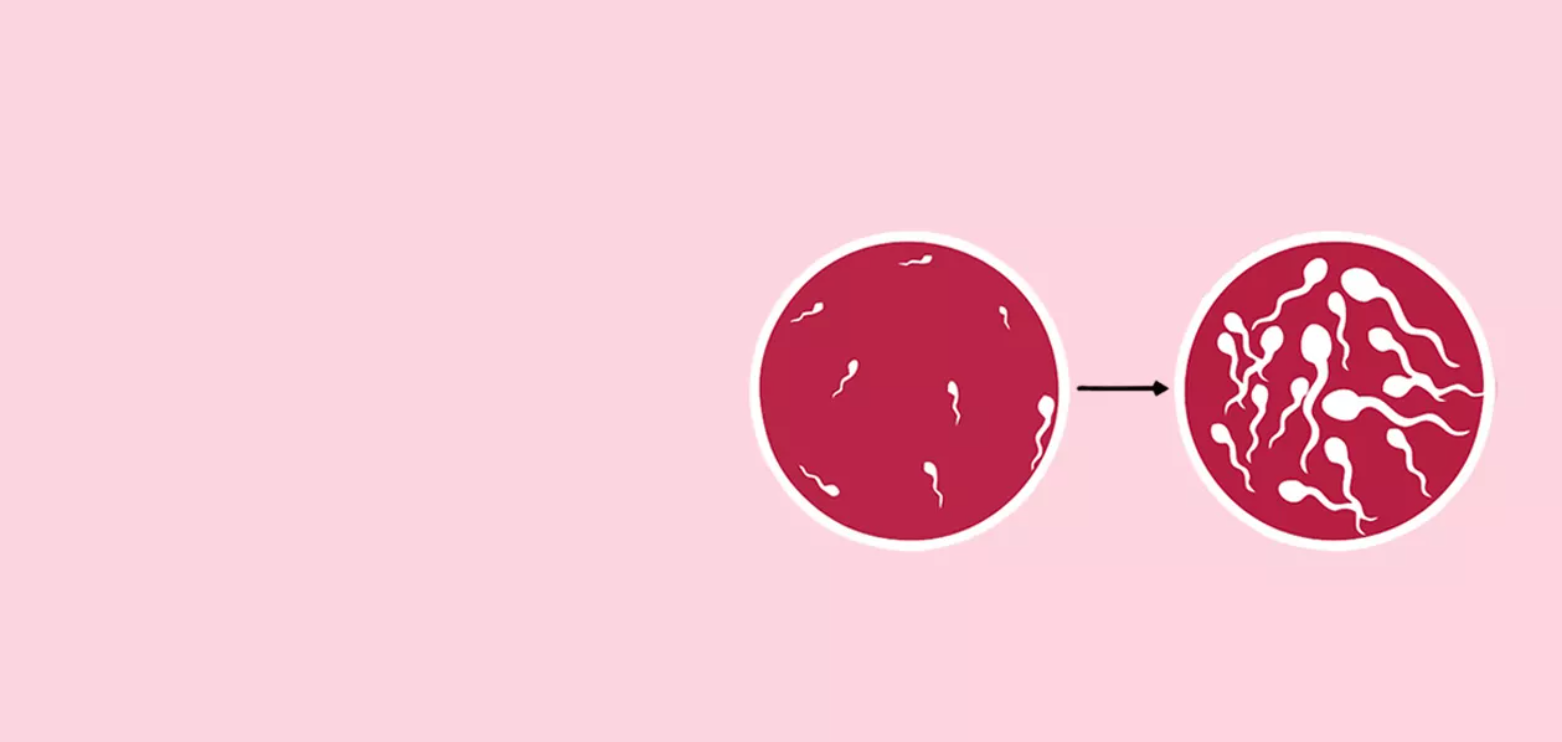
Oligospermia, a condition marked by a low sperm count, is a challenge that affects millions of men around the world, impacting their ability to conceive. While traditional treatments for male infertility often involve medications, lifestyle modifications, or assisted reproductive technologies like In Vitro Fertilization (IVF), there is a promising alternative that is gaining attention: stem cell therapy.
