Osteoarthritis (OA) is a progressive, often debilitating joint condition that affects millions worldwide. Traditional treatments—ranging from pain medications to joint replacement surgery—focus on symptom management rather than healing. But what if there was a way to not just mask the pain, but repair the damage itself?
Enter stem cell therapy—a cutting-edge, regenerative approach that’s generating excitement and cautious optimism in both medical and patient communities. By using the body’s own powerful building blocks—stem cells—this therapy aims to reduce inflammation, regenerate cartilage, and restore joint function.
But is it too good to be true? Or is science finally catching up with the promise?
In this article, we explore the potential of stem cell therapy as a viable treatment for osteoarthritis. We break down the science, review clinical evidence, compare it with conventional treatments, and hear from real patients who’ve taken the leap. Whether you’re newly diagnosed or exploring alternatives to surgery, this guide will help you understand if stem cell therapy could be a real solution or simply a hopeful frontier.
Introduction to Osteoarthritis and Modern Treatments
What Is Osteoarthritis?
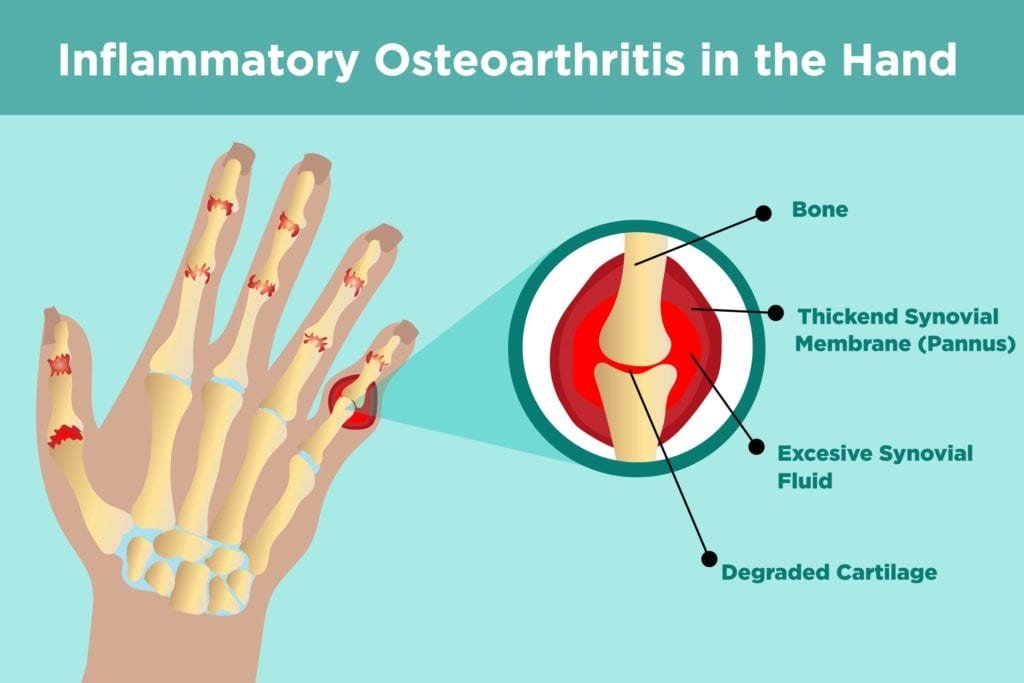
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It’s a chronic, degenerative joint condition where the protective cartilage that cushions the ends of your bones gradually wears down over time. This loss of cartilage leads to joint pain, stiffness, swelling, and reduced flexibility. While OA can impact any joint, it most commonly affects the knees, hips, hands, and spine.
Unlike some autoimmune forms of arthritis, OA is typically caused by aging, repetitive stress on the joints, previous injuries, or genetic predisposition. It’s a progressive condition—meaning it tends to worsen over time—and there’s currently no known cure. However, various treatments aim to manage symptoms and improve quality of life.
Traditional Approaches to Osteoarthritis Management
Conventional treatment strategies for osteoarthritis are centered around symptom relief and slowing joint deterioration. These include:
-
Medications: Over-the-counter pain relievers like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help manage pain and inflammation.
