Muscle injuries are a common occurrence, affecting individuals across various age groups and activity levels. Whether incurred through sports, accidents, or everyday activities, these injuries can significantly impact one’s quality of life and physical function. While traditional treatment methods such as rest, physical therapy, and surgery have been mainstays in managing muscle injuries, the emergence of stem cell therapy offers new hope for improved recovery outcomes.
Background of Muscle Injuries
Muscle injuries encompass a range of conditions, including strains, tears, and contusions, each with its own set of causes and symptoms. These injuries can occur suddenly, as in the case of acute trauma, or develop gradually due to overuse or repetitive stress. Regardless of the cause, prompt and effective treatment is essential to prevent complications and promote optimal healing.
Importance of Effective Treatment Methods
The timely and appropriate management of muscle injuries is crucial for several reasons. Firstly, untreated or poorly managed injuries can lead to chronic pain, reduced mobility, and long-term disability. Moreover, athletes and individuals with physically demanding occupations rely on rapid recovery to return to their respective activities and livelihoods. Therefore, advancements in treatment modalities that expedite healing and restore function are highly sought after.
Overview of Stem Cell Therapy
Stem cell therapy represents a cutting-edge approach to tissue repair and regeneration. By harnessing the regenerative potential of stem cells, researchers aim to accelerate the healing process and improve outcomes for a variety of medical conditions, including muscle injuries. Stem cells possess unique properties that enable them to differentiate into specialized cell types and modulate the immune response, making them ideal candidates for therapeutic intervention.
Understanding Muscle Injuries
Types of Muscle Injuries (Strains, Tears, Contusions)
Muscle injuries can be broadly categorized into strains, tears, and contusions, each involving damage to different structures within the muscle tissue. Strains occur when muscle fibers stretch or tear due to excessive force or overextension. Tears, on the other hand, involve more extensive damage to the muscle fibers, often resulting in significant pain and functional impairment. Contusions refer to bruising or localized bleeding within the muscle tissue, typically caused by direct impact or trauma.
Causes and Risk Factors
Muscle injuries can occur as a result of various factors, including sudden trauma, repetitive motion, inadequate warm-up or stretching, and structural imbalances. Athletes participating in high-impact sports are particularly susceptible to muscle injuries due to the intense physical demands placed on their bodies. Additionally, factors such as age, muscle weakness, and poor conditioning can increase the risk of sustaining a muscle injury.
Consequences of Untreated Muscle Injuries
Failure to address muscle injuries promptly can have significant consequences, ranging from prolonged pain and disability to irreversible tissue damage. Chronic muscle injuries may lead to scar tissue formation, decreased muscle strength, and impaired range of motion, ultimately affecting an individual’s ability to perform daily activities and participate in physical exercise.
Traditional Treatment Approaches
RICE Method (Rest, Ice, Compression, Elevation)
The RICE method, consisting of rest, ice, compression, and elevation, has long been employed as a first-line treatment for acute muscle injuries. This approach aims to reduce pain and inflammation, promote tissue healing, and prevent further damage. While effective in many cases, the RICE method may not always suffice for more severe or chronic injuries, necessitating additional interventions.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play a crucial role in the recovery process following a muscle injury. Through targeted exercises, stretching, and manual techniques, physical therapists help restore strength, flexibility, and function to the injured muscle. Rehabilitation programs are tailored to each individual’s specific needs and may involve gradual progression from passive to active exercises.
Surgical Interventions (Repair and Reconstruction)
In cases of severe muscle injuries or failure to respond to conservative treatments, surgical intervention may be necessary. Surgical procedures such as muscle repair and reconstruction aim to restore the integrity of the muscle tissue and optimize functional outcomes. These interventions are often reserved for complex injuries or situations where conservative measures have proven ineffective.
