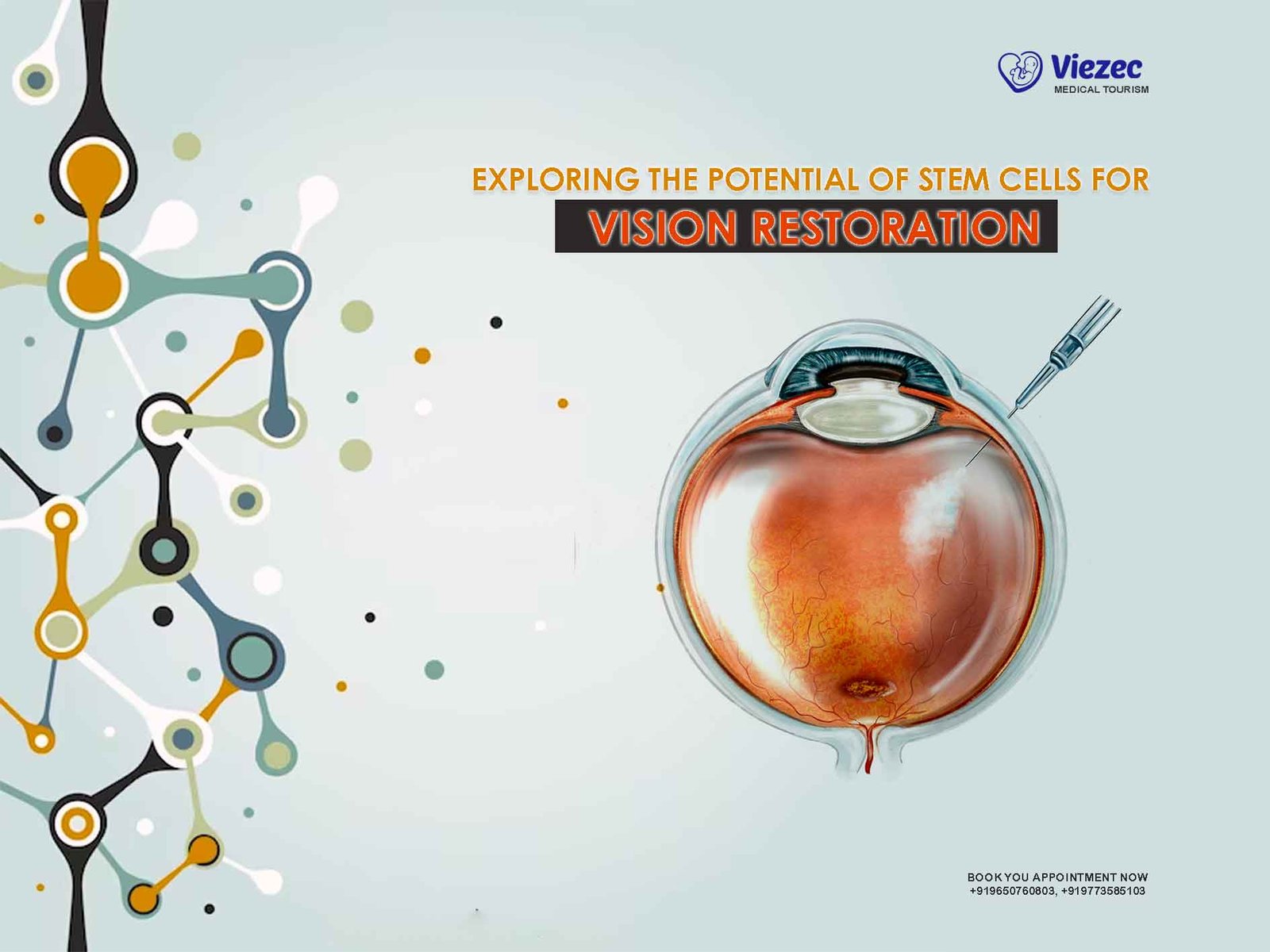
In recent years, stem cell research has emerged as a promising avenue for treating a wide range of medical conditions, including those affecting the eyes and vision. One area where stem cells hold significant potential is in vision restoration. From retinal degenerative diseases like age-related macular degeneration (AMD) to optic nerve damage caused by glaucoma or injury, stem cell therapies offer hope for restoring sight to millions worldwide. This article delves into the current state of stem cell research in vision restoration, exploring its potential, challenges, and future directions.