-
Physical therapy: Customized exercises can strengthen the muscles around the joint, improve range of motion, and reduce discomfort.
-
Lifestyle changes: Weight loss, low-impact exercise, and joint-friendly activities like swimming can significantly ease strain on affected joints.
-
Injections: Corticosteroid or hyaluronic acid injections are often used to temporarily relieve pain and inflammation in moderate to severe OA.
-
Surgery: In advanced cases, procedures such as arthroscopy, osteotomy, or total joint replacement may be necessary.
While these treatments can improve symptoms, they don’t reverse joint damage. That’s why many researchers and patients are turning to regenerative medicine—and in particular, stem cell therapy—as a potential game-changer in OA care.
Stem Cell Therapy Explained
What Are Stem Cells?
Stem cells are like the body’s raw materials unique cells with the remarkable ability to develop into many different cell types, from muscle and nerve cells to cartilage-producing cells. Unlike specialized cells, stem cells can replicate themselves and repair damaged tissues, making them a powerful tool in regenerative medicine.
What makes them especially exciting in osteoarthritis treatment is their potential to not just relieve symptoms—but to actually restore joint function by repairing or regenerating damaged cartilage.
Types of Stem Cells Relevant to Osteoarthritis
There are several types of stem cells being explored for use in treating osteoarthritis. Here are the most relevant:
-
Mesenchymal Stem Cells (MSCs): These are adult stem cells most commonly used in OA therapy. They’re found in bone marrow, adipose (fat) tissue, and umbilical cord tissue. MSCs are favored for their ability to differentiate into cartilage cells and their anti-inflammatory properties.
-
Embryonic Stem Cells (ESCs): These pluripotent cells can turn into any type of cell in the body. However, their use is controversial and heavily restricted due to ethical concerns, and they are rarely used in OA therapy.
-
Induced Pluripotent Stem Cells (iPSCs): These are adult cells genetically reprogrammed to act like embryonic stem cells. iPSCs are promising in lab research, but clinical applications for OA are still in early development.
Among these, MSCs are the most widely researched and clinically used for osteoarthritis due to their accessibility, safety profile, and ability to influence healing.
How Stem Cells Regenerate Tissue
So how do stem cells actually help repair joints?
When introduced into an osteoarthritic joint—usually via injection—stem cells respond to the signals from damaged tissue. They begin releasing bioactive molecules, such as growth factors and cytokines, which:
-
Reduce inflammation
-
Encourage tissue repair
-
Attract other healing cells to the area
-
Differentiate into chondrocytes, the specialized cells that produce cartilage
This process not only slows the progression of joint degeneration but may also help restore the structure and function of the joint over time. While results vary, many patients experience improved mobility, reduced pain, and a better quality of life after treatment.
Is Stem Cell Therapy Right for You?
Explore the benefits of stem cell therapy for osteoarthritis and take the first step toward a pain-free life.
How Does Stem Cell Therapy Work for Osteoarthritis?
Mechanism of Action in Joint Repair
When stem cells—particularly mesenchymal stem cells (MSCs)—are injected into a joint affected by osteoarthritis, they do more than just sit there. They respond to the joint’s inflammatory environment by migrating to areas of damage and releasing a cascade of regenerative signals.
These cells don’t necessarily “become” cartilage on their own (although some may differentiate into chondrocytes), but their primary power lies in their paracrine effects—meaning they influence surrounding cells to heal and regenerate. Here’s what they do:
-
Stimulate the growth of new cartilage cells
-
Inhibit enzymes that break down existing cartilage
-
Reduce joint inflammation
-
Improve lubrication and cushioning within the joint
Over time, this activity can lead to less joint pain, improved mobility, and potentially even the rebuilding of cartilage tissue in mild to moderate cases of OA.
Role of Inflammation and Stem Cells
Chronic inflammation is a hallmark of osteoarthritis. As cartilage breaks down, the immune system kicks into high gear, producing pro-inflammatory cytokines that worsen the damage and lead to swelling, stiffness, and discomfort.
This is where MSCs shine: they’re natural inflammation regulators. When introduced into an inflamed joint, MSCs secrete molecules that:
-
Decrease levels of pro-inflammatory cytokines (like TNF-α and IL-1β)
-
Increase production of anti-inflammatory cytokines (like IL-10)
-
Modulate immune cell activity to prevent further joint damage
By creating a more balanced immune response, MSCs calm the storm, setting the stage for healing and cartilage preservation.
