Type 1 diabetes is a chronic autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas. Unlike type 2 diabetes, which is often associated with lifestyle factors, type 1 diabetes typically develops early in life and requires lifelong insulin therapy for management.
Mechanisms of Autoimmunity in Type 1 Diabetes
The exact cause of type 1 diabetes is still not fully understood, but it is believed to involve a complex interplay of genetic predisposition and environmental triggers. In individuals with a genetic susceptibility, exposure to certain environmental factors, such as viral infections or dietary factors, may initiate an autoimmune response against the insulin-producing beta cells.
Current Treatment Challenges
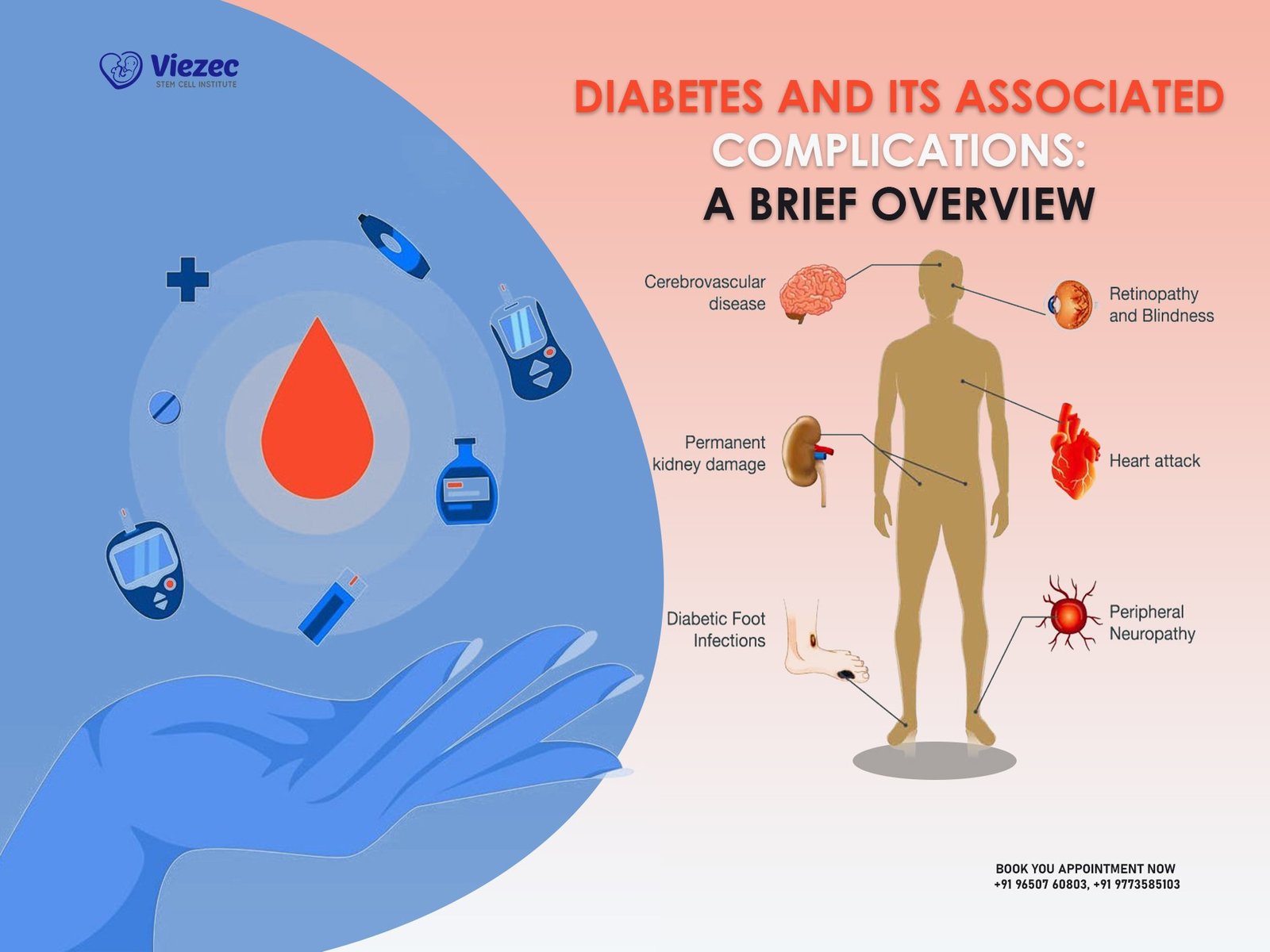
Despite significant advances in diabetes management, individuals with type 1 diabetes still face numerous challenges. Insulin therapy, while life-saving, is not a cure and requires meticulous monitoring of blood glucose levels to prevent complications such as hypoglycemia and hyperglycemia. Moreover, the long-term complications of diabetes, including cardiovascular disease, kidney failure, and nerve damage, continue to pose significant health risks.