Understanding Stem Cells
What Are Stem Cells?
Stem cells are unique cells with the remarkable ability to differentiate into various specialized cell types. They serve as the body’s natural repair system, replenishing damaged tissues and organs throughout life. Stem cells can be broadly categorized into two types: embryonic stem cells (ESCs) and adult stem cells.
Embryonic Stem Cells (ESCs)
ESCs are derived from the inner cell mass of early-stage embryos. They have the capacity to differentiate into any cell type in the body, making them particularly valuable for regenerative medicine research. However, their use is ethically contentious due to the destruction of human embryos involved in their extraction.
Adult Stem Cells
Adult stem cells, also known as somatic or tissue-specific stem cells, are found in various tissues and organs throughout the body. Unlike ESCs, adult stem cells are multipotent or pluripotent, meaning they can differentiate into a limited range of cell types. While they are less versatile than ESCs, adult stem cells offer the advantage of being readily accessible from tissues such as bone marrow, adipose tissue, and the eye itself.
Induced Pluripotent Stem Cells (iPSCs)
In 2006, researchers made a groundbreaking discovery by reprogramming adult cells, such as skin cells, to revert to a pluripotent state, similar to ESCs. These reprogrammed cells, known as induced pluripotent stem cells (iPSCs), share many characteristics with ESCs but avoid the ethical concerns associated with embryonic tissue. iPSCs have since become a cornerstone of regenerative medicine research, offering a potentially limitless source of patient-specific stem cells for therapeutic applications.
Stem Cell Therapy for Vision Restoration
Retinal Degenerative Diseases
Retinal degenerative diseases, including AMD, retinitis pigmentosa (RP), and Stargardt disease, are leading causes of irreversible vision loss worldwide. These conditions primarily affect the light-sensitive photoreceptor cells in the retina, leading to progressive vision impairment and, in severe cases, blindness. Traditional treatments for retinal degeneration, such as anti-VEGF injections for AMD or retinal prostheses, aim to slow disease progression or provide artificial vision but do not restore lost vision.
Photoreceptor Replacement
One promising approach for treating retinal degenerative diseases is the transplantation of stem cell-derived photoreceptor cells to replace those lost due to disease. Researchers have demonstrated the feasibility of generating photoreceptor-like cells from both ESCs and iPSCs in vitro, capable of integrating into the host retina and restoring visual function in animal models.
Challenges and Considerations
However, several challenges must be addressed before photoreceptor replacement therapy can be translated into clinical practice. These include optimizing cell survival and integration, ensuring long-term functionality, and minimizing immune rejection. Additionally, the complex structure of the retina poses challenges for precise cell targeting and connectivity within the visual circuitry.
Optic Nerve Regeneration
Damage to the optic nerve, whether from trauma, glaucoma, or other causes, can result in permanent vision loss due to the inability of retinal ganglion cells (RGCs) to regenerate axons and reconnect with their targets in the brain. Stem cell-based approaches aimed at promoting optic nerve regeneration offer hope for restoring visual function in such cases.
RGC Replacement
One strategy involves transplanting stem cell-derived RGCs or progenitor cells into the damaged optic nerve to replace lost or damaged RGCs. Studies in animal models have shown encouraging results, with transplanted cells surviving, extending axons, and forming functional connections with downstream targets in the visual pathway.
Overcoming Challenges
To realize the potential of RGC replacement therapy in humans, researchers must overcome several hurdles, including enhancing cell survival and integration, promoting axonal growth and guidance, and optimizing the functional integration of transplanted cells within the existing neural circuitry. Additionally, strategies to modulate the immune response and prevent graft rejection are critical for long-term success.
Corneal Regeneration
The cornea plays a crucial role in focusing light onto the retina and maintaining ocular transparency. Damage to the cornea, whether from injury, infection, or disease, can result in vision impairment or loss. While traditional treatments such as corneal transplantation have been effective in restoring vision, they are limited by donor tissue availability and the risk of rejection. Stem cell-based approaches offer a promising alternative for corneal regeneration.