The Promise of Stem Cell Therapy
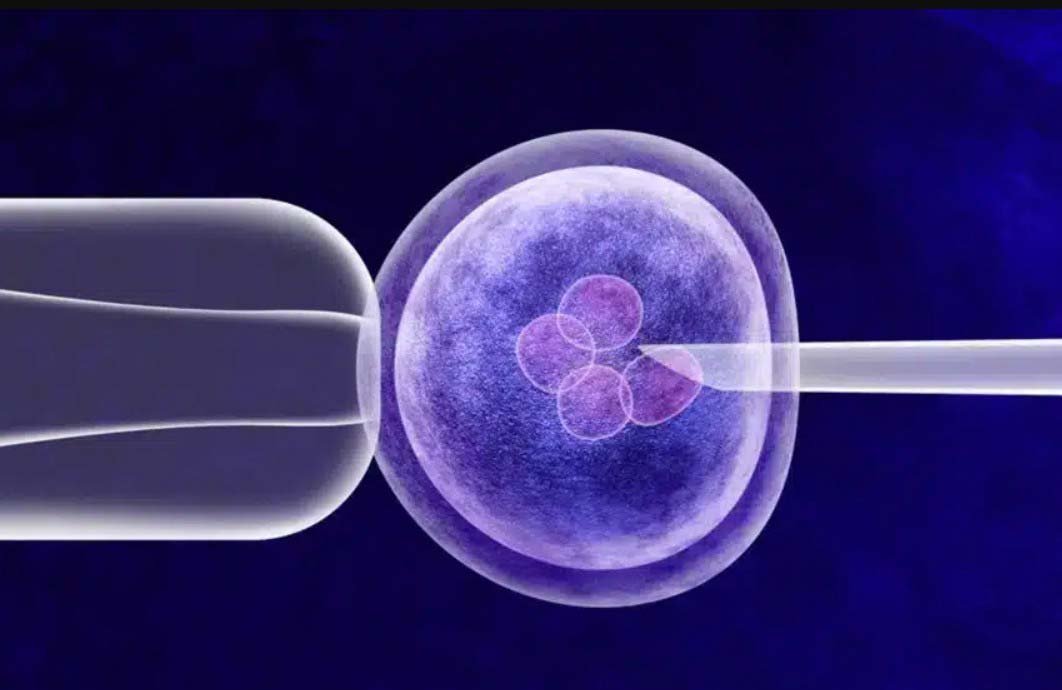
Definition and Types of Stem Cells
Stem cells are undifferentiated cells capable of self-renewal and differentiation into specialized cell types. They can be broadly categorized into embryonic stem cells (ESCs), adult stem cells, and induced pluripotent stem cells (iPSCs), each with its own unique characteristics and applications.
Mechanisms of Action in Muscle Repair
Stem cells exert their therapeutic effects through various mechanisms, including differentiation into muscle cells, secretion of growth factors and cytokines, and modulation of the immune response. By promoting tissue regeneration and reducing inflammation, stem cell therapy offers a novel approach to enhancing muscle repair and recovery.
Advantages Over Traditional Treatments
Compared to traditional treatment approaches, stem cell therapy offers several distinct advantages. These include the ability to target the underlying mechanisms of tissue damage, promote natural healing processes, and potentially regenerate lost or damaged muscle tissue. Additionally, stem cell therapy may reduce the need for invasive procedures and mitigate the risk of complications associated with surgery.
Types of Stem Cells Used in Muscle Injury Recovery
Several types of stem cells have shown promise in the treatment of muscle injuries, including embryonic stem cells, adult stem cells (such as mesenchymal stem cells and satellite cells), and induced pluripotent stem cells. Each type of stem cell offers unique advantages and may be selected based on the specific requirements of the patient and the nature of the injury.
Application of Stem Cell Therapy in Muscle Injury Recovery
Preclinical Studies and Animal Models
Preclinical studies using animal models have provided valuable insights into the therapeutic potential of stem cell therapy for muscle injuries. These studies have demonstrated the ability of stem cells to enhance muscle regeneration, improve functional outcomes, and reduce scar tissue formation. Moreover, they have helped elucidate the optimal delivery methods and dosing regimens for translating stem cell therapies to clinical practice.
