it is not a guaranteed solution. Patients must weigh benefits, risks, costs, and scientific evidence before pursuing therapy. When combined with traditional rehabilitation and a healthy lifestyle, stem cell therapy offers a promising avenue for faster, more effective recovery.
Note – As regenerative medicine continues to advance, stem cell therapy may become a standard part of post-surgical care, offering patients a quicker return to their daily lives and improved long-term outcomes.
List of References:-
Cui, C., Lin, F., Xia, L., & Zhang, X. (2025). Mesenchymal stem cells therapy for the treatment of non-union fractures: a systematic review and meta-analysis. BMC Musculoskeletal Disorders, 26, 245. https://doi.org/10.1186/s12891-025-08365-w
Theodosaki, A. M., Tzemi, M., Galanis, N., Bakopoulou, A., Kotsiomiti, E., Aggelidou, E., & Kritis, A. (2024). Bone regeneration with mesenchymal stem cells in scaffolds: Systematic review of human clinical trials. Stem Cell Reviews and Reports, 20(4), 938–966. https://doi.org/10.1007/s12015-024-10696-5
Gómez-Barrena, E., Padilla-Escabias, P., et al. (2023). (as part of the systematic analyses included in Theodosaki et al.’s 2024 review) — various clinical trials of MSC-based scaffold therapy for bone defects and non-unions. Included in: Bone regeneration with mesenchymal stem cells in scaffolds: Systematic review of human clinical trials. Stem Cell Reviews and Reports, 20(4), 938–966. https://doi.org/10.1007/s12015-024-10696-5
Various authors (2022–2025). Human clinical studies of MSC therapy in non-union fractures and bone-defect repair, aggregated in the meta-analysis by Cui et al. (2025). The primary source meta-analysis — see item #1. https://link.springer.com/article/10.1186/s12891-025-08365-w
Studies using MSC + scaffold therapy (alveolar bone defects, clefts, long-bone defects) in human patients — aggregated and discussed in Theodosaki et al. (2024). Stem Cell Reviews and Reports, 20(4), 938–966. https://doi.org/10.1007/s12015-024-10696-5