MSCs (Mesenchymal Stem Cells) in Joint Health
Think of MSCs as multitaskers in joint health. In addition to reducing inflammation and aiding cartilage repair, they:
-
Support the formation of synovial fluid, which lubricates joints
-
Promote angiogenesis, the formation of new blood vessels, which improves nutrient delivery to joint tissues
-
Inhibit scar tissue formation and fibrosis, which can stiffen joints
Comparing Stem Cell Therapy to Traditional Treatments
Medications vs. Regenerative Therapy
Traditional medications like NSAIDs (nonsteroidal anti-inflammatory drugs), acetaminophen, and corticosteroid injections are widely used to manage osteoarthritis symptoms. They’re effective at reducing pain and inflammation, but they don’t actually repair joint damage—and over time, they can come with unwanted side effects.
-
NSAIDs may irritate the stomach lining, raise blood pressure, and increase the risk of heart problems with long-term use.
-
Corticosteroids, while offering quick relief, can actually accelerate cartilage breakdown if used too frequently.
Stem cell therapy, on the other hand, belongs to a new class of treatments called regenerative medicine. Instead of just masking symptoms, it targets the underlying damage, aiming to stimulate tissue repair and slow the disease process.
The contrast is clear: while medications offer short-term symptom control, stem cell therapy presents a long-term, potentially restorative approach.
Surgery vs. Stem Cells
Joint replacement surgery—particularly for the knees and hips—is often considered the final solution for severe OA. It can dramatically improve mobility and reduce pain, but it also comes with significant risks and recovery time:
-
Up to 3–6 months of rehabilitation
-
Potential complications like blood clots, infection, or implant failure
-
Limited lifespan of prosthetic joints (typically 15–20 years)
Stem cell therapy, in comparison, is minimally invasive, typically performed as an outpatient procedure with little to no downtime. While it might not be suitable for everyone—especially in advanced OA cases—it offers a compelling option for patients who:
-
Want to avoid surgery or delay it
-
Are not good surgical candidates due to age or health conditions
-
Prefer a more natural, biologically-based treatment
Cost-Benefit Comparison
At first glance, stem cell therapy may seem expensive. In the U.S., the cost typically ranges from $3,000 to $10,000 per joint, depending on the provider, stem cell source, and number of treatments needed.
However, when comparing this to:
-
The $30,000–$50,000 cost of a total joint replacement
-
The recovery time, time off work, and long-term medication use often required after surgery
-
The fact that stem cell therapy may delay or prevent the need for surgery altogether
Get Started with Stem Cell Therapy Today!
If you’re ready to take control of your health, contact us now to learn more about our treatments for osteoarthritis.
Risks and Side Effects
Is Stem Cell Therapy Safe?
One of the biggest questions patients have about stem cell therapy is: “Is it safe?” The reassuring news is that, when performed correctly using autologous (your own) stem cells, the procedure is generally considered low risk and well-tolerated.
Reported side effects are usually mild and may include:
-
Temporary joint swelling or discomfort after injection
-
Mild soreness at the site where cells were harvested (e.g., hip or abdomen)
-
Rarely, infection or inflammation at the injection site
To date, no significant long-term adverse effects have been linked to properly administered stem cell therapy using autologous MSCs. However, risks can increase when:
-
The procedure is performed by unqualified providers
-
Unregulated or non-FDA-approved products are used
-
Cells are cultured or altered in ways that aren’t thoroughly tested
Candidacy and Suitability
Who Can Benefit Most from Stem Cell Therapy?
Stem cell therapy for osteoarthritis isn’t a one-size-fits-all solution. However, it holds the most promise for individuals in the early to moderate stages of OA, where there’s still some cartilage left to work with and the joint structure remains relatively intact.