Clinical Trials and Human Studies
Clinical trials evaluating the safety and efficacy of stem cell therapy for muscle injuries have shown promising results. These studies have demonstrated improvements in pain, muscle strength, and functional capacity following stem cell treatment. While further research is needed to validate these findings and establish standardized protocols, early clinical data support the potential of stem cell therapy as a viable treatment option for muscle injuries.
Efficacy and Safety Considerations
The efficacy and safety of stem cell therapy for muscle injuries depend on various factors, including the type of stem cells used, the mode of delivery, and the characteristics of the injury. While stem cell therapy holds great promise, concerns remain regarding its long-term safety, including the risk of immune rejection, tumorigenicity, and ectopic tissue formation. Addressing these concerns through rigorous preclinical and clinical testing is essential for ensuring the responsible translation of stem cell therapies into clinical practice.
Optimizing Stem Cell Therapy for Muscle Injury Recovery
Delivery Methods (Injection, Implantation, Scaffold-Based)
The choice of delivery method is critical for maximizing the therapeutic efficacy of stem cell therapy. Injection-based approaches, such as direct intramuscular injection or intra-arterial infusion, offer a minimally invasive and targeted delivery route. Implantation techniques involve the placement of stem cells within a biocompatible scaffold, providing structural support and promoting tissue integration. Scaffold-based approaches offer the advantage of prolonged stem cell retention and controlled release of bioactive factors, thereby enhancing the regenerative potential of stem cells.
Dosage and Timing Considerations
Optimizing the dosage and timing of stem cell therapy is essential for achieving optimal outcomes. Dosage optimization involves determining the appropriate number of stem cells to administer based on factors such as the extent of the injury and the patient’s individual characteristics. Timing considerations revolve around identifying the optimal window of opportunity for initiating stem cell therapy to maximize its efficacy and promote timely tissue repair.
Combining Stem Cell Therapy with Other Modalities
Combining stem cell therapy with complementary modalities, such as growth factors, biomaterials, and physical therapy, may enhance its therapeutic effects. Synergistic approaches that target multiple aspects of the injury cascade, including inflammation, angiogenesis, and tissue remodeling, have the potential to accelerate healing and improve functional outcomes. Additionally, personalized treatment regimens tailored to each patient’s unique needs may further optimize the efficacy of stem cell therapy.
Challenges and Limitations
Immune Response and Rejection
One of the primary challenges associated with stem cell therapy is the risk of immune rejection, particularly in allogeneic transplantation settings. Host immune responses may recognize transplanted stem cells as foreign entities, leading to immune-mediated rejection and compromised therapeutic efficacy. Strategies to mitigate immune rejection, such as immunosuppressive therapy and the use of autologous stem cells, are actively being investigated to improve the safety and long-term viability of stem cell-based therapies.
Tumorigenicity and Cell Stability
Another concern with stem cell therapy is the potential risk of tumorigenicity and aberrant cell behavior. Pluripotent stem cells, in particular, possess the capacity for uncontrolled proliferation and differentiation, raising safety concerns regarding their use in clinical applications. Strategies to enhance the stability and lineage commitment of stem cells, such as genetic modification and preconditioning, are being explored to minimize the risk of tumorigenicity and ensure the controlled differentiation of transplanted cells.
Regulatory Hurdles and Ethical Concerns
The translation of stem cell therapies from the laboratory to the clinic is hindered by regulatory hurdles and ethical considerations. Regulatory agencies play a critical role in evaluating the safety and efficacy of stem cell-based treatments and ensuring compliance with established guidelines and standards. Ethical concerns surrounding the use of embryonic stem cells and the informed consent process further complicate the development and implementation of stem cell therapies for muscle injuries.
Future Directions and Emerging Technologies
Gene Editing and Genetic Modification
Advancements in gene editing technologies, such as CRISPR-Cas9, offer exciting possibilities for enhancing the therapeutic potential of stem cells. By precisely modifying the genetic profile of stem cells, researchers can optimize their function, improve their survival, and mitigate potential safety concerns. Gene-edited stem cells hold promise for personalized medicine approaches tailored to individual patient needs and genetic predispositions.