Stem cell therapy for oligospermia is a groundbreaking approach that aims to regenerate sperm production in the testes, offering hope to men who struggle with infertility. Unlike conventional treatments, which may only provide temporary fixes, stem cell therapy addresses the root cause of infertility, potentially restoring natural sperm production and fertility.
In this article, we’ll dive into how stem cell therapy works, its key benefits over traditional treatments, the procedure itself, and the risks and side effects. We’ll also take a look at real-life success stories and examine the future potential of this revolutionary therapy.
Understanding Oligospermia: What It Is and How It Affects Fertility
Oligospermia is a medical condition characterized by a low sperm count, typically defined as having fewer than 15 million sperm per milliliter of semen. This condition can significantly affect a man’s fertility, making it difficult for sperm to successfully fertilize an egg.
While oligospermia can sometimes go unnoticed, it often presents a major obstacle for couples who are trying to conceive. With fewer sperm available, the chances of a successful pregnancy naturally decrease, and fertility treatments may be required.
Causes of Oligospermia: Genetic, Environmental, and Lifestyle Factors
Oligospermia doesn’t stem from a single cause—rather, it results from a variety of genetic, environmental, and lifestyle factors. Understanding these causes is key to addressing the issue effectively:
-
Genetic Factors: Certain genetic disorders, such as Klinefelter syndrome, Y chromosome microdeletions, or cystic fibrosis, can lead to low sperm count. These conditions may affect sperm production or the development of male reproductive organs.
-
Environmental Factors: Exposure to harmful chemicals, pesticides, heavy metals, and radiation can impact sperm quality and count. Environmental toxins can disrupt the hormonal balance required for sperm production and lead to oligospermia.
-
Lifestyle Factors: Unhealthy habits like smoking, excessive alcohol consumption, being overweight, or using recreational drugs (such as anabolic steroids or marijuana) can all significantly reduce sperm count. Stress and poor diet also contribute to poor reproductive health.
Common Symptoms and Diagnosis
Oligospermia typically doesn’t present any obvious symptoms. Most men are unaware of their condition until they experience difficulty in conceiving. If you and your partner are struggling to get pregnant, it’s important to get a semen analysis done.
A semen analysis evaluates sperm count, motility (movement), and morphology (shape). In addition to this test, further examinations, such as hormone level testing, genetic screening, and a testicular biopsy, may be necessary to identify the underlying cause of oligospermia.
The Science Behind Stem Cell Therapy for Male Infertility
Stem cell therapy is an innovative approach that has shown significant promise in addressing the underlying causes of male infertility, particularly in cases of oligospermia. By stimulating the regeneration of sperm cells in the testes, stem cell therapy offers a potential solution for men whose sperm production has been impaired due to various factors.
Unlike conventional treatments, which may focus on external methods like IVF or hormonal therapies, stem cell therapy works at the root of the issue—directly enhancing sperm production by restoring the function of the testes.
How Stem Cells Regenerate Sperm Production
Stem cells have the remarkable ability to differentiate into many types of cells, including sperm cells. When stem cells are introduced into the testes, they can promote the regeneration of spermatogenic cells (the cells responsible for sperm production) that may have been damaged or impaired.
Once these stem cells are injected into the testes, they interact with the surrounding environment and begin to stimulate the growth of new, healthy sperm cells. This process increases sperm count, quality, and motility, leading to improved fertility.
This regenerative process is key to stem cell therapy’s effectiveness. For men suffering from oligospermia, particularly those with testicular dysfunction or damage, stem cell therapy holds the potential to significantly improve sperm production and restore fertility.
Types of Stem Cells Used in Oligospermia Treatment
Several types of stem cells are being studied and used in the treatment of oligospermia, each with its own advantages:
-
Embryonic Stem Cells: These cells, derived from early-stage embryos, are pluripotent, meaning they can develop into any type of cell, including sperm cells. However, the use of embryonic stem cells is often controversial due to ethical concerns.