Ideal candidates typically include:
-
Adults with mild to moderate OA who haven’t found lasting relief from medications, physical therapy, or other conservative treatments
-
People looking to delay or avoid joint replacement surgery
-
Patients who prefer a less invasive, biologically-driven approach
-
Those with localized joint pain rather than widespread arthritis
Athletes and active individuals often turn to stem cell therapy to preserve joint health and extend their physical careers. However, everyday patients—those just wanting to walk without pain or enjoy life without constant discomfort—are seeing positive outcomes too.
Age, Severity, and Other Considerations
While stem cell therapy is considered safe across a wide age range, results can vary based on individual health and joint condition. Here are a few important factors:
-
Age: Younger patients (under 60) often respond better due to higher baseline cell quality and less advanced joint damage.
-
Severity of OA: Stem cell therapy is less effective in severe or end-stage OA, where cartilage has been almost completely worn away and the joint space is significantly narrowed.
-
Overall health: Chronic conditions like uncontrolled diabetes or autoimmune disorders may affect healing potential.
-
Lifestyle: Non-smokers, active individuals, and those committed to rehabilitation tend to experience more favorable outcomes.
That said, even patients in their 70s have seen meaningful improvements—especially when they maintain a healthy weight, stay mobile, and follow their provider’s aftercare instructions.
Ultimately, a thorough medical evaluation, including imaging and joint assessments, is necessary to determine if stem cell therapy is a viable and realistic option for a given patient.
Cost and Accessibility
Average Cost of Treatment
Stem cell therapy isn’t cheap, and one of the most common barriers for patients is the out-of-pocket expense. In the U.S., treatment costs typically range from $3,000 to $10,000 per joint, depending on several factors:
-
Source of stem cells: Bone marrow or fat-derived cells (autologous) may cost less than cultured or lab-expanded allogeneic options.
-
Number of injections: Some patients receive a single treatment, while others may require multiple sessions for optimal results.
-
Clinic location and expertise: Costs can vary widely depending on geographic region and the reputation of the clinic or provider.
-
Additional services: Some providers include PRP (platelet-rich plasma), physical therapy, or advanced imaging in the package.
It’s worth noting that while this upfront cost may seem high, many patients compare it favorably to the long-term costs of medications, physical therapy, and potential surgery, not to mention lost productivity or reduced quality of life.
Experience the Power of Stem Cell Therapy
Join the growing number of patients benefiting from regenerative treatments for osteoarthritis.
Stem Cell Treatment for Osteoarthritis in India
Growing Demand and Accessibility in India
India has rapidly emerged as a global hub for regenerative medicine, offering advanced stem cell therapies at more accessible prices compared to many Western countries. The country’s combination of skilled medical professionals, state-of-the-art facilities, and cost-effective care makes it an attractive option for both local and international patients seeking alternatives to surgery for osteoarthritis.
With a growing number of clinics and research institutions investing in stem cell science, India is at the forefront of offering innovative, evidence-based treatments—especially for chronic joint conditions like osteoarthritis.
Viezec – A Recognized Provider in India
One of the notable providers of stem cell therapy for osteoarthritis in India is Viezec Medical Health Care, based in New Delhi. Viezec has positioned itself as a trusted facilitator of personalized, patient-centered regenerative treatments, collaborating with accredited hospitals and labs.
Key features of Viezec’s stem cell offerings include:
-
Use of mesenchymal stem cells (MSCs) derived from umbilical cord tissue or autologous sources
-
Minimally invasive injection procedures tailored to the patient’s specific joint condition
-
A focus on international patients, offering end-to-end medical travel support
-
Coordination with licensed, experienced specialists and JCI/NABH-accredited hospitals
-
Transparent consultation and follow-up care
Patients often choose Viezec for its blend of affordability, professionalism, and access to quality healthcare infrastructure. While the therapy is still considered investigational, Viezec maintains ethical standards and prioritizes patient safety.
Why Consider India for OA Treatment?
-
Lower costs: Stem cell therapy in India typically costs 30–60% less than in the U.S. or Europe, with similar quality standards.
-
Expertise and innovation: Many Indian clinics collaborate with global research networks and follow emerging protocols.
-
Medical tourism infrastructure: Language support, visa assistance, and comprehensive care packages make India a viable choice for international patients.
As always, patients should do their due diligence—verifying credentials, requesting clinical outcomes data, and discussing potential risks and benefits before committing to treatment.
Read related articles here:-