Biomaterials and Tissue Engineering
The integration of stem cells with biomaterials and tissue engineering scaffolds represents a promising strategy for enhancing their regenerative capacity. Biomaterials provide a supportive microenvironment for stem cell growth, differentiation, and tissue integration, while tissue engineering approaches enable the fabrication of complex three-dimensional structures mimicking native tissue architecture. Combining stem cells with biomaterials offers a synergistic approach for promoting tissue regeneration and functional recovery in muscle injuries.
Personalized Medicine Approaches
Advances in personalized medicine and regenerative therapies are revolutionizing the treatment of musculoskeletal injuries. By tailoring treatment regimens to each patient’s unique physiological and genetic characteristics, clinicians can optimize therapeutic outcomes and minimize the risk of adverse events. Personalized approaches encompass a range of modalities, including stem cell therapy, gene therapy, and precision medicine, with the potential to transform the landscape of musculoskeletal care.
Case Studies and Success Stories
Notable Examples of Muscle Injury Recovery with Stem Cell Therapy
Several case studies and success stories highlight the potential of stem cell therapy for promoting muscle injury recovery. From professional athletes returning to peak performance following stem cell treatment to individuals regaining function and mobility after debilitating injuries, these examples underscore the transformative impact of regenerative medicine on patient outcomes. While further research is needed to validate these findings and elucidate the underlying mechanisms of action, these success stories offer hope for individuals grappling with muscle injuries.
Long-term Outcomes and Patient Satisfaction
Assessing the long-term outcomes and patient satisfaction associated with stem cell therapy is essential for evaluating its efficacy and informing clinical practice. Longitudinal studies tracking patients over extended periods can provide valuable insights into the durability of treatment effects, the incidence of complications, and the overall quality of life following stem cell therapy. Additionally, patient-reported outcomes and satisfaction surveys offer valuable feedback for optimizing treatment protocols and addressing unmet needs in muscle injury management.
Cost-Benefit Analysis and Economic Considerations
Comparing the cost-effectiveness of stem cell therapy to traditional treatments is essential for informing healthcare decision-making and resource allocation. While stem cell therapy may entail higher upfront costs, its potential to reduce long-term healthcare expenditures by preventing chronic disability and minimizing the need for repeat interventions warrants consideration. Cost-benefit analyses accounting for direct medical costs, indirect costs (e.g., lost productivity), and quality-adjusted life years (QALYs) can help quantify the economic value of stem cell therapy in the context of muscle injury recovery.
Impact on Healthcare Expenditure and Resource Allocation
The widespread adoption of stem cell therapy for muscle injury recovery has implications for healthcare expenditure and resource allocation. While stem cell therapy holds promise for improving patient outcomes and reducing the burden of chronic musculoskeletal conditions, its implementation requires careful consideration of cost-effectiveness, reimbursement policies, and infrastructure requirements. Allocating resources judiciously to support research, innovation, and clinical implementation is essential for maximizing the societal benefits of stem cell therapy while ensuring equitable access for all patients.
Health Economics of Preventing Chronic Muscle Injuries
Preventing chronic muscle injuries through early intervention and effective treatment strategies has significant health economic implications. By reducing the incidence of debilitating conditions and minimizing the need for costly interventions, proactive management of muscle injuries can yield substantial savings in healthcare expenditures and productivity losses. Investing in preventive measures, such as education, training, and injury prevention programs, can yield substantial returns on investment and promote population-wide musculoskeletal health.
Ethical and Legal Implications
Informed Consent and Patient Rights
Respecting patient autonomy and ensuring informed consent are paramount in the ethical practice of stem cell therapy. Patients must be provided with comprehensive information regarding the risks, benefits, and alternatives to treatment, allowing them to make well-informed decisions about their care. Informed consent processes should be transparent, culturally sensitive, and tailored to the individual needs and preferences of each patient, empowering them to actively participate in their healthcare decisions.