-
Adult Stem Cells: These are stem cells found in adult tissues, such as bone marrow or fat. Adult stem cells are more commonly used in medical treatments because they do not raise the same ethical issues as embryonic stem cells. They have been shown to be effective in regenerating sperm production in men with oligospermia.
-
Induced Pluripotent Stem Cells (iPSCs): iPSCs are adult cells that have been reprogrammed to behave like embryonic stem cells. This breakthrough technology allows for the creation of pluripotent stem cells without the need for embryos, offering a more ethical and practical solution for stem cell-based treatments.
Each of these stem cell types has been shown to have the potential to regenerate sperm production, but ongoing research continues to refine techniques to maximize the effectiveness of stem cell therapy.
Key Benefits of Stem Cell Therapy Over Conventional Treatments
Stem cell therapy presents several compelling advantages over traditional treatments for oligospermia, making it a revolutionary approach to male infertility. By addressing the root cause of infertility—low sperm production—stem cell therapy provides a more sustainable solution compared to conventional methods like medications or assisted reproductive technologies.
Long-term Success and Reduced Need for Ongoing Treatments
One of the most significant benefits of stem cell therapy is its potential for long-term success. Unlike traditional treatments, which may require ongoing interventions or multiple cycles of IVF, stem cell therapy aims to restore natural sperm production at its core. By regenerating healthy sperm cells in the testes, stem cell therapy could enable a man to achieve sustainable fertility, reducing the need for continuous treatment.
For men whose oligospermia does not respond well to other forms of treatment, stem cell therapy offers a promising alternative that could provide lasting results without the need for regular medical intervention.
Advantages in Sperm Quality and Quantity
In addition to increasing sperm count, stem cell therapy can also improve sperm quality. Many men with oligospermia struggle not only with low sperm count but also with poor sperm motility and abnormal sperm morphology (shape). These factors are crucial for successful fertilization.
Stem cell therapy works by regenerating healthy sperm cells that exhibit better motility and more favorable morphology, which increases the chances of natural conception. This improvement in both quantity and quality of sperm makes stem cell therapy a powerful tool in treating male infertility, offering men a better chance at starting a family.
Who is a Candidate for Stem Cell Therapy for Oligospermia?
Stem cell therapy for oligospermia is not a one-size-fits-all treatment. As with any medical procedure, determining whether a man is a suitable candidate for stem cell therapy requires a thorough evaluation of his overall health, medical history, and the specific causes of his infertility.
Eligibility Criteria for Treatment
Candidates for stem cell therapy are typically men who have:
-
Diagnosed Oligospermia: Men who have a low sperm count, especially those who have not responded well to conventional treatments like medications or hormonal therapies.
-
No Severe Underlying Health Conditions: Stem cell therapy may not be suitable for men with certain genetic disorders, severe testicular damage, or other health issues that may prevent successful treatment. A full medical assessment is necessary to ensure that the treatment is viable.
-
Sufficient Testicular Function: Men who still have viable sperm-producing cells in their testes are more likely to benefit from stem cell therapy. This means that while they may have low sperm count, their testes are still capable of producing sperm with the help of stem cells.
While stem cell therapy has shown promise, it is essential to understand that it may not be effective for all cases of oligospermia, especially in cases where there is significant testicular dysfunction or irreversible damage.
Screening Tests and Medical History Evaluation
Before undergoing stem cell therapy, men must go through a comprehensive screening process. This typically involves:
-
Semen Analysis: To evaluate sperm count, motility, and morphology. This is crucial to assess the severity of the oligospermia and determine if stem cell therapy is a suitable treatment option.
-
Hormone Level Testing: To assess the levels of reproductive hormones like testosterone, FSH (follicle-stimulating hormone), and LH (luteinizing hormone), which play a key role in sperm production.
-
Genetic Testing: To rule out genetic causes of infertility, such as Y chromosome microdeletions, which may affect the ability to produce sperm.