Limbal Stem Cell Therapy
The limbus, located at the junction between the cornea and the sclera, harbors a population of stem cells responsible for maintaining corneal epithelial integrity and regeneration. In cases of limbal stem cell deficiency (LSCD), where these stem cells are depleted or dysfunctional, corneal epithelial regeneration is impaired, leading to chronic inflammation, scarring, and vision loss. Stem cell-based therapies aimed at replenishing the limbal stem cell pool offer a potential solution for treating LSCD and restoring corneal transparency.
Clinical Applications
Several approaches to limbal stem cell therapy have been investigated, including autologous limbal stem cell transplantation, ex vivo expansion of limbal epithelial cells, and transplantation of tissue-engineered constructs containing limbal stem cells. These strategies have shown promising results in restoring corneal epithelial function and improving visual outcomes in patients with LSCD, highlighting the potential of stem cells in corneal regeneration.
Challenges and Considerations
Safety and Efficacy
While stem cell therapies hold great promise for vision restoration, safety and efficacy remain paramount concerns. The potential risks associated with stem cell transplantation, such as tumor formation, immune rejection, and off-target effects, must be carefully evaluated in preclinical studies and clinical trials. Additionally, long-term follow-up is essential to monitor for any adverse effects and assess the durability of treatment outcomes.
Immune Rejection
The immune system plays a critical role in recognizing and eliminating foreign cells, tissues, or organs, posing a significant challenge to the success of stem cell-based therapies. Strategies to minimize immune rejection, such as immunosuppressive drugs, cell encapsulation, or genetic engineering of stem cells to evade immune detection, are actively being explored. However, achieving immune tolerance while preserving therapeutic efficacy remains a complex and ongoing area of research.
Ethical and Regulatory Considerations
The ethical and regulatory landscape surrounding stem cell research and therapy is complex and varies across different jurisdictions. Concerns about the source of stem cells, informed consent, patient safety, and equitable access to emerging therapies must be carefully addressed to ensure ethical conduct and regulatory compliance. Collaborative efforts between researchers, clinicians, policymakers, and regulatory agencies are essential to navigate these ethical and legal challenges responsibly.
Future Directions
Despite the challenges and uncertainties, the field of stem cell-based vision restoration continues to advance rapidly, driven by ongoing research efforts and technological innovations. Future directions for stem cell therapy in vision restoration include:
Enhanced Cell Engineering
Advances in cell engineering techniques, such as CRISPR-Cas9 gene editing, allow for precise modification of stem cells to improve their survival, integration, and functionality within the host tissue. Engineering stem cells to express neuroprotective factors, promote axonal regeneration, or evade immune detection holds promise for enhancing the efficacy and safety of stem cell-based therapies for vision restoration.
Biomaterial-Based Approaches
Biomaterials play a crucial role in supporting stem cell survival, proliferation, and differentiation in vivo. Scaffold-based approaches, such as hydrogels, microfabricated substrates, and decellularized matrices, offer a platform for delivering stem cells to the target tissue, providing structural support, and facilitating tissue regeneration. Incorporating bioactive cues and signaling molecules into biomaterials further enhances their regenerative potential for vision restoration applications.
Patient-Specific Therapies
The advent of iPSC technology enables the generation of patient-specific stem cells, allowing for personalized therapies tailored to individual genetic backgrounds and disease profiles. Patient-derived iPSCs offer a limitless supply of autologous cells for transplantation, minimizing the risk of immune rejection and optimizing treatment outcomes. Integrating iPSC-based approaches with advanced imaging modalities and computational modeling holds promise for precision medicine in vision restoration.
Stem cell therapy holds immense promise for vision restoration, offering hope for millions of individuals affected by sight-threatening conditions worldwide. From retinal degenerative diseases to optic nerve damage and corneal disorders, stem cells offer a versatile platform for regenerating damaged tissues and restoring visual function. While significant challenges remain to be addressed, ongoing research efforts and technological innovations continue to propel the field forward, bringing us closer to realizing the full potential of stem cells in restoring sight and improving quality of life for patients with vision impairment.