Emerging Therapeutic Strategies
Breakthroughs in Immunomodulation
Recent advances in immunomodulation have offered new hope for the treatment of type 1 diabetes. Therapies aimed at modulating the immune system to prevent the destruction of beta cells or induce immune tolerance hold promise for preserving insulin production and potentially halting the progression of the disease.
Harnessing the Power of Stem Cells
Stem cell therapy represents a cutting-edge approach to diabetes treatment by replenishing the insulin-producing beta cells that are destroyed in type 1 diabetes. By harnessing the regenerative capacity of stem cells, researchers aim to restore normal insulin production and provide a long-term solution for individuals with the condition.
Gene Therapy Advancements
Gene therapy holds immense potential for treating type 1 diabetes by targeting the underlying genetic defects that contribute to the development of the disease. By delivering therapeutic genes to the pancreas or modifying immune cells to prevent the destruction of beta cells, gene therapy offers a targeted and personalized approach to diabetes treatment.
Stem Cell Treatment: A Promising Frontier
Introduction to Stem Cell Therapy
Stem cell therapy involves the transplantation of stem cells into the body to replace damaged or dysfunctional cells and restore normal function. In the context of type 1 diabetes, stem cell therapy holds promise for replenishing the insulin-producing beta cells that are destroyed by the immune system.
Types of Stem Cells Used in Diabetes Treatment
Several types of stem cells have been explored for diabetes treatment, including embryonic stem cells, induced pluripotent stem cells, and adult stem cells derived from various sources such as the bone marrow or umbilical cord blood. Each type of stem cell has its unique advantages and limitations, and ongoing research aims to optimize their therapeutic potential.
Clinical Applications and Research Findings
Clinical trials investigating the safety and efficacy of stem cell therapy for type 1 diabetes have shown promising results. Transplantation of insulin-producing cells derived from stem cells has been shown to improve glycemic control and reduce the need for exogenous insulin in some patients. However, challenges such as immune rejection and the scalability of cell production remain significant hurdles to overcome.
Bioengineering Solutions
Artificial Pancreas Technology
Artificial pancreas technology represents a revolutionary approach to diabetes management by integrating continuous glucose monitoring with automated insulin delivery systems. By mimicking the function of the pancreas, artificial pancreas devices can regulate blood glucose levels more effectively and reduce the burden of diabetes self-management.
Nanotechnology Innovations in Diabetes Management
Nanotechnology holds promise for revolutionizing diabetes care through the development of novel drug delivery systems, glucose-sensing technologies, and targeted therapies. By leveraging the unique properties of nanomaterials, researchers aim to enhance the precision and efficacy of diabetes treatments while minimizing side effects.
Biomaterials for Islet Cell Encapsulation
Islet cell encapsulation involves the encapsulation of insulin-producing cells within biocompatible materials to protect them from immune attack while allowing for the exchange of nutrients and insulin. This approach offers a potential solution to the immune rejection that has limited the success of traditional islet cell transplantation and holds promise for long-term insulin independence in individuals with type 1 diabetes.
Precision Medicine Approaches
Personalized Immunotherapy for Type 1 Diabetes
Personalized immunotherapy involves tailoring treatment strategies based on the individual’s immune profile and genetic makeup. By identifying specific immune targets and developing personalized immunomodulatory therapies, researchers aim to achieve better outcomes and reduce the risk of adverse reactions in patients with type 1 diabetes.
Pharmacogenomics in Diabetes Treatment
Pharmacogenomics, the study of how genetic variations influence drug response, holds promise for optimizing diabetes treatment by identifying patients who are most likely to benefit from specific therapies. By incorporating genetic testing into clinical practice, healthcare providers can personalize treatment plans and improve therapeutic outcomes for individuals with type 1 diabetes.
Role of Artificial Intelligence in Treatment Optimization
Artificial intelligence (AI) technologies such as machine learning and predictive analytics offer valuable tools for optimizing diabetes management. By analyzing large datasets and identifying patterns in patient data, AI algorithms can help healthcare providers make more informed decisions and tailor treatment plans to individual needs, ultimately improving patient outcomes and quality of life.