Regulatory Frameworks and Oversight
Regulatory frameworks play a crucial role in ensuring the safety, efficacy, and ethical conduct of stem cell-based therapies. Regulatory agencies such as the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) oversee the approval and oversight of stem cell products, establishing rigorous standards for preclinical testing, clinical trials, and manufacturing practices. Compliance with regulatory requirements is essential for securing approval for clinical use and safeguarding patient welfare.
Intellectual Property and Commercialization Issues
The commercialization of stem cell therapies raises complex ethical and legal considerations surrounding intellectual property rights, access to healthcare, and equity in innovation. Balancing the interests of patients, researchers, and industry stakeholders requires transparent and equitable frameworks for intellectual property protection, licensing, and technology transfer. Furthermore, efforts to promote open science, collaboration, and knowledge sharing are essential for fostering innovation and maximizing the societal impact of stem cell research.
Patient Education and Public Awareness
Educating patients and the public about stem cell therapy is essential for fostering informed decision-making and dispelling misconceptions. Healthcare providers play a central role in educating patients about the potential benefits, risks, and limitations of stem cell therapy, guiding them towards evidence-based treatment options. Public awareness campaigns, educational resources, and community outreach initiatives can help demystify stem cell research and promote a deeper understanding of its potential applications in muscle injury recovery.
Conclusion and Recommendations
Stem cell therapy represents a promising approach to muscle injury recovery, offering the potential to enhance healing, restore function, and improve patient outcomes. While significant progress has been made in understanding the mechanisms of action and clinical applications of stem cell therapy, challenges remain in optimizing its efficacy, ensuring safety, and navigating ethical and regulatory considerations. Moving forward, continued research, collaboration, and innovation are essential for realizing the full potential of stem cell therapy and advancing the field of regenerative medicine.
Summary of Key Findings
- Muscle injuries are common and can have significant consequences if left untreated.
- Traditional treatment methods may not always suffice, necessitating the exploration of alternative approaches such as stem cell therapy.
- Stem cells offer unique regenerative capabilities and hold promise for accelerating muscle repair and recovery.
- Preclinical and clinical studies have demonstrated the safety and efficacy of stem cell therapy for muscle injuries, but challenges remain in optimizing treatment protocols and addressing regulatory concerns.
- Personalized medicine approaches, emerging technologies, and interdisciplinary collaboration are shaping the future of muscle injury management.
Implications for Clinical Practice and Research
- Healthcare providers should stay abreast of developments in stem cell therapy and consider its potential role in the management of muscle injuries.
- Researchers should continue to investigate the mechanisms of action and optimal delivery methods for stem cell therapy, with an emphasis on safety, efficacy, and long-term outcomes.
- Regulatory agencies should establish clear guidelines and oversight mechanisms to ensure the responsible translation of stem cell therapies into clinical practice.
- Patient education and advocacy efforts are essential for promoting awareness, understanding, and acceptance of stem cell therapy as a viable treatment option for muscle injuries.
Recommendations for Future Implementation and Policy Development
- Foster interdisciplinary collaboration and knowledge exchange to accelerate advancements in stem cell therapy for muscle injury recovery.
- Invest in research infrastructure, training programs, and clinical trials to further elucidate the safety and efficacy of stem cell-based treatments.
- Develop evidence-based guidelines and regulatory frameworks to govern the ethical and responsible use of stem cell therapies in clinical practice.
- Prioritize patient-centered care, informed consent, and equitable access to stem cell therapy to ensure that all individuals benefit from advances in regenerative medicine.
Stem cell therapy holds great promise as a novel and promising approach to muscle injury recovery. By harnessing the regenerative potential of stem cells, researchers and clinicians are poised to revolutionize the management of muscle injuries and improve the lives of countless individuals worldwide. Through continued research, collaboration, and innovation, we can unlock the full potential of stem cell therapy and usher in a new era of personalized medicine and regenerative healthcare.