-
Testicular Biopsy: In some cases, a biopsy may be necessary to examine the testicular tissue and evaluate its ability to produce sperm.
The Stem Cell Therapy Procedure for Oligospermia: What to Expect
The stem cell therapy procedure for oligospermia involves a series of carefully planned steps aimed at regenerating sperm production within the testes. While the treatment process can seem complex, understanding each step helps manage expectations and ensures patients are well-prepared.
Step-by-Step Overview of the Treatment Process
Stem cell therapy for oligospermia typically follows these steps:
-
Initial Consultation: The process begins with a thorough consultation, during which the patient’s medical history is reviewed, and tests such as semen analysis, hormone levels, and genetic screenings are performed. This helps assess the severity of oligospermia and determine if the patient is a good candidate for stem cell therapy.
-
Stem Cell Harvesting: Once the patient is deemed a suitable candidate, stem cells are harvested. These stem cells are usually collected from the patient’s own body, often from bone marrow or adipose (fat) tissue. The harvesting process involves a minor surgical procedure, which is typically done under local anesthesia.
-
Stem Cell Injection: After harvesting, the stem cells are processed and injected directly into the testes. This is done in a sterile, controlled environment to ensure the cells are delivered precisely where they are needed. The stem cells begin to interact with the surrounding tissue and stimulate the production of new, healthy sperm cells.
-
Monitoring and Follow-up: Following the injection, patients are closely monitored to assess the success of the procedure. This involves regular follow-ups to check for signs of sperm regeneration. Sperm production improvements may take a few months to show results, as the regeneration process is gradual.
Pre-Treatment Preparation and Considerations
Before undergoing stem cell therapy, patients should take certain steps to ensure the best possible outcome:
-
Avoid Certain Medications: Some medications, particularly those that affect sperm production or immune function, may need to be stopped several weeks before the procedure. Always consult with the doctor regarding medication adjustments.
-
Lifestyle Modifications: Patients are advised to avoid smoking, alcohol, and recreational drugs, as these can negatively impact the success of stem cell therapy. A healthy lifestyle—including a balanced diet and regular exercise—can support the body’s healing and regeneration processes.
-
Comprehensive Health Evaluation: A full medical exam ensures the patient is in good health and ready for the procedure. Conditions like infections or other health issues may need to be addressed beforehand.
Post-Treatment Care and Recovery
After the stem cell injection, recovery is relatively straightforward, but there are a few things to keep in mind:
-
Rest and Recovery: Most patients experience mild discomfort at the injection site, which typically resolves within a few days. Rest is essential, and patients are advised to avoid strenuous activities or heavy lifting for at least a week after the procedure.
-
Gradual Results: Sperm production may take several months to improve. It’s important to remain patient during this process and attend all follow-up appointments to track progress.
-
Follow-Up Testing: After treatment, regular semen analysis and hormone level testing are performed to monitor sperm count, motility, and overall reproductive health. This helps determine the success of the therapy and if additional treatments are needed.
Comparing Stem Cell Therapy with Other Fertility Solutions
Stem cell therapy is an exciting and innovative treatment for oligospermia, but it’s important to compare it with other well-established fertility solutions to understand its advantages and limitations. In this section, we’ll examine how stem cell therapy stacks up against traditional methods like In Vitro Fertilization (IVF) and discuss the key factors that men should consider when choosing the right treatment.
In Vitro Fertilization (IVF) vs. Stem Cell Therapy
IVF is one of the most common and widely accepted fertility treatments for couples facing male infertility. The process involves fertilizing an egg outside the body and then implanting the fertilized embryo into the uterus. For men with low sperm count, IVF often involves using sperm directly from the semen or sperm retrieval from the testes.
However, IVF does not address the root cause of male infertility—low sperm production. While it can be effective in helping a couple conceive, it often requires multiple cycles, which can be costly, time-consuming, and emotionally taxing.