Regulatory Challenges and Ethical Considerations
FDA Regulations on Novel Diabetes Treatments
The Food and Drug Administration (FDA) plays a critical role in regulating the development and approval of novel diabetes treatments. While stringent regulatory oversight is essential for ensuring patient safety and efficacy, the lengthy and costly approval process can pose challenges for bringing innovative therapies to market in a timely manner.
Ethical Issues Surrounding Stem Cell Therapy
Stem cell therapy raises important ethical considerations related to the use of human embryonic stem cells, the informed consent process, and the equitable distribution of resources. Ethical guidelines and regulatory frameworks are needed to ensure that stem cell research and therapy are conducted ethically and responsibly, with due consideration for the rights and welfare of patients.
Patient Advocacy and Policy Implications
Patient advocacy organizations play a crucial role in raising awareness, driving research funding, and influencing healthcare policy decisions related to diabetes care. By advocating for patient-centered approaches, increased research funding, and improved access to care, patient advocacy groups can help address the unmet needs of individuals with type 1 diabetes and drive positive change in healthcare systems.
Clinical Trials and Future Prospects
The landscape of Type 1 Diabetes (T1D) research is continually evolving, with clinical trials playing a pivotal role in advancing our understanding and treatment of the disease. Currently, there are numerous ongoing clinical trials exploring a variety of therapeutic avenues, ranging from immune modulation to beta cell regeneration. These trials offer hope for individuals living with T1D by testing innovative approaches that could potentially lead to a cure or significant improvements in disease management.
Patient-Centric Approaches to Care
Beyond medical interventions, it is increasingly recognized that holistic care is essential for effectively managing T1D. Psychosocial support plays a crucial role in helping individuals cope with the emotional and mental challenges associated with the disease. Additionally, lifestyle interventions and behavioral strategies, such as dietary modifications and exercise regimens, can have a profound impact on glycemic control and overall well-being. Integrative medicine, encompassing practices like acupuncture and mindfulness techniques, is also gaining recognition for its potential benefits in diabetes management.
Global Health Perspectives
While advancements in T1D research offer promise, it is essential to address disparities in access to care, both within and across nations. In low-resource settings, where healthcare infrastructure may be limited, innovative solutions are needed to ensure that all individuals with T1D receive adequate treatment and support. International collaborations play a crucial role in sharing knowledge and resources to tackle the global burden of T1D. However, challenges persist, including funding constraints and regulatory hurdles, underscoring the need for sustained efforts to improve diabetes care on a global scale.
Educational Initiatives and Public Awareness
Education is a cornerstone of effective diabetes management, empowering patients and their families to make informed decisions about their health. Diabetes education programs provide valuable information on topics such as blood glucose monitoring, insulin administration, and dietary management. Advocacy efforts are also instrumental in raising awareness about the challenges faced by individuals with T1D and advocating for policy changes to improve access to care. Media campaigns and community outreach initiatives further contribute to destigmatizing the disease and fostering a supportive environment for those affected by T1D.
Economic Implications and Healthcare Systems
The economic burden of T1D extends beyond the individual level to impact healthcare systems and society as a whole. Novel diabetes therapies, while offering potential benefits in terms of improved health outcomes, must also be evaluated for their cost-effectiveness. Health economics research plays a vital role in assessing the long-term economic implications of T1D management strategies and informing policy decisions. Sustainable healthcare systems are essential for ensuring that individuals with T1D have access to quality care without imposing undue financial strain on patients or healthcare providers.
Concluding Remarks and Call to Action
In conclusion, transformative approaches to T1D care offer hope for a future where individuals living with the disease can lead healthier, more fulfilling lives. Multidisciplinary collaboration, encompassing healthcare professionals, researchers, policymakers, and patient advocacy groups, is essential for driving progress in T1D research and treatment. However, there is an urgent need for continued investment in research and innovation to overcome the remaining challenges and ultimately find a cure for T1D.
FAQs:
1. What are some of the most promising therapeutic targets currently being explored in T1D research?
- Promising therapeutic targets in T1D research include immune modulation therapies aimed at preserving beta cell function, regenerative medicine approaches to restore insulin-producing cells, and precision medicine strategies to personalize treatment based on individual genetic and immune profiles.
2. How can individuals living with T1D access psychosocial support and integrative medicine services?
- Many healthcare facilities offer psychosocial support services, such as counseling and support groups, for individuals with T1D and their families. Integrative medicine services may be available through specialized clinics or practitioners trained in complementary and alternative therapies.
3. What role can advocacy efforts play in improving diabetes care on a global scale?
- Advocacy efforts can raise awareness about the social, economic, and political factors that impact access to diabetes care, mobilize resources to support research and treatment initiatives, and influence policy changes to prioritize diabetes prevention and management as public health priorities.