In contrast, stem cell therapy works by stimulating the testes to regenerate sperm production. Unlike IVF, stem cell therapy aims to increase sperm count and improve sperm quality from the inside out. While IVF is more commonly used and well-established, stem cell therapy offers a potential solution for men whose oligospermia has not responded to other treatments.
Effectiveness and Cost Considerations
Stem cell therapy and IVF both have their benefits, but there are key differences in their effectiveness and cost:
-
Effectiveness: Stem cell therapy has shown promising results, particularly for men with severe oligospermia who have not had success with traditional treatments. For some, stem cell therapy can lead to natural sperm regeneration and a better chance of fatherhood. IVF, while effective, depends on external factors like sperm quality, and it may not be suitable for men with very low sperm production or complete azoospermia (lack of sperm).
-
Cost: Stem cell therapy can be expensive, with treatment costs ranging from $5,000 to $10,000, depending on the clinic and location. However, unlike IVF, which may require multiple cycles (each with its own cost), stem cell therapy could potentially provide a one-time solution. This can make stem cell therapy more cost-effective in the long run, especially for men who are looking for a more sustainable and permanent solution.
While both treatments offer unique benefits, it’s important for patients to consult with their healthcare provider to determine the most suitable option based on their individual condition and fertility goals.
Is Stem Cell Therapy the Future of Male Infertility Treatment?
Stem cell therapy for oligospermia is a groundbreaking approach that has the potential to change the landscape of male infertility treatment. By targeting the root cause of infertility—low sperm production—this innovative therapy offers hope for men who have struggled with fertility issues and have not found success with conventional treatments.
Why It’s a Game-Changer for Oligospermia Patients
For many men, stem cell therapy presents a game-changing opportunity to regain their fertility. Unlike traditional treatments like hormone therapy or IVF, which often offer temporary fixes, stem cell therapy aims to provide a long-term solution by regenerating sperm production within the testes. This offers men a chance to naturally conceive and, in some cases, eliminate the need for ongoing medical interventions.
While stem cell therapy is still an emerging field, its potential to address the root causes of oligospermia and restore fertility is incredibly promising. As research continues to advance, the treatment is likely to become even more effective, offering greater success rates and accessibility for men struggling with male infertility.
The future of stem cell therapy in treating oligospermia holds exciting possibilities. With new technologies, refined techniques, and continued clinical research, stem cell therapy could become the go-to treatment for male infertility, revolutionizing how we approach reproductive health and fertility challenges.
Frequently Asked Questions
Q1: Can stem cell therapy treat male infertility?
Yes, stem cell therapy is showing promise in restoring sperm production and improving fertility in men with conditions like azoospermia or oligospermia.
Q2: How do stem cells help with male infertility?
Stem cells can regenerate damaged testicular tissue and promote the formation of new sperm cells.
Q3: Is stem cell therapy effective for low AMH levels?
Preliminary studies suggest stem cell therapy may improve ovarian function and AMH levels in women with diminished ovarian reserve.
Q4: Can stem cells improve fertility in women with low AMH?
Yes, stem cell therapy may enhance egg quality and increase pregnancy chances in women with low AMH.
Q5: What is the cost of stem cell therapy for oligospermia?
In India, the cost typically ranges between ₹2,00,000 and ₹5,00,000 depending on the clinic and treatment approach.
Q6: Does insurance cover stem cell treatment for oligospermia?
Most insurance plans do not cover stem cell therapy as it’s considered experimental or investigational.
Q7: Can stem cell therapy help in non-obstructive azoospermia?
Yes, in some cases, stem cells can stimulate the regeneration of sperm in men with non-obstructive azoospermia.
Q8: What results can I expect from stem cell therapy for azoospermia?
While research is ongoing, some men have reported the return of spermatogenesis and improved sperm counts.
Q9: Is stem cell treatment for azoospermia available in India?
Yes, several advanced clinics in India offer stem cell-based treatments for male infertility, including azoospermia.
Q10: How much does stem cell therapy for azoospermia cost in India?
The cost usually falls between ₹2,50,000 and ₹6,00,000, varying by clinic, protocol, and